Job-Aid for Detention Facilities During Mumps Outbreaks
What Health Departments Need to Know When Responding to Mumps Outbreaks in Correctional and Detention Facilities*
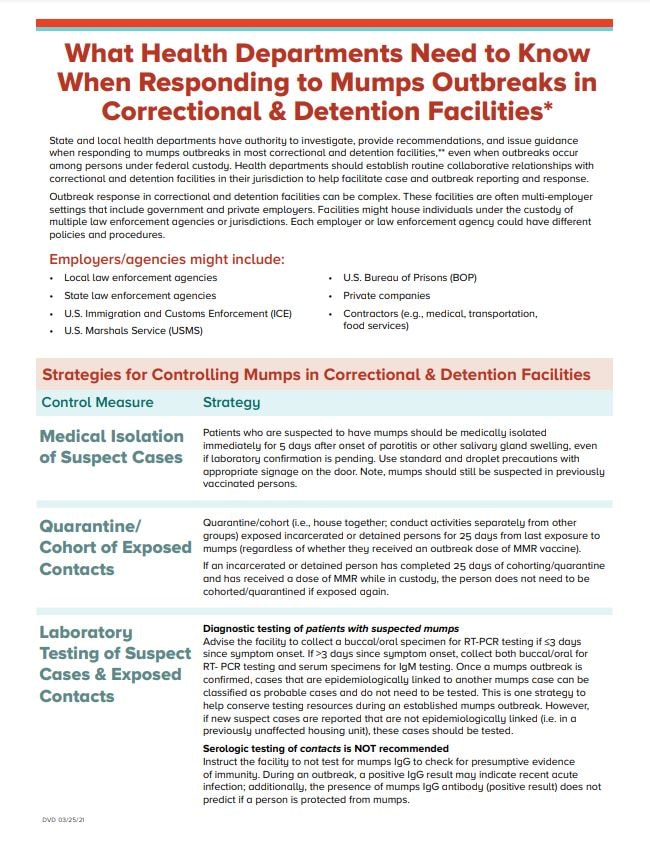
State and local health departments have authority to investigate, provide recommendations, and issue guidance when responding to mumps outbreaks in most correctional and detention facilities,** even when outbreaks occur among persons under federal custody. Health departments should establish routine collaborative relationships with correctional and detention facilities in their jurisdiction to help facilitate case and outbreak reporting and response.
Outbreak response in correctional and detention facilities can be complex. These facilities are often multi-employer settings that include government and private employers. Facilities might house individuals under the custody of multiple law enforcement agencies or jurisdictions. Each employer or law enforcement agency could have different policies and procedures.
Employers/agencies might include:
- Local law enforcement agencies
- State law enforcement agencies
- U.S. Immigration and Customs Enforcement (ICE)
- U.S. Marshals Service (USMS)
- U.S. Bureau of Prisons (BOP)
- Private companies
- Contractors (e.g., medical, transportation, food services)
Strategies for Controlling Mumps In Correctional and Detention Facilities
| Control Measure | Strategy |
|---|---|
| Medical Isolation of Suspect Cases | Patients who are suspected to have mumps should be medically isolated immediately for 5 days after onset of parotitis or other salivary gland swelling, even if laboratory confirmation is pending. Use standard and droplet precautions with appropriate signage on the door. Note, mumps should still be suspected in previously vaccinated persons. |
| Quarantine/cohort of Exposed Contacts | Quarantine/cohort (i.e., house together; conduct activities separately from other groups) exposed incarcerated or detained persons for 25 days from last exposure to mumps (regardless of whether they received an outbreak dose of MMR vaccine).
If an incarcerated or detained person has completed 25 days of cohorting/quarantine and has received a dose of MMR while in custody, the person does not need to be cohorted/quarantined if exposed again.
|
| Laboratory Testing of Suspect Cases and Exposed Contacts | Diagnostic testing of patients with suspected mumps Advise the facility to collect a buccal/oral specimen for RT-PCR testing if ≤3 days since symptom onset. If >3 days since symptom onset, collect both buccal/oral for RT-PCR testing and serum specimens for IgM testing. Once a mumps outbreak is confirmed, cases that are epidemiologically linked to another mumps case can be classified as probable cases and do not need to be tested. This is one strategy to help conserve testing resources during an established mumps outbreak. However, if new suspect cases are reported that are not epidemiologically linked (i.e. in a previously unaffected housing unit), these cases should be tested. Serologic testing of contacts is NOT recommended
Instruct the facility to not test for mumps IgG to check for presumptive evidence of immunity. During an outbreak, a positive IgG result may indicate recent acute infection; additionally, the presence of mumps IgG antibody (positive result) does not predict if a person is protected from mumps. |
| Vaccination of Exposed Contacts | Advise the facility medical staff to: Offer all exposed incarcerated and detained persons a dose of MMR vaccine. Advise facilities to screen for MMR vaccine precautions and contraindications. Investigate to determine if there are other groups of incarcerated or detained persons at the facility who are likely to have close contact with a mumps patient and offer a dose of MMR vaccine (e.g. persons from other units who may have contact with the same staff members or use the same services/areas).
Consider recommending a dose of MMR vaccine for all staff who have close contact with incarcerated or detained persons. This includes public sector employees, private contractors (e.g. food, sanitation, and transport services), and healthcare workers.
MMR vaccine is not effective at preventing mumps after exposure but should still be given to exposed persons to help protect against future exposures if the current exposure did not result in infection.
|
| Vaccine Procurement |
|
| Documentation of Vaccination | Advise the facility medical staff to:
|
*Correctional facilities refer to state and federal prisons, which incarcerate persons who have been tried for a crime, convicted, and sentenced for a duration >1 year. Those convicted of federal crimes are incarcerated in federal prisons; those convicted of state crimes are held in state prisons.
Detention facilities refer to jails or detention centers, which temporarily detain persons awaiting sentencing or deportation, usually for a duration of <1 year.
**Exceptions include facilities that are both federally owned and operated, CBP border patrol stations, and facilities where ICE Health Service Corps staff the medical services.