US Primary Care Providers’ Experiences and Practices Related to Routine Pediatric Vaccination During the COVID-19 Pandemic
Sean T. O’Leary,1,2 MD, MPH, Jessica Cataldi,1.2 MD, MSCS, Megan C. Lindley,3 MPH, Brenda L. Beaty,1 MSPH, Laura P. Hurley,1,5 MD, MPH, Lori A. Crane,1,4 PhD, MPH, Michaela Brtnikova,1,2 PhD, MPH, Carol Gorman,1 BA, Tara Vogt,3 PhD, Yoonjae Kang,3 MPH, Allison Kempe,1,2 MD, MPH1,2
Affiliations: 1Adult and Child Consortium for Health Outcomes Research and Delivery Science (ACCORDS), University of Colorado School of Medicine and Children’s Hospital Colorado, Aurora, CO; 2Department of Pediatrics, University of Colorado Anschutz Medical Campus, Aurora, CO; 3National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention, Atlanta, GA; 4Department of Community and Behavioral Health, Colorado School of Public Health, Denver, CO, United States, and 5Division of General Internal Medicine, Denver Health, Denver, CO, United States.
Introduction
The World Health Organization declared a global pandemic due to Severe Acute Respiratory Virus Coronavirus-2 (SARS-CoV-2) on March 11, 2020,1 and the United States declared the pandemic a National Emergency on March 13, 2020. Shortly thereafter, stay-at-home and shelter-in-place orders were enacted in much of the United States in an effort to limit the spread of SARS-CoV-2. CDC recommended that outpatient medical providers prioritize urgent visits, delay elective care, and convert clinic visits to telehealth encounters whenever possible.2 While CDC and the American Academy of Pediatrics (AAP) recommended that vaccinations continue to be delivered, many parents and patients were fearful of going into a clinic or assumed, mostly incorrectly, their primary care provider’s office was closed.3 Outpatient pediatric visits fell dramatically in March and April of 2020.3 As a result, childhood vaccination uptake fell dramatically in the same period.4,5 It is unclear the extent to which the decline in vaccination uptake was a result of parent and patient behavior versus the lack of vaccination services from traditional vaccination providers, such as primary care providers. In this report, we describe the experiences and practices of primary care providers related to vaccination during the first several months of the SARS-CoV-2 pandemic. Our specific objectives were to describe, among a nationally representative sample of pediatricians (Peds) and family physicians (FPs), 1) changes made to routine childhood vaccination delivery as a result of the pandemic, and 2) perceived barriers to delivering vaccinations from March 2020 through the time of the survey.
Methods
We conducted surveys among Peds and FPs sentinel networks from October to December 2020. The networks were created using quota sampling and designed to be representative of AAP and American Academy of Family Physicians (AAFP) membership using methodology previously described.6,7 The survey was designed collaboratively with CDC, with input from national physician advisory committees from the two specialties. It was then piloted among 44 physicians. The survey was administered by mail or Internet, based on physician preference. The Colorado Multiple Institutional Review Board approved this study as exempt research.
Results
The response rate was 64% (579/909; Peds 63% [275/439], FPs 65% [304/470]). Overall, respondents (R) were similar to non-respondents (NR) with respect to gender, practice setting (private, public, health maintenance organization, hospital-affiliated), practice location (urban, suburban, rural), and provider age, with minor differences in region of the country (Midwest: R, 25%, NR, 25%; Northeast: R, 19%, NR, 15%; South: R, 33%, NR, 43%; West: R, 23%, NR, 18%; p=0.02).
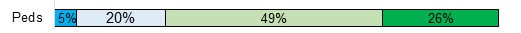
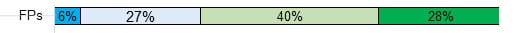
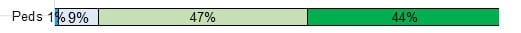
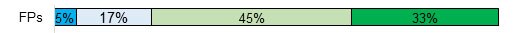
Interruptions in Vaccine Delivery
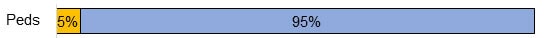
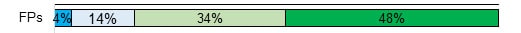
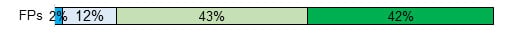
For children aged 0–2 years, 1% of Peds and 23% of FPs reported they were not routinely vaccinating that age group prior to the pandemic. Among those who did vaccinate that age group prior to the pandemic (Peds n=265, FPs n=222), 5% of Peds and 15% of FPs reported they had stopped vaccinating children aged 0–2 years at any time between March 2020 and survey completion (Figure 1). For children aged 4–6 years, 2% of Peds and 20% of FPs reported they were not routinely vaccinating that age group prior to the pandemic. Among those who did vaccinate that age group prior to the pandemic (Peds n=264, FPs n=229), 19% of Peds and 17% of FPs reported they had stopped vaccinating children aged 4–6 years at any time between March 2020 and survey completion. For children aged 11–18 years, 1% of Peds and 13% of FPs reported they were not routinely vaccinating that age group prior to the pandemic. Among those who did vaccinate that age group prior to the pandemic (Peds n=265, FPs n=251), 24% of Peds and 19% of FPs reported they had stopped vaccinating children aged 11–18 years at any time between March 2020 and survey completion.

Children 0-2 years
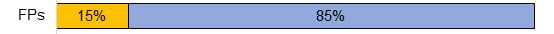
Children 4-6 years


Children 11-18 years
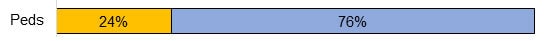
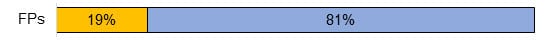
Peds=pediatricians, FPs=family physicians
*Among physicians who reported delivering vaccines prior to the pandemic. Physicians who reported not delivering vaccines prior to the pandemic: for children aged 0–2 years, 1% of Peds and 23% of FPs; for children aged 4–6 years, 2% of Peds and 20% of FPs; for children aged 11–18 years, 1% of Peds and 13% of FPs.
Vaccination Services Delivery at the Time of the Survey
Among all respondents at the time of the survey (October to December 2020), 99% of Peds and 81% of FPs reported providing routine non-influenza vaccines to children aged 0–2 years, 99% of Peds and 82% of FPs to children aged 4–6 years, and 98% of Peds and 89% of FPs to children aged 11–18 years.
Similarly, at the time of the survey, 99% of Peds reported they were providing seasonal influenza vaccine to children aged 0–18 years. For FPs, 83% reported they were providing seasonal influenza vaccine to children aged 0–2 years, 85% to children aged 4–6 years, and 91% to persons aged 11–18 years.
Changes to Clinic Processes Implemented Due to the Pandemic
Almost all physicians reported implementing some changes to their clinic processes as a result of the pandemic, including requiring patients and families to wear face coverings (99% Peds and FPs), limiting the number of people who accompany a patient to a clinic visit (97% Peds, 94% FPs), changing the clinic’s physical space to allow for physical distancing (95% Peds, 96% FPs), and the check-in process to decrease or eliminate time spent in the clinic (93% Peds, 96% FPs) (Figure 2). Other frequently reported changes included scheduling sick and well visits during different times of the day (71% Peds, 41% FPs), giving vaccinations outdoors (34% Peds, 43% FPs), offering drive-up visits for acute illness (34% Peds, 36% FPs), and scheduling sick and well visits at different locations (33% Peds, 39% FPs). Changes reported less frequently included advising some patients and/or parents to delay some vaccinations to avoid in-person risk (10% Peds, 24% FPs) and scheduling sick and well visits on different days of the week (4% Peds, 7% FPs).
Requiring patients and families to wear a mask or face covering in clinic
Limiting the number of people who accompany a patient to a clinic visit
Changes to the physical space inside the clinic to allow physical/social distancing
Changes to the check-in process to decrease or eliminate time spent in the clinic
Scheduling sick and well visits during different times of day (morning / afternoon)
Giving vaccinations outdoors

Drive up visits for acute illness


Scheduling sick and well visits at different clinic locations


Advising patients and/or parents to delay some vaccinations to avoid in-person risk


Scheduling sick and well visits on different days of the week


Peds=pediatricians, FPs=family physicians
Perceived Barriers to Providing Vaccinations During the Pandemic
The factors most frequently reported as major or moderate barriers to providing vaccinations included fewer in-person visits because patients and/or parents were concerned about risk of SARS-CoV-2 infection (Peds, 11% major, 41% moderate; FPs, 11% major, 43% moderate), fewer in-person visits for sports clearance (Peds, 7% major, 32% moderate; FPs, 12% major, 32% moderate), and fewer back-to-school in-person visits because some children were participating in virtual learning (Peds, 5% major, 20% moderate; FPs, 6% major, 27% moderate) (Figure 3). Barriers reported less frequently included loss of health insurance coverage, lack of personal protective equipment, problems with maintaining vaccine supply, lack of adequate reimbursement when pairing a telehealth visit with in-person vaccination, patient/parent financial concerns, clinic being closed, reduced clinic staff, looser enforcement of school vaccination requirements, fewer in-person visits because of provider concern about risk of SARS-CoV-2 infection, and patients’ loss of transportation to the clinic.
Fewer in-person visits because patients and/or parents are concerned about risk of COVID-19 infection
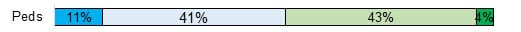
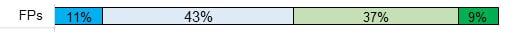
Fewer in-person visits for sports clearance
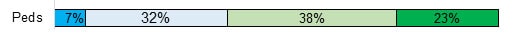
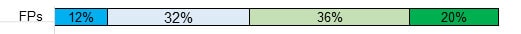
Fewer back-to-school in-person visits because some children are participating in virtual learning
Lack of personal protective equipment


Lack of adequate reimbursement when pairing a telehealth visit with in-person vaccination


Reduced clinic staff


Patients’ loss of health insurance coverage
Fewer in-person visits because providers are concerned about risk of COVID-19 infection


Patient and/or parent financial concerns

Looser enforcement of school vaccination requirements


Patients’ loss of transportation to come in to the clinic

Peds=pediatricians, FPs=family physicians
Some percentages do not add up to 100% due to rounding.
Barriers not shown due to fewer than 10% of either specialty reporting as a major or moderate barrier: clinic closed and problems with maintaining vaccine supply.
Discussion
In this nationally representative survey of primary care physicians, we observed changes in the delivery of vaccinations to children resulting from the COVID-19 pandemic. Although some physicians reported interrupting vaccination services at some point during the pandemic, the majority reported continuing to provide vaccinations throughout. Almost all physicians who had stopped providing vaccinations at some point had returned to pre-pandemic vaccination services at the time of the survey. Nearly all respondents reported making numerous changes to minimize the risk of COVID-19 transmission when delivering well care, including vaccines. Among those, there were some interesting differences by specialty. For example, more pediatricians than family physicians scheduled sick and well visits at different times of day, and more family physicians than pediatricians advised parents to delay some vaccinations. Many physicians even reported delivering vaccines outdoors. Despite these changes, the most frequently perceived barrier to vaccination during the pandemic had to do with parent concerns about contracting COVID-19 at the clinic.
It is worth noting that a large proportion of family physicians reported not delivering vaccines to children of any age—even before the pandemic—even though they conduct well-childcare visits for children in these age groups. Professional societies and public health authorities should strongly encourage all primary care physicians who care for children to provide vaccinations in their offices, and barriers to doing so should be urgently addressed.8
The results of this survey suggest that, although some primary care physician offices limited vaccination delivery for a period of time, this is not likely contributing to a continued decline in vaccination coverage in the U.S. To address the serious gaps in vaccination that we have seen as a result of the pandemic, professional societies, public health authorities, and primary care providers should work in concert to inform the general public that almost all primary care clinics are open and available to provide vaccinations to children of all ages, and the vast majority of healthcare providers are now vaccinated. Parents should also be made aware of the remarkable changes and numerous safety measures primary care practices have put in place to ensure safe vaccination during the pandemic. Further, more than half of physicians reported that parents’ loss of health insurance was at least a minor barrier to providing vaccinations. Many Americans may believe their children cannot be vaccinated because they have lost health insurance as a result of the pandemic.9 . However, many of these children are eligible for free vaccinations through the Vaccines for Children (VFC) program, so public messaging should emphasize this. In addition, primary care providers should implement vaccination reminders and recalls for parents and patients, as well as provider prompts when patients who are overdue for vaccines visit the clinic.10 Local and state health departments should consider implementing immunization information system-based recalls for children identified as behind on vaccinations.11 Schools and local public health authorities should continue to enforce school vaccination requirements, even for children attending school virtually, 12 to ensure a safe return to in-person learning for U.S. children.
References
- Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020;91(1):157–160.
- Centers for Disease Control and Prevention. Interim Guidance for Routine and Influenza Immunization Services During the COVID-19 Pandemic. Published 2020. Updated October 20, 2020. Accessed February 25, 2021.
- Mehrotra, M; Linetsky, D; Hatch, H; Cutler, D. What Impact Has COVID-19 Had on Outpatient Visits?external icon The Commonwealth Fund. To the Point website. Published 2020. Updated April 23, 2020. Accessed February 25, 2021.
- O’Leary ST, Trefren L, Roth H, Moss A, Severson R, Kempe A. Number of Childhood and Adolescent Vaccinations Administered Before and After the COVID-19 Outbreak in Colorado. JAMA Pediatr. 2021 Mar 1;175(3):305-307.
- Santoli JM, Lindley MC, DeSilva MB, et al. Effects of the COVID-19 Pandemic on Routine Pediatric Vaccine Ordering and Administration — United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(19):591–593.
- Crane LA, Daley MF, Barrow J, et al. Sentinel physician networks as a technique for rapid immunization policy surveys. Eval Health Prof. 2008;31(1):43–64.
- Brtnikova M, Crane LA, Allison MA, Hurley LP, Beaty BL, Kempe A. A method for achieving high response rates in national surveys of U.S. primary care physicians. PLoS One. 2018;13(8):e0202755.
- National Vaccine Advisory Committee. Standards for child and adolescent immunization practices. National Vaccine Advisory Committee. Pediatrics. 2003;112(4):958–963.
- Woolhandler S, Himmelstein DU. Intersecting U.S. epidemics: COVID-19 and lack of health insurance. Ann Intern Med. 2020; 173(1):63–64.
- Szilagyi P, Vann J, Bordley C, et al. Interventions aimed at improving immunization rates. Cochrane Database Syst Rev. 2002(4):CD003941.
- Kempe A, Saville AW, Dickinson LM, et al. Collaborative centralized reminder/recall notification to increase immunization rates among young children: a comparative effectiveness trial. JAMA Pediatr. 2015;169(4):365–373.
- Seither R, McGill MT, Kriss JL, et al. Vaccination Coverage with Selected Vaccines and Exemption Rates Among Children in Kindergarten — United States, 2019–20 School Year. MMWR Morb Mortal Wkly Rep. 2021;70(3):75–82.