 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Importance of Culture Confirmation of Shiga Toxin-producing Escherichia coli Infection as Illustrated by Outbreaks of Gastroenteritis --- New York and North Carolina, 2005Escherichia coli O157:H7 and other strains of E. coli that produce Shiga toxin are collectively known as Shiga toxin-producing E. coli (STEC). The current outbreak of STEC O157 infections associated with eating fresh spinach illustrates the importance of obtaining isolates to identify the source of the infections (1). Laboratory methods that do not require bacterial culture of stool specimens to identify STEC are being used increasingly by clinical diagnostic laboratories, sometimes without subsequent confirmation of a strain by isolating it in culture. This report describes findings from outbreaks of gastroenteritis in 2005 in New York and North Carolina in which clinical diagnostic laboratories initially used only non-culture methods to detect Shiga toxin (Stx). The findings highlight the importance of confirmation of Stx-positive stool specimens by bacterial culture for timely and reliable identification of STEC infections, including E. coli O157 and non-O157 STEC, to enable implementation of appropriate public health actions. An important part of that identification is determining the serotype of all STEC isolates and the subtype of STEC O157 strains so that outbreaks can be detected and traced back to sources. New YorkDuring August 28--September 13, 2005, a total of 52 (2.4%) of 2,160 inmates at a state correctional facility reported diarrhea, including 17 (33%) with bloody diarrhea. Nineteen inmates were treated at the prison infirmary; three were hospitalized for an average of 1.8 days. Stool specimens from these three inmates tested positive for Stx by enzyme immunoassay (EIA) at a clinical diagnostic laboratory. Subsequently, stool specimens collected from 21 ill inmates were submitted to the New York State Department of Health (NYSDOH)-Wadsworth Center. Stool specimens were inoculated to E. coli enrichment broth and sorbitol MacConkey agar (SMAC), a selective medium used to screen for STEC serotype O157:H7 because this serotype, unlike most E. coli (and unlike most STEC), does not ferment sorbitol. Sixteen of the stool enrichment broths, when tested by polymerase chain reaction (PCR), were positive for the Shiga toxin 1 gene (stx1) but negative for STEC O157-specific DNA; 13 of the SMAC agar plates demonstrated growth of sorbitol-fermenting E. coli colonies that also were positive for stx1 by PCR and did not agglutinate with commercial latex reagents for STEC serogroups O26, O91, O103, O111, O128, O145, and O157. Isolates from three patients were sent to CDC and determined to be STEC serotype O45:nonmotile (NM) (one patient had both STEC serotype O45:NM and O45:H2). These STEC O45 isolates were indistinguishable by pulsed-field gel electrophoresis (PFGE) using XbaI and BlnI restriction endonucleases. The source of the outbreak likely was an ill food worker. Control measures included enhanced surveillance for additional illness and reminders of the need for exclusion of the infected food worker from food service or other jobs with increased risk for transmission until his specimens no longer tested positive for STEC. North CarolinaOn November 10, 2005, the Davidson County Health Department received a report of non-bloody diarrheal illness in an infant aged 6 months who attended a day care center. Diarrhea was reported in four additional day care center attendees and three family members of the index patient. An enrichment broth from a stool specimen from the index patient tested positive for Stx by EIA at a clinical diagnostic laboratory. After a delay of some days, the laboratory sent the enrichment broth culture of this stool specimen to the North Carolina State Laboratory for Public Health, where neither STEC O157 nor STEC serogroups O26, O45, O103, O121, O111, or O145 were isolated. The enrichment broth was then sent to CDC, where it again tested positive for Stx by EIA, but PCR tests of the enrichment broth at CDC were negative for stx1 and stx2. The enrichment broth was plated on SMAC, and PCR tests of both a sweep of growth from the plate and of 10 sorbitol-fermenting colonies were negative for stx1 or stx2. Subsequently, the North Carolina State Laboratory for Public Health performed additional testing on stool specimens from five ill persons, including the index case; each tested positive for norovirus by reverse transcription-PCR. In response to the initial Stx-positive report, public health control measures appropriate for STEC had been instituted, including exclusion of the index case from the day care center pending receipt of two STEC-negative cultures of stool specimens collected at least 24 hours apart. These exclusion measures also had been enforced for the four other ill children in the day care center. When the outbreak was determined to have been caused by norovirus, not STEC, control measures were revised, and the ill children were allowed to return to the day care center after they became asymptomatic. Reported by: R Atkinson, PhD, G Johnson, T Root, T Halse, D Wroblewski, MS, New York State Dept of Health. M Davies, MD, A Byrd, L Long, MSA, Davidson County Health Dept, North Carolina. L Demma, PhD, F Angulo, DVM, PhD, C Bopp, MS, P Gerner-Smidt, MD, PhD, N Strockbine, PhD, K Greene, B Swaminathan, PhD, P Griffin, MD, Div of Foodborne, Bacterial, and Mycotic Diseases, National Center for Zoonotic, Vector-Borne, and Enteric Diseases (proposed); J Schaffzin, MD, PhD, B Goode, MPH, EIS officers, CDC. Editorial Note:The New York outbreak demonstrates that Stx testing of stool specimens from patients with diarrhea by clinical diagnostic laboratories can facilitate detection of outbreaks of non-O157 STEC. However, as the North Carolina outbreak demonstrates, occasional false-positive results from the Stx EIA test can result in inappropriate and unnecessary public health action. These two outbreaks illustrate the importance of culture confirmation of Stx EIA-positive specimens. Although STEC O45 is an important cause of sporadic non-O157 STEC infections in the United States, the cases in New York represent the first outbreak of STEC O45 infections ever identified in the United States (2). During 1983--2002, public health laboratories submitted 940 non-O157 STEC isolates to CDC, of which 7% were identified as O45, making it the fifth most commonly isolated non-O157 STEC serogroup during that period (2). The outbreak in North Carolina illustrates the importance both of rapid culturing of all Stx-positive broths specifically for STEC O157 and of rapid culture confirmation of Stx-positive specimens. The initial Stx-positive result prompted public health actions that, in retrospect, placed an unnecessary burden on patients, day care center staff, and public health officials. Had a culture for E. coli O157 been performed simultaneously with the EIA or after the EIA was determined positive, the negative result might have prompted investigation for norovirus sooner. Once the EIA result was determined falsely positive, and the true etiology of the outbreak was determined, control measures appropriate for norovirus were instituted. This is not the first time that an outbreak of norovirus infections was mistakenly attributed to STEC (3). In 2000, non-O157 STEC infections became nationally notifiable. However, few non-O157 STEC infections are detected because most clinical diagnostic laboratories do not test stool specimens routinely for these organisms (4,5). No selective agar medium exists for isolation of non-O157 STEC. SMAC and other sorbitol-containing selective media such as cefixime-tellurite SMAC (CT-SMAC), Rainbow Agar O157, and CHROmagar O157 enhance isolation of STEC O157 because strains of this serotype typically do not ferment sorbitol or produce beta-D-glucuronidase. However, most non-O157 STEC strains ferment sorbitol and are phenotypically indistinguishable from other E. coli strains present in the normal intestinal flora. Non-O157 STEC infections can be diagnosed by use of EIA, PCR, or cell culture methods to detect free Stx or the stx1 or stx2 genes in stool or enrichment broths. EIA testing of broth cultures, rather than the stool specimens themselves, is recommended because the amount of free fecal Stx in stools often is low (6). Alternatively, production of Stx or the presence of Stx gene sequences can be demonstrated by selecting colonies from plating media and testing them by EIA or PCR. The development of commercial Stx EIA kits has allowed clinical diagnostic laboratories to easily screen stool specimens for STEC independent of serotype. If the index of clinical suspicion for STEC O157 is high, the stool specimen should be tested simultaneously by Stx EIA and by bacterial culture on a sorbitol-containing medium such as SMAC (7). Virulence factors strongly associated with the development of hemolytic uremic syndrome (HUS) are almost always present in STEC O157, but less frequently in non-O157 STEC (8). The majority of clinical diagnostic laboratories cannot determine the virulence profile of STEC but can identify an STEC O157 infection. Therefore, early diagnosis of at least STEC O157 is important to identify patients at highest risk for HUS. Treatment with parenteral-volume expansion early in the course of STEC O157 infection can decrease renal injury and improve patient outcome (9). Clinical diagnostic laboratories should strongly consider including STEC O157 in their routine bacterial enteric panel (with Salmonella, Shigella, and Campylobacter spp.). If bacterial culture for STEC O157 is not performed in parallel with EIA, Stx-positive broths should be inoculated to a selective isolation medium, such as SMAC agar, and any resulting sorbitol-negative colonies should be tested with O157 antiserum or latex reagent. All confirmed and presumptive STEC O157 isolates and Stx-positive broths that do not yield STEC O157 should be forwarded to a public health laboratory as soon as possible for confirmatory testing and further genetic characterization. STEC O157 isolates should be confirmed, characterized, and tested by PFGE, and the pattern promptly entered into the PulseNet database. At the public health laboratory, the broth should be subcultured to selective agar and a representative sample of sorbitol positive and negative colonies tested by Stx EIA or PCR for stx1 and stx2 genes. Non-O157 STEC isolates can be tested using commercial antisera for the most common non-O157 STEC serogroups (O26, O45, O103, O111, O121, and O145) and should be sent to the CDC E. coli Reference Laboratory for complete serotyping and further genetic characterization, including PFGE. To facilitate investigation of possible outbreaks, clinicians should inform health departments about clusters of patients with bloody diarrhea or HUS, and clinical diagnostic laboratories should follow recommended procedures for identification of STEC (Box). Screening stool specimens by clinical diagnostic laboratories for Stx using EIA, subsequent bacterial culture of Stx-positive specimens using SMAC, and forwarding enrichment broths from Stx-positive specimens that do not yield STEC O157 to state or local public health laboratories, are crucial steps for public health surveillance of STEC infections. With this coordinated approach, accurate laboratory data can be combined with epidemiologic information to ensure prompt diagnosis and treatment of STEC O157 infections, improved diagnostic accuracy, and improved detection of outbreaks caused by non-O157 STEC. Acknowledgments The findings in this report are based, in part, on contributions by M Caldwell, MD, A Evans, S Ireland, M DeFabio, Dutchess County Dept of Health, Poughkeepsie; L Klopf, MSEd, C Metzler, New York State Dept of Correctional Svcs; N Dumas, T Quinlan, L Armstrong, J Edwards, K Musser, PhD, R Limberger, PhD, New York State Dept of Health-Wadsworth Center; R Gallo, B Devine, New York State Dept of Health. B Jenkins, C Hartley, L Wolf, North Carolina State Laboratory of Public Health. S Rolando, MHS, Assoc of Public Health Laboratories, Silver Springs, Maryland. KG Holt, DVM, Food Safety and Inspection Svc, US Dept of Agriculture. References
Box 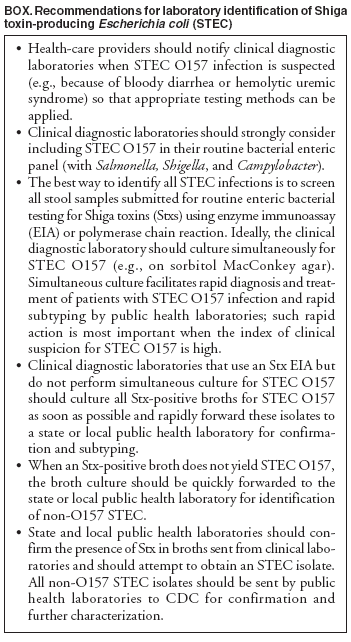 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 9/28/2006 |
|||||||||
|