Diagnosis of transplant-associated rabies virus infection in the United States (AL, AR, OK, TX)
2004
In 2004, four organ recipients from a common organ donor died of a brain infection of unknown cause. All recipients developed encephalitis within a month after transplant surgery and died about two weeks after the onset of neurologic symptoms. Autopsy tissue samples from all four recipients were sent to IDPB for pathology testing. The results showed evidence that the brain cells were infected with rabies. This process of detecting antigens in a cell (immunohistochemistry or IHC) led to a diagnosis of rabies in all recipients.
The organ donor originally went to the hospital because of altered mental status and was declared brain-dead after worsening neurologic symptoms. Screening and testing normally done on potential organ donors did not reveal any signs or symptoms to prohibit transplantation and the donor’s death was thought to be due to non-infectious causes. Friends of the donor, when questioned after the donor’s death, indicated the donor had recently reported being bitten by a bat. Bats are known to be common carrier of rabies virus. For more information about bats, visit CDC’s Bats and Rabies site.
These were the first documented cases of rabies virus transmission among solid organ transplant recipients. Infection likely occurred via tissue contained in the organs. These cases illustrate the potential for transmission of infectious disease through organ transplantation and that the prevention and recognition of transplant-associated infections may be improved.
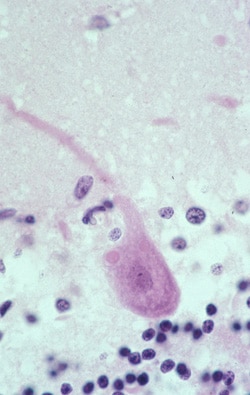
This is an photomicrograph of a hematoxylin and eosin stain of brain tissue from a patient infected with rabies virus. The eosinophilic (pink) intracytoplasmic inclusion (Negri body) characteristic of rabies infection can be seen in this photo.