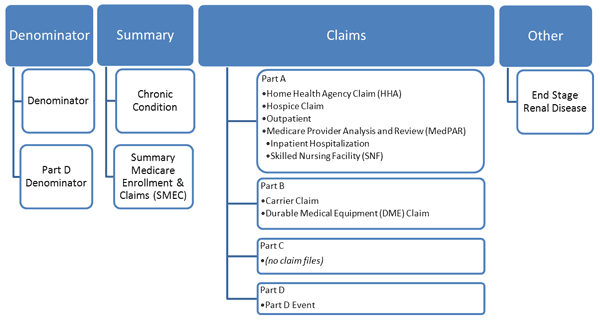
Diagram: NHANES-Medicare Linked Data Structure
View text version of Diagram
Medicare enrollment and fee-for-service (FFS) claims data are available for NCHS respondents who are considered linkage eligible and matched to the CMS Denominator file. To link the NCHS survey respondents with their Medicare data, the following identifiers were used: Social Security Number (SSN), date of birth (month, day, year), and sex. To be considered a successful match, the NCHS survey respondent’s record needed to match exactly to the CMS Denominator file on all three items listed above. CMS provided NCHS with Medicare FFS claims data for all successfully matched NHANES participants. CMS also provided Medicare Part D prescription drug event data to NCHS, beginning with the onset of the Part D benefit in 2006. Refer to Course 1, Module 4, Task 2 “Years of NHANES-CMS linked data” for the range of NHANES and CMS years of data that are linked.
The CMS claims files linked to NHANES data are all finalized claims files. These files are generated from raw claims through final action algorithms that match the original claim with adjusted claims to resolve any adjustments. Finalized claim files are available from CMS approximately nine months into the following calendar year (for example: 2007 data will become available in September of 2008). The files are annual and are available for Part A (inpatient, outpatient, Skilled Nursing Facility, hospice, or Home Health Agency) and for Part B (Carrier, Durable Medical Equipment).
The files contain information collected by Medicare to pay for health care services provided to a Medicare beneficiary. There is one record in the file for each claim (note some episodes of care include more than one claim).
The following is a list and description of Medicare files that have been linked with NHANES.
Denominator File: The Denominator File contains basic demographic and enrollment information about each beneficiary entitled to Medicare during each calendar year and is needed to construct an analytic data file, particularly to identify Medicare beneficiaries enrolled in a Medicare Part C plan. Medicare Part C plans are also referred to as Medicare Advantage (MA) and include Health Maintenance Organizations (HMOs), Preferred Provider Organizations (PPOs), Private Fee-for-Service (PFFS) Plans, Special Needs Plans, and Medicare Medical Savings Account Plans.
You should always include a request for the Denominator File as part of the data request.
Part D Denominator File: The Medicare Part D Denominator File contains demographic and enrollment data, with additional Part D enrollment data, for each beneficiary enrolled in Medicare during the calendar year.
If you intend to analyze Part D event data, a request for the Part D Denominator File should also be included as part of the data request.
Chronic Condition Summary File: The Chronic Condition Summary File is used to indicate the presence of the 21 Chronic Condition Warehouse condition indicators for all beneficiaries.
Summary Medicare Enrollment and Claims (SMEC) File: The SMEC files, created by NCHS, were designed to be used for analyzing Medicare cost and claims data from multiple Medicare service files.
Home Health Agency (HHA) Claim File: The HHA Claim File contains claims data submitted by HHA providers.
Hospice Claim File: The Hospice Claim File contains claims data submitted by hospice providers.
Outpatient Claim File: The Outpatient Claim File contains claims data submitted by institutional outpatient providers.
Medicare Provider Analysis and Review (MedPAR) and Skilled Nursing Facility (SNF) Files: The MedPAR Hospital and SNF Files contain inpatient hospital and skilled nursing facility (SNF) stay data. An inpatient "stay" record summarizes all services rendered to a beneficiary from the time of facility admission through discharge.
Carrier Claim File: The Carrier Claim File (previously referred to as the Physician/Supplier Part B file) contains claims data submitted by non-institutional providers.
Durable Medical Equipment (DME) Claim File: The DME File contains claims data submitted by DME regional carriers to CMS.
Part D Drug Event (PDE) File: The PDE File contains prescription drug costs and payment data that enable CMS to make payments to the plans and otherwise administer the Part D benefit.
Part C (Medicare Advantage (MA) plans are offered by private companies approved by Medicare. There are no Part C claims files among the linked data files.These beneficiaries should be excluded from any analysis involving claims because they do not have claims data. Refer to Module 8 for details on how to use the Denominator File to identify managed care participants.
End Stage Renal Disease (ESRD) File: NCHS has linked to a separate set of data files from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) containing information on patients diagnosed with End Stage Renal Disease (ESRD). The ESRD data files can be used by researchers interested in conducting analysis specifically related to patients with ESRD.
Medicaid is administered by states under general guidelines established by the federal government and is financed jointly by federal and state funds. The Federal Medical Assistance Percentage (FMAP), also called the federal match rate, represents the percent of Medicaid financed by the federal government in each state. The FMAP differs by state and takes into account the average per capita income in a state relative to the national average. You can find the FMAP for individual states for each federal fiscal year in the Federal Percentages and Federal Medical Assistance Percentages table produced by the Department of Health and Human Services’ Assistant Secretary for Planning and Evaluation. See the Resources section for the link to this material.
State Medicaid programs must cover mandatory services specified in federal law to receive federal matching funds. Beneficiaries are entitled to receive the following mandatory services:
Medicaid long-term care services include comprehensive services provided in nursing homes and intermediate care facilities for the mentally retarded (ICF‐MR). Long-term care also includes a wide range of services and supports needed by people to live independently in the community, including home health care, personal care, medical equipment, rehabilitative therapy, adult day care, case management and respite for caregivers.
States are also permitted to cover many services that federal law designates as optional, including dental services, prescription drugs, case management, and hospice services. State variation in Medicaid coverage, with regard to both program eligibility and covered services, results in state differences in enrollment rates and expenditures. Other factors, including the age distribution, the poverty rate, and the Medicaid provider reimbursement rates, also contribute to variation among states in enrollment, service use, and costs. As a result, Medicaid operates as more than 50 distinct programs – one in each state, the District of Columbia, and each of the territories. Consideration of these state-level differences may be necessary for many analyses. State identifiers for NHANES need to be specifically requested in those circumstances. State identifiers are not available in public use data files and must be specifically requested in NCHS Research Data Center proposals.