Questions and Answers about HIP
HIP is an approach to disease prevention in which cost-effective, proven, and scalable interventions are targeted to specific populations on the basis of disease burden. It provides a strategy for using data to maximize the impact of available resources and interventions. The primary goals of HIP are to prevent the largest number of new infections, save life-years, and reduce disparities among populations. In this approach to disease prevention, resources are aligned with disease burden in geographic areas and within populations.
CDC funds jurisdictions by aligning the amount of funding according to disease burden. The number of cases per jurisdiction is calculated by using surveillance data. Funding amounts are then set on the basis of disease burden in each jurisdiction. Other factors are sometimes considered, such as merit, disease severity among patients, or reducing disparities among populations with low burden but high rates of poor outcomes. All jurisdictions, even those with a low disease burden, receive a baseline amount for implementing required programmatic activities. Two case studies demonstrate how this was achieved.
Jurisdictions are also expected to align resources according to geographic areas or populations with the greatest disease burden within their jurisdiction. Populations with low burden but high disparities also are considered high priority when using a HIP approach to resource allocation.
The HIP approach uses a 4-step process to determine which interventions will lead to the greatest reduction in disease or disparities (see visual).
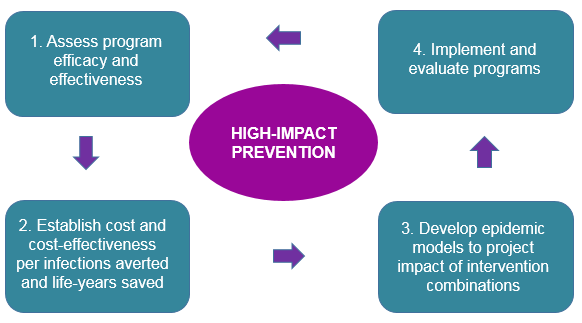
- Assess program efficacy and effectiveness. Efficacy means how successful interventions are when implemented in optimal or controlled environments; effectiveness means how successful interventions are when implemented in everyday situations. For example, condoms are almost 100% effective in preventing HIV when people use them the correct way every time they have sex; however, in everyday life, people do not always use condoms correctly, reducing their effectiveness.
- Establish cost and cost-effectiveness per infection averted and life-years saved. Although all proven interventions might have a place in prevention activities, HIP prioritizes those that are most cost-effective in reducing overall new infections. Cost-effectiveness analyses involve calculating the costs and outcomes of a program. Measured outcomes include cases of a disease prevented, years of life gained, or quality-adjusted life-years (i.e., 1 year of perfect health equals 1 quality-adjusted life-year, but 1 year of illness might only equal 0.5 years). For example, in 2012, CDC recommended that US residents born during 1945–1965 receive a 1-time antibody test for hepatitis C virus. Since then, new, highly effective drugs have been released, and clinical treatment recommendations have been updated to incorporate their use. The cost-effectiveness analyses indicate that the new treatments (i.e., pegylated interferon combined with ribavirin and sofosbuvir and the combination of sofosbuvir and simeprevir) are cost-effective per person treated, compared with their alternatives.1
- Develop epidemic models to project impact of intervention combinations. HIP assigns priority to interventions that are practical to implement on a large scale and are cost-effective. Modeling the effect of multiple interventions at the same time gives valuable information on which intervention combinations are likely to prevent the greatest number of new infections. An example of this type of modeling was used in the Enhanced Comprehensive HIV Prevention Planning project. For that project, health departments in 12 US cities with a high prevalence of HIV initiated innovative demonstration projects by using comprehensive program planning and cost-effective and scalable HIV prevention interventions to target populations at high risk. In Los Angeles County, California, the health department developed a model to assess which intervention combination might lead to the greatest number of infections averted for the lowest cost. The model estimated that investment in antiretroviral treatment and adherence to treatment was more cost-effective in reducing HIV infection than the existing approach of implementing behavioral risk-reduction interventions. The modeling results supported a change in programmatic efforts that led to better outcomes (CDC. Enhanced Comprehensive HIV Prevention Planning and Implementation for Metropolitan Statistical Areas Most Affected by HIV/AIDS. Atlanta, GA: US Department of Health and Human Services, CDC; 2017).
- Implement and evaluate programs. Ongoing evaluation provides valuable information regarding which programs are working and which ones need adjustment to improve outcomes. CDC monitors and evaluates programs across the nation to identify success and areas in need of improvement. For example, the HIV Prevention Progress Report, 2019 [PDF – 37.1 MB]2 summarizes progress on multiple indicators and identifies areas in which additional programmatic efforts are needed. Likewise, the National Tuberculosis Indicators State Comparison Reports3 provide information about national and state progress toward established TB prevention targets.
References
- Rein DB, Wittenborn SJ, Smith BD, Liffmann DK, Ward JW. The cost-effectiveness, health benefits, and financial costs of new antiviral treatments for hepatitis C virus. Clin Infect Dis 2015;61:157–68).
- CDC. HIV Prevention Progress Report [PDF – 37.1 MB]: Includes National and State Level Data for 2010 Through 2017 Where Available. Atlanta, GA: US Department of Health and Human Services, CDC; 2019
- CDC. 2017 State and City Tuberculosis Report. Atlanta, GA: US Department of Health and Human Services, CDC; [undated]
Reviewing the existing cost-effectiveness research will help identify interventions that are HIP. In addition, CDC funds model development for evaluating cost-effectiveness, including through its NCHHSTP Epidemiologic and Economic Modeling Agreement. The models identified as effective are shared in the public health literature for others to use in their jurisdictions. Additionally, CDC has made available at the Effective Interventions web site those interventions that are highly effective in HIV prevention activities. Many of the interventions encompass other diseases in addition to HIV, including hepatitis, tuberculosis, or sexually transmitted diseases, and focus on different populations, including youth, men who have sex with men, or persons who inject drugs.
If you work in public health, you are probably already using HIP. This approach has a basis in the traditional public health framework, such as using data for identifying or monitoring a priority area, choosing the best intervention that works for your clients and locality, and providing ongoing monitoring and evaluation. By coordinating this effort in a more structured framework, CDC can help direct national priorities, evaluate interventions, and package and disseminate those interventions that are highly effective. Also, CDC can fund development of cost-effectiveness models and provide funding and technical assistance to jurisdictions.
Overall, HIP can help you:
- prevent new infections,
- increase years of life and add quality of life to those years,
- reduce disparities,
- increase efficiency,
- define the problem,
- focus your resources,
- work smarter and more collaboratively,
- reach your goals, and
- provide the most cost-effective services in your jurisdiction.
HIP is a process for efficiently and effectively identifying a problem and choosing the best intervention(s) to address it. Without using the systematic HIP framework, well-intentioned programs might not be as effective or as efficient as they could be.