FY 2020 Extramural Research Program Highlights: Cooperative Agreements
Cooperative Agreements
Cooperative agreements allow NIOSH to partner with universities, state health departments, labor unions, and nonprofit organizations to address important public health problems. NIOSH funds a broad array of these agreements to develop knowledge in preventing job-related injuries, illnesses, and fatalities.
In FY 2020, NIOSH funded the state surveillance program to support states in monitoring occupational injuries, diseases, exposures, and deaths. Other cooperative agreements awarded in FY 2020 included funding for occupational safety and health surveillance collaboration, education, and translation; National Mesothelioma Virtual Bank funding; and the Commercial Fishing Occupational Safety Research and Training Program. Selected highlights from the state surveillance program are provided below.
You can also find the information on this page in the NIOSH Extramural Research and Training Program: Annual Report of Fiscal Year 2020.
State Surveillance Program
The state surveillance program helps expand the ability of states to monitor work-related health and safety issues. The program supports the role of states to conduct in-depth surveillance and follow-up investigations and interventions. These local state-based skills and abilities help NIOSH meet the mandate to ensure a safe workplace.
NIOSH Sponsored State Occupational Health & Safety Surveillance Program
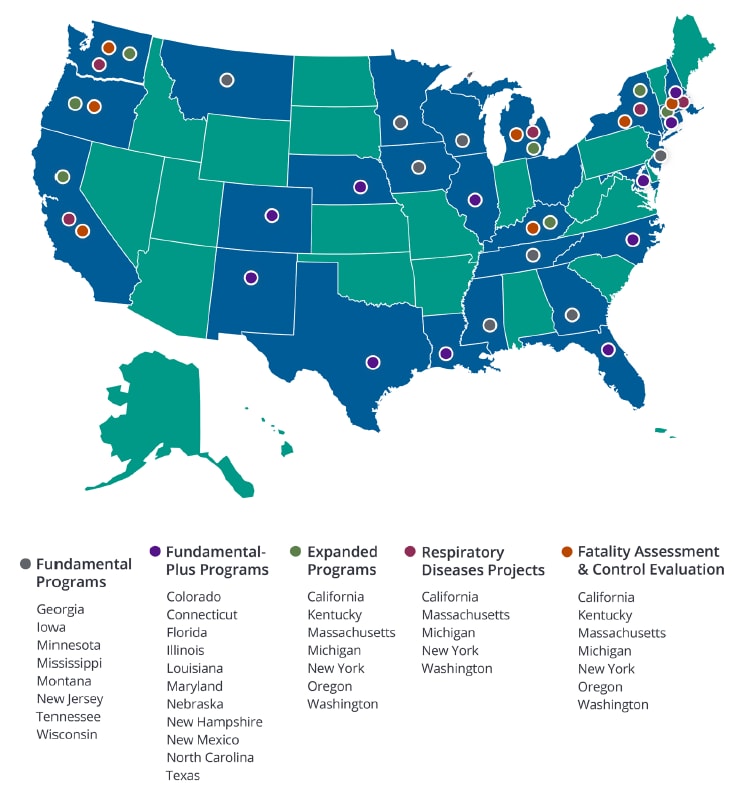
NIOSH values state programs and gives financial and technical support to state health and labor agencies, universities, and other eligible groups to develop and expand their occupational health surveillance programs. The NIOSH extramural surveillance portfolio includes 26 state recipients composed of 49 projects focusing on work-related injuries and death, exposures and hazards, and worker populations of interest. These programs use and distribute surveillance data to find the incidences of job-related injuries, illnesses, exposures, and fatalities. They help to discover trends, research opportunities, emerging issues, and high-risk worker populations. The programs also create and send out targeted educational and prevention materials, adapting materials to best protect workers. They often engage in outreach and involve partners in public health and safety to advance “data into action.”
State surveillance program outputs are the products of both nonresearch and research activities and include publications. We collected publications by NIOSH-funded extramural researchers from principal investigator reports to NIOSH, the NIH Reporter database, the NIOSHTIC-2 database, and the PubMed database. From October 1, 2019, through September 30, 2020, the state surveillance program published 14 articles in peer-reviewed journals. Find a searchable database of NIOSH publications, which includes grantee final reports and publications, by using the NIOSHTIC-2 publications search.
Occupational Injury Added to Syndromic Surveillance System
EpiCenter—the New Jersey syndromic surveillance system that alerts local and state health officials of potential community outbreaks in near real time based on data from emergency department visits—now includes occupational injury classifiers. These classifiers allow cases of workplace injuries and illnesses to be identified through keywords entered in the chief complaint field. This new addition to EpiCenter occurred through a partnership between the Occupational Health Surveillance (OHS) Unit and the Communicable Disease Service, Infectious, and Zoonotic Disease Program within the State of New Jersey Department of Health. Through the new classifiers, the OHS Unit receives alerts on potential occupational hazards, like chemical exposures, when three or more cases are reported in 24 hours. The OHS Unit also notifies the appropriate groups when these alerts are received, including the health department’s Public Employees Occupational Safety and Health, along with regional Occupational Safety and Health Administration (OSHA) offices, so immediate public health action can be taken.
Building on this milestone, staff in the health department’s OHS Unit chaired an occupational Syndromic Surveillance Workgroup for the Council of State and Territorial Epidemiologists (CSTE). CSTE invited this state surveillance program to lead the workgroup, which eventually created a guidance document for other states to use to implement their own syndromic surveillance for occupational health. The guidance includes information on how states can use syndromic surveillance and develop their occupational health syndrome definitions. The report also describes some states’ current syndromic surveillance systems, including details on their types of systems and what variables are collected. CSTE posted the guidance document on its website and featured it during its December 2019 Occupational Health Surveillance Subcommittee Meeting.
Details:
- NJ Health: Syndromic Surveillance
- NJ Health: Workplace Health and Safety Occupational Health Surveillance
- Syndromic Surveillance for Occupational Health Surveillance: Guidance Document and Examples
Effort to Prevent Opioid Exposure Reaches Thousands of Georgia First Responders
Carfentanil and other similar substances designed to mimic fentanyl—a synthetic, or manmade, opioid—can be harmful to public safety, first responder, and medical treatment and laboratory workers. Emergency responders are likely to come into contact with illicit drugs on the job, including opioids such as fentanyl and fentanyl-related compounds like Carfentanil. These substances are increasingly linked to opioid overdose deaths. Fentanyl and substances that are compounds from its drug class have many forms, like powder or liquid, and exposed workers can accidentally inhale or absorb it through the skin. In 2018, emergency medical services (EMS) and law enforcement personnel completed a survey on opioid exposure, given by the Georgia Department of Public Health Occupational Health & Safety Surveillance Program (GA-OHS). Less than half of the workers knew about CDC/NIOSH recommendations for preventing opioid exposures among first responders, according to survey findings.
Based on these data, GA-OHS determined a need for more education and outreach on preventing opioid exposure. The program created a fact sheet in FY 2020 summarizing CDC/NIOSH recommendations entitled “First Responder Safety Precautions for Dealing With Unknown Opioids,” and widely distributed the document. All licensed EMS personnel in Georgia received the fact sheet via email, totaling more than 20,000 workers. The program also hosted a booth at the 2019 Georgia EMS Association Providers and Educators Conference in October 2019, where GA-OHS staff talked with hundreds of EMS personnel. They handed out the fact sheets, along with information on the NIOSH illicit drug toolkit, and provided education on preventing opioid exposures, including use of personal protective equipment. The Georgia Association of Chiefs of Police also featured the fact sheet in its quarterly newsletter.
Details:
- Opioid Epidemic: First Responders and EMS
- Preventing Emergency Responders’ Exposures to Illicit Drugs
- Fentanyl
- Georgia Association of Chiefs of Police Online Quarterly News
Identification of Top Occupational Injury Claims in Massachusetts
In a study examining workers’ compensation claims from 2014 through 2016, the Massachusetts Department of Public Health, in collaboration with the Massachusetts Department of Industrial Accidents and the Massachusetts Department of Labor Standards, found state workers filed claims most often for strains and sprains. Investigators used previously unavailable data from the Massachusetts Department of Industrial Accidents and looked at trends of occupational injuries and illnesses for private sector workers. Analyzing 93,123 workers’ compensation lost-wage claims, they identified common types of incidents leading to injuries and illnesses and reported demographics like gender, age, and industry. The claims were filed during 2014–2016 for employees working at least 40 hours weekly, equaling to an average of 31,041 claims per year.
The occupational sectors with the highest claim rates included Transportation and Warehousing, Construction, Healthcare and Social Assistance, and Wholesale and Retail Trade. Other key findings included that injuries accounted for 95% of all claims, with most of the workers experiencing strains and sprains (51%); contusions, crushings, bruises (12%); fractures (9%); and cuts, lacerations, and punctures (8%). Overexertion due to lifting and pushing marked the top cause of all injuries (38%), followed by slips, trips, and falls (29%), contact with an object or equipment (19%), and violence and transportation incidents (5%). Males filed the majority of claims, along with workers aged 55–64 years who mostly reported being injured from a fall on the same level. These findings can help guide research and prevention efforts—full results are available in a report released in November 2019.
Details:
- Outside NIOSH: Strains and Sprains Lead Work-related Injury Claims in Massachusetts
- Occupational Health Surveillance Program
Surveillance Uncovers Hazardous Lead Exposure at Small Business
The New York State Department of Health (NYSDOH) uses its Heavy Metals Registry (HMR) to collect surveillance data on adult exposures to lead, mercury, cadmium, and arsenic. The registry helped the NYSDOH surveillance program identify 27 workers at a small business who had the highest blood lead levels (BLLs) ever recorded in the HMR. They were subcontractor field technicians hired by a specialty company to remove and refurbish older windows in a commercial building under renovation. After looking into the situation, the program found the commercial building was older with lead paint on its interior and exterior surfaces, as well as its windows and doors. The investigation also revealed the company did not test the facility for lead, and employees reported safety rules were not enforced onsite, along with a lack of respiratory protection and guidance on sanitation and hygiene practices for lead exposure.
The business responded to the incident with several actions including putting their workers on a medical monitoring plan based on OSHA guidelines and setting up a Respiratory Protection Program. The workers must now wear personal protective equipment, including respirators, which they are fit tested for, when around lead or other harmful materials. The company also developed standard operating procedures (SOPs) that include the new safety and health changes. They trained all employees on the SOPs and now offer an annual lead training that includes a review of OSHA standards and lead hazards.
The NYSDOH surveillance program continues to monitor the workers’ BLLs and tracks the company’s progress in implementing the new safety and health changes. The program also offers follow-up medical care to the workers, when needed, through its Occupational Health Clinic Network, which assists thousands of patients annually for occupational illness and injuries.
Details:
- Heavy Metals Surveillance: New York State Heavy Metals Registry
- Occupational Health Clinic Network—Prevention and Protection for the NYS Workforce
Identification of Injury Risks Associated With Motor Vehicle Towing
Past data show that deaths related to managing the scene after motor vehicle crashes most likely involve commercial tow truck operators. Following roadway incidents, these workers coordinate with traffic incident managers in multiple ways to remove disabled or nonworking vehicles, clearing debris and cleaning up fallen cargo. Research shows these workers have a high likelihood of being struck by roadway traffic, also called pedestrian struck-by incidents, when performing these traffic incident management (TIM) activities. In fact, commercial tow truck operators are at greater risk than other first responders with TIM functions like fire, police, and emergency medical personnel.
Limited research exists on hazards related to motor vehicle towing (MVT) and effective safety strategies for this industry. To address this issue, the Kentucky Occupational Health and Safety Surveillance Program used OSHA data to describe factors linked to injuries among commercial tow truck operators as they provided roadside assistance. They analyzed information from OSHA investigation files from 2002–2017, specifically the written descriptions of each injury event. They also examined separate data on weather conditions for each case.
In total, there were 106 cases where tow truck operators died or were severely hurt, but researchers could only get detailed descriptions for 41 cases. They focused on types of injury incidents and related causes. Most of the incidents were either struck-by incidents or caught-in or -between’ incidents, where workers were pinned beneath or between vehicles or caught in their moving parts.
According to researchers, these findings demonstrate the need for first-time and refresher safety trainings in the MVT industry on loading and unloading vehicles and defensive techniques while around roadway traffic. Researchers also recommended trainings on proper wheel chocking and braking procedures, advocating for states to add tow trucks to the list of first responder vehicles in “Move Over” laws. The Journal of Safety Research published this study in December 2019, and the Kentucky surveillance program shared its findings with the Towing and Recovery Association of America and Emergency Road Service Coalition of America.
Details:
