PulseNet: 20 Years of Making Food Safer to Eat
Download Fact Sheet: PulseNet: 20 Years of Making Food Safer to Eat pdf icon[PDF – 4 pages]
Central Pillar of U.S. Food Safety System
- 1 billion pounds of contaminated food recalled since PulseNet was launched
- $507 million saved each year (medical costs and lost productivity) with quick outbreak detection
- 1 million DNA fingerprints of foodborne bacteria in the PulseNet USA database
- 89,000 DNA fingerprints of bacteria submitted to PulseNet in 2015 – a record number
- 1,500 clusters of illness from Salmonella, E. coli, and Listeria infections annually identified by PulseNet member labs
- 280 multistate clusters of illness caused by Salmonella, E. coli, and Listeria infections identified by PulseNet each year
- 83 federal, regional, state, and local laboratories in the PulseNet network
- 40 clusters of human illnesses tracked weekly
PulseNet is a national network of laboratories that solves outbreaks of foodborne disease. PulseNet scientists detect outbreaks—large and small—by connecting the dots between cases of similar illness that are happening anywhere in the country. PulseNet investigations have brought about lasting changes in food industry practices and new regulations that have made our food safer.
How PulseNet Works:
- DNA fingerprinting technology identifies the bacteria making people sick
- Database managers check the national databases for more-than-expected numbers of matching DNA fingerprints, or clusters, from anywhere in the US
- Alert state and local health departments about a possible outbreak
- PulseNet scientists work with FDAexternal icon (US Food and Drug Administration) and USDA/FSISexternal icon (US Department of Agriculture/Food Safety and Inspection Service) officials, epidemiologists, environmental health specialists to identify the contaminated food
- Public alerted of the outbreak
- Manufacturer may voluntarily recall the contaminated food
The Story of PulseNet
“APHL is proud of its long-standing connection to PulseNet, from the first software purchases to whole genome sequencing.”
Scott J. Becker, Executive Director, Association of Public Health Laboratories
In the beginning..there were contaminated hamburgers
In 1993, more than 700 people got sick and 4 died in the western United States after eating at a large fast-food chain. More than 1 month after the first person fell ill, public health investigators identified the culprit: hamburger patties contaminated with a deadly type of E. coli bacteria. This outbreak spurred foodborne disease experts at CDC to find a way to speed up detection of foodborne outbreaks.
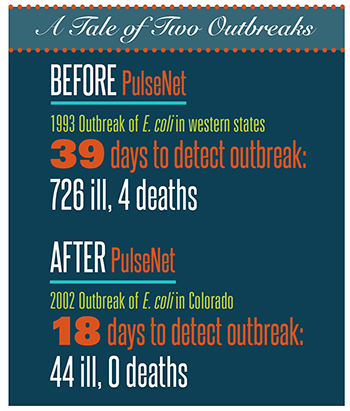
A few years later, in partnership with the Association of Public Health Laboratories (APHL)external icon, federal partners, and public health labs in 4 states, CDC created PulseNet. The goal was to create databases that would be the central repository for DNA fingerprints extracted from gut bacteria of patients with foodborne disease. Public health laboratories around the United States could submit these DNA fingerprints to PulseNet, which would be managed by CDC. When investigators searched the PulseNet databases and discovered that several ill people had bacteria with the same DNA fingerprint, they would suspect an outbreak.
Now, every state has at least one public health laboratory that uses PulseNet’s technology and can access its databases of close to 1 million fingerprints of bacteria. Because it has connected the dots between current illnesses and stored DNA fingerprints, PulseNet has revolutionized the way foodborne outbreaks are detected and investigated.
PulseNet in Action: Making food safer

In November 2014, PulseNet scientists detected two clusters of illness (35 people from 12 states, including 7 who died) caused by the foodborne bacteria Listeria. Using traditional lab analysis methods, the scientists linked sick patients who were likely to have eaten the same contaminated food. They also used whole-genome sequencing (WGS) to more precisely determine which illnesses were linked. Armed with this information, investigators interviewed patients about foods they had eaten and identified a new source of Listeria infection: caramel apples.
Real-time WGS helped investigators solve the outbreak at least 1 week sooner than would have been possible using traditional methods. The apple producer and several caramel apple manufacturers recalled apples to prevent more illnesses.
Food safety requires that we pay close attention to every step in the food supply chain, from farm to fork. Diligent efforts by farmers, producers, distributors, regulators, and consumers have made the US food supply among the safest in the world. Nevertheless, an estimated 48 million people, or 1 in 6 Americans, get sick every year from foodborne illnesses. That is where PulseNet comes in.
During outbreak investigations, scientists can use PulseNet data to identify the specific type of bacteria that caused people to get sick, track down the food that was contaminated, and find out what happened to cause the contamination. For example, in the early 2000s, PulseNet traced an outbreak of Salmonella infection to raw almonds grown in California. The outbreak prompted regulators to mandate that almonds for sale in the United States be pasteurized (by fumigation or hot steam treatment) to control the problem and prevent similar outbreaks in the future.
Outbreak investigations supported by PulseNet help scientists find gaps in food safety systems that would otherwise be unrecognized. Information from PulseNet has stimulated production changes by the food industry and helped federal agencies create new or improved recommendations and regulations to make our food supply safer.
The Future of PulseNet: Faster, Cheaper, and Better Foodborne Disease Detection
A new test
Culture-independent diagnostic tests, or CIDTs, are new tests that can detect the DNA of bacteria directly from patient samples like stool. As their name implies, CIDTs do not need a culture (cells grown in a lab) to identify the bacteria that caused a patient’s illness. Clinical laboratories are increasing their use of CIDTs because they save costs and diagnose illnesses faster.
The challenge to PulseNet
For PulseNet to work, scientists need genetic information drawn from cultures. Because CIDTs skip the step of producing a culture, these newer tests don’t produce DNA fingerprints to store in PulseNet’s database. Without these data, public health scientists will not be able to find, monitor, and prevent foodborne disease outbreaks or follow trends to know if prevention policies are working. Many outbreaks will go undetected or be detected later when the outbreak has grown, and contaminated products will remain on the market longer.
Harmonizing the system
CDC is working closely with public health officials, diagnostic laboratories, CIDT kit manufacturers, and clinicians to ensure that PulseNet collects the DNA fingerprints it needs. PulseNet is also developing a new way to detect outbreaks that doesn’t depend on cultures. These innovations are in the early stages of research and development, but we are heading toward a system that answers both needs: rapid and less costly diagnosis for individuals and a way to ensure essential data are still collected.
Transforming disease detection
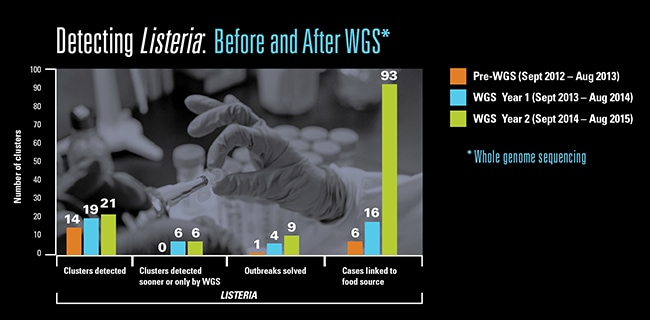
In 2013, CDC began using whole-genome sequencing (WGS) to detect outbreaks caused by Listeria, the most deadly foodborne pathogen. WGS reveals all the genetic material, or the genome, of an organism (like bacteria and viruses) in one efficient process. The Listeria project was one of the first to receive support from CDC’s Advanced Molecular Detection (AMD) initiative, a program that uses newer, more powerful, pathogen detection technologies to find outbreaks sooner. CDC is partnering with other federal agencies and state and local health departments to analyze Listeria from human cases and possible food sources.
Since the Listeria project began, scientists have detected more clusters, solved outbreaks faster with fewer cases, linked cases to likely food sources, and identified Listeria in unexpected foods, such as caramel apples and ice cream. CDC is quickly expanding the use of WGS in state laboratories and has begun using WGS for investigations of other foodborne pathogens such as Campylobacter, E. coli, and Salmonella. WGS has been a game changer for outbreak detection, spurring innovation and new discoveries. With WGS and PulseNet working in tandem, we have taken a significant leap forward in making food safer to eat.