 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Entry Into Prenatal Care --- United States, 1989--1997Assuring early initiation of prenatal care (PNC) is an important component of safe motherhood programs, which aim to improve maternal and infant health outcomes. Women who receive delayed (i.e., entry into PNC after the first 12 weeks of pregnancy) or no PNC do not receive timely preventive care or education and are at risk for having undetected complications of pregnancy that can result in severe maternal morbidity and sometimes death (1,2). Despite overall improvements, the national health objective for 2000 to increase to at least 90% the proportion of pregnant women who enter PNC during the first trimester of pregnancy (objective 14.11) was not met (3). To increase the proportion of mothers receiving early PNC, Congress authorized the Medicaid expansion program in the mid-1980s, which allowed states to expand Medicaid eligibility criteria to include formerly ineligible pregnant women (4). To examine trends in delayed entry into PNC during 1989--1997 and barriers to obtaining early PNC, CDC analyzed data from two sources. This report summarizes the results of that analysis, which indicated that although more women are obtaining early PNC, racial/ethnic disparities still exist and lack of money or health insurance was not the only barrier to obtaining PNC. CDC analyzed 1989--1997 birth certificate data for all 50 states and the District of Columbia to examine the extent to which women in the United States received delayed PNC or had no PNC. Analysis was restricted to the approximately 4 million live births to U.S. residents each year and for whom data were available on the month of their PNC entry. CDC then used 1997 Pregnancy Risk Assessment Monitoring System (PRAMS) data for 13 states* to assess reasons for delayed PNC or no PNC among women. PRAMS is an ongoing, state-based surveillance system that randomly samples birth certificates and collects information from mothers on pregnancy-related behaviors and experiences. The 20,345 women in the study represented approximately 842,000 women who gave birth to live-born infants in 1997 in the 13 states for which response rates exceeded 70%. SUDAAN was used for analysis, and data were weighted to adjust for survey design, nonresponse, and sampling frame noncoverage. During 1989--1997, the percentage of women with delayed PNC or no PNC decreased from 25% to 18%, with improvement in both delayed PNC (from 22% to 16%) and in no PNC (from 2% to 1%) (Table 1). The decrease in no PNC during 1989--1997 resulted in an estimated 206,000 additional women entering PNC who may not have done so had the 1989 rate remained unchanged. Groups more likely to have delayed or no PNC during 1989--1997 included non-Hispanic blacks, Hispanics, women aged <20 years, women with <12 years of education, and multiparous women. However, those same groups generally had larger absolute improvements in delayed and no PNC during 1989--1997. For example, the prevalence of Hispanic women with delayed or no PNC decreased from 41% to 26%, and for women aged <20 years, from 47% to 32%. Improvements in the percentages of women with no PNC occurred for all racial/ethnic groups during 1989--1995, but then leveled off for non-Hispanic black and non-Hispanic white women (Figure 1). Data from 1997 PRAMS indicated that 56% of women with delayed or no PNC wanted to begin PNC earlier. Reasons for delayed or no PNC varied by racial/ethnic group, age, or method of payment for PNC (Table 2). The most common reason for not receiving care earlier was "I didn't know that I was pregnant" (non-Hispanic black [44%], non-Hispanic white [37%], women aged <20 years [47%], and women whose PNC was paid for by private insurance [44%]). The second most cited barrier to earlier PNC entry was "I didn't have enough money or insurance to pay for my visits" (Hispanics [41%], non-Hispanic whites [36%], women aged 20--24 years [36%], and women whose PNC was paid for by a method other than public or private insurance [36%]). Among women whose PNC was paid for by public assistance (e.g., Medicaid and state programs), 33% cited the latter reason as a barrier to early care. The third most common reason for not receiving early PNC was inability to get an appointment (Hispanics [27%] and women aged >35 years [36%]). Reported by: Statistics and Computer Resources Br, Program Svcs and Development Br, Pregnancy and Infant Health Br, Div of Reproductive Health, National Center for Chronic Disease Prevention and Public Health Promotion; Reproductive Statistics Br, Div of Vital Statistics, National Center for Health Statistics, CDC. Editorial Note:During 1989--1997, the prevalence of delayed or no PNC improved each year among women delivering a live-born infant in the United States. Improvements in access to early PNC may, in part, be attributed to the Medicaid expansion program (5). States responded to this change in the Medicaid regulations by implementing various programs that differed in regards to eligibility criteria and breadth of assistance (6,7). Evaluations of Medicaid expansion programs have shown that as more low-income women become eligible for Medicaid, more of these women accessed early PNC (8). However, as of 1998, no states had achieved the national health objective for 2000 for early PNC. Although the goals emphasized resolving health disparities, only one state had reached these goals for black women and no state had achieved them for Hispanic women (9). In 1997, the percentages of non-Hispanic black women and Hispanic women with delayed or no PNC remained approximately two times that of white women, approximately the same as in 1989. Such continuing disparities in obtaining early PNC mirror the disparities in many reproductive health outcomes among non-Hispanic black and Hispanic women compared with non-Hispanic white women. Although Medicaid expansion has contributed substantially to improving access to early PNC by removing financial barriers for women, a substantial proportion of pregnant women still did not receive PNC during the first trimester. More than half of women with delayed or no PNC would have liked to obtain earlier care, and these women cited various reasons for delayed entry, with these reasons varying by group. The most frequent reasons for delay were not knowing that they were pregnant, lack of money or insurance coverage, and inability to get an appointment earlier. These reasons suggest a need for improved health education, women's health services, and coverage of early PNC services. The findings in this report are subject to at least three limitations. First, the findings examined only one variable at a time and do not account for overlaps between demographic and socioeconomic groups of women (e.g., non-Hispanic black mothers are more likely to be aged <20 years than non-Hispanic white mothers). Second, although the measure used for initiation of care addresses the timing of PNC initiation, it does not account for the frequency, quality, or satisfaction with the PNC received. Finally, despite being representative of all women delivering a live-born infant in their states, PRAMS data are only available for a limited number of states and are not representative of all U.S. births. Early, high-quality PNC is one of the cornerstones of a safe motherhood program, which begins before conception, continues with appropriate PNC and protection from pregnancy complications, and maximizes healthy outcomes for women, infants, and families. Barriers that keep women from entering PNC must be better understood to improve maternal health and to eliminate racial/ethnic disparities in the health outcomes of mothers and infants. Systems such as PRAMS provide the opportunity to understand the reasons women find it difficult to begin PNC early and to monitor changes in access to PNC. Only when timely services are available and accessible to women in their communities can strategies to assure safe motherhood provide the best start for pregnant women and their infants. References
* Alabama, Alaska, Arkansas, Colorado, Florida, Georgia, Maine, North Carolina, New York (excluding New York City), Oklahoma, South Carolina, Washington, and West Virginia. Table 1  Return to top. Figure 1 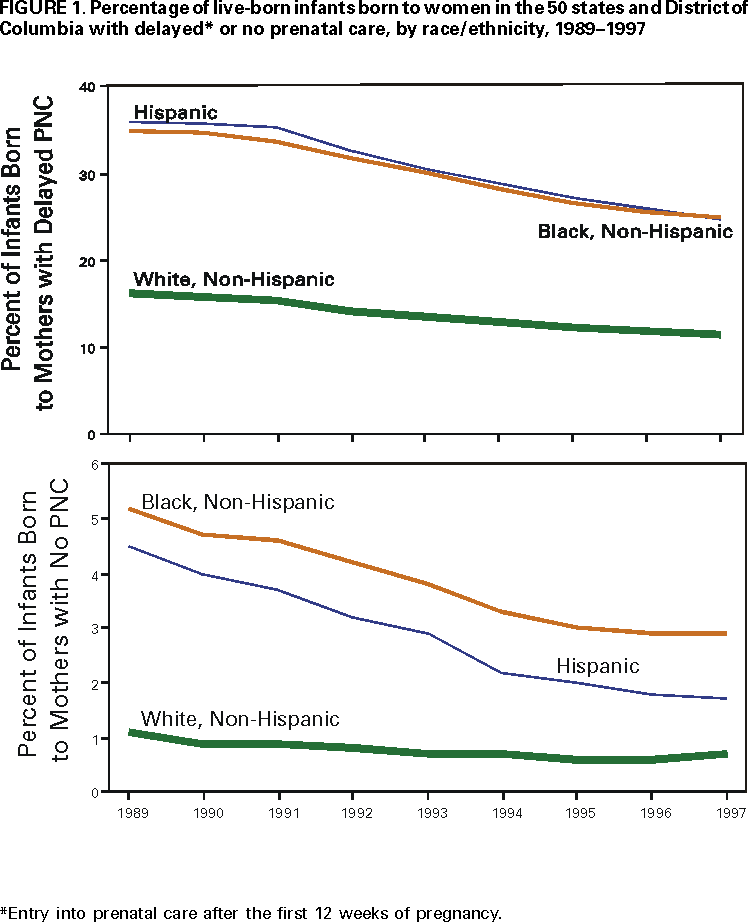 Return to top. Table 2  Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 5/11/2000 |
|||||||||
This page last reviewed 5/2/01
|