Incidence, Prevalence, and Cost of Sexually Transmitted Infections in the United States
FACT SHEET
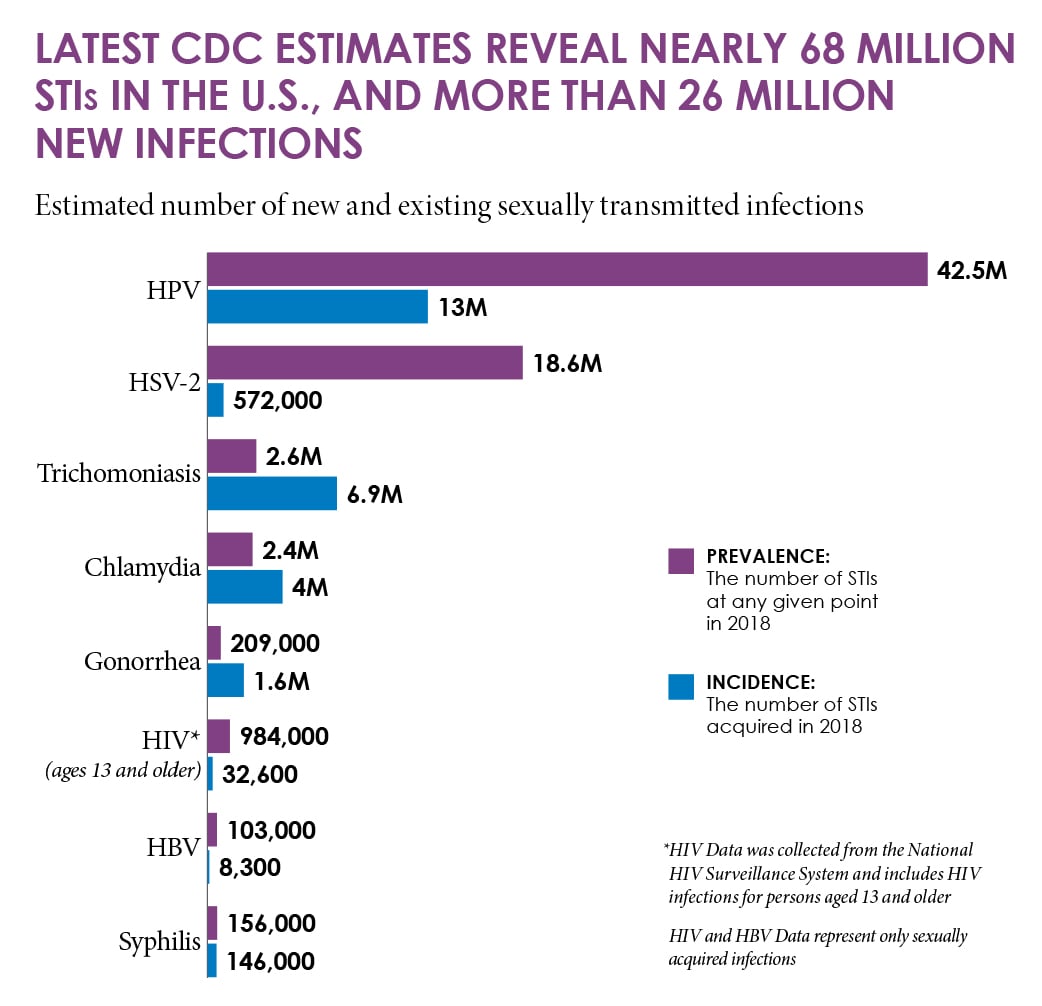
2021 CDC analyses1,2 provide the clearest picture to date of how common and costly sexually transmitted infections (STIs) are in the United States. CDC’s latest estimates indicate that 20% of the U.S. population – approximately one in five people – had an STI on any given day in 2018, and STIs acquired that year cost the American healthcare system nearly $16 billion in direct medical costs alone.
CDC’s analyses included eight common STIs, four of which are easily treated and cured if diagnosed early: chlamydia, gonorrhea, syphilis, and trichomoniasis. Also included in the analyses are four sexually transmitted viruses: human papillomavirus (HPV), herpes simplex virus type 2 (HSV-2), human immunodeficiency virus (HIV), and hepatitis B virus (HBV). Many of these infections go undetected because they often have no symptoms and can have serious health consequences.
1 in 5 people in the U.S. have an STI
Nearly 68 million infections

26 million
STIs acquired in 2018

Nearly $16 billion
Total medical costs
(in 2018 dollars)

NEARLY HALF OF ALL NEW INFECTIONS OCCUR AMONG NATION’S YOUTH
America’s youth shoulder a substantial burden of sexually transmitted infections.
Nearly half (46%) of all new STIs in the country occur among young people (ages 15-24).
Estimated number of new and existing sexually transmitted infections.
PREVALENCE: The number of people with an STI at a given point in 2018.
INCIDENCE: The number of people who acquired a disease in 2018.
*HIV Data was collected from the National HIV Surveillance System and includes HIV infections for persons aged 13 and older
HPV
infections
HPV
infections
PREVALENCE: 42.5M
PREVALENCE: 42.5M
INCIDENCE: 13M
INCIDENCE: 13M
HSV-2
infections
HSV-2
infections
PREVALENCE: 18.6M
PREVALENCE: 18.6M
INCIDENCE: 572,000
INCIDENCE: 572,000
Trichomoniasis
infections
Trichomoniasis
infections
PREVALENCE: 2.6M
PREVALENCE: 2.6M
INCIDENCE: 6.9M
INCIDENCE: 6.9M
Chlamydia
infections
Chlamydia
infections
PREVALENCE: 2.4M
PREVALENCE: 2.4M
INCIDENCE: 4M
INCIDENCE: 4M
Gonorrhea
infections
Gonorrhea
infections
PREVALENCE: 209,000
PREVALENCE: 209,000
INCIDENCE: 1.6M
INCIDENCE: 1.6M
HIV*
infections
(ages 13 and older)
HIV*
infections
(ages 13 and older)
PREVALENCE: 984,000
PREVALENCE: 984,000
INCIDENCE: 32,600
INCIDENCE: 32,600
HBV
infections
HBV
infections
PREVALENCE: 103,000
PREVALENCE: 103,000
INCIDENCE: 8,300
INCIDENCE: 8,300
Syphilis
infections
Syphilis
infections
PREVALENCE: 156,000
PREVALENCE: 156,000
INCIDENCE: 146,000
INCIDENCE: 146,000
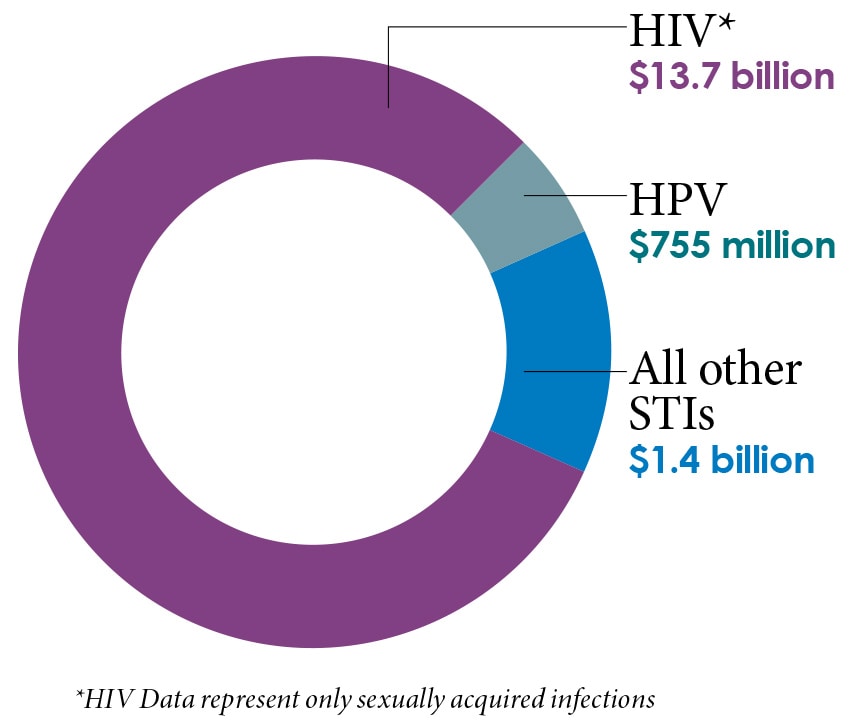
In 2018, new infections totaled nearly $16 billion in direct lifetime medical costs

CHLAMYDIA, GONORRHEA, and SYPHILIS combined accounted for
$1.1 billion in direct medical costs
Care for young people (ages 15-24) accounted for about 60% of these costs

Care for women represented nearly
75% of all STI-related medical costs (not including HIV care)
While medical costs alone are significant, the overall cost of STIs is higher when factoring in costs associated with maternal transmission, STI prevention, lost productivity, or other non-medical costs.
Because STIs are preventable, significant reductions in new infections are not only possible, they are urgently needed. Prevention can minimize the negative, long-term consequences of STIs and reduce healthcare costs. To do this, prevention efforts should:
- Focus on disproportionately affected populations. Young people and women face some of the biggest impacts and most significant consequences of STIs.
- Consider the social, cultural & economic conditions that make it more difficult for some sexually active people to stay healthy (e.g., poverty, unstable housing, drug use, lack of medical insurance or medical home, high burden of STIs in some communities).
More information on STD prevention is available here.
For all individuals who are sexually active – particularly young people and women – STI screening and prompt treatment (if infected) are critical to protect a person’s health and prevent transmission to others. If you are sexually active, be sure to talk to your healthcare provider about STI testing and which tests may be right for you. CDC’s STI screening recommendations are available here and information for providers can be found here.