Public Health Case Study 1: Malaria in Florida
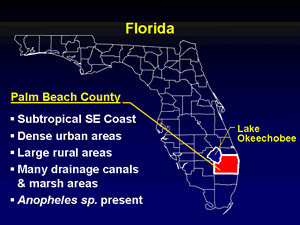
Palm Beach County, Florida
In Palm Beach County, Florida, during the summer of 2003 a cluster of eight cases of malaria was detected. The background incidence is 60 cases per year (Florida) and 10 cases per year (Palm Beach County).
All patients were infected by the same parasite species shown in the figure.
Question 1: What is the species?
Plasmodium falciparum
Plasmodium vivax
That is correct.
The figure shows two trophozoites, which exhibit a typical ameboid shape; and a schizont, which contains approximately 20 nuclei, compatible with P. vivax. The red blood cells infected with trophozoites contain Schüffner’s dots. The smears were prepared on blood that had been stored for several hours, thus their imperfect quality. One P. vivax characteristic that is absent here: the infected red cells are usually much more enlarged (1 1/4 to 2 times the size of non-infected red cells).
Plasmodium ovale
That is incorrect. Please, try another answer.
Plasmodium malariae
That is incorrect. Pleease, try another answer
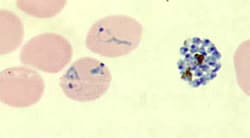
Blood smear from a patient in the Palm Beach County outbreak.
The patients were men whose ages varied from 17-45 (median 37). None had a history of prior malaria infection, recent history of travel in a malaria-endemic area, blood transfusion or organ transplantation or intravenous drug use. They were from diverse backgrounds, including one homeless man living near a drainage canal, two undocumented workers, and one affluent banker who liked to golf in the evening. All lived within 10 miles of Palm Beach International Airport.
Question 2: Among the modes of infection below, which one(s) need to be given the most serious consideration?
Infection during travel overseas
That is incorrect. Please, try another answer.
Blood transfusion/Transplantation
That is incorrect. Please, try another answer.
Needlestick contamination
That is incorrect. Please, try another answer.
Congenital malaria
That is incorrect. Please, try another answer.
Infection by local Anopheles mosquito
That is correct.
In any investigation of possible locally transmitted malaria, unreported travel to a malaria-endemic area must always be considered first. Often repeated questioning is required as well as inspection of travel documents such as passports in order to fully evaluate this possibility. With the large number of cases involved, unreported travel by all of the cases would have been unlikely, though.
Congenital malaria is excluded because of the patient’s ages. None of the patients had a compatible history of blood transfusion/transplantation or needle use.
The two most likely hypotheses would be “airport malaria” and infection by a local Anopheles mosquito. These hypotheses are compatible with the environmental conditions in Palm Beach County, favorable to mosquito breeding and survival, and with the fact that most patients had a history of outdoor exposure in the evenings or at night.
In the “airport malaria” scenario, an airplane may have carried a mosquito (or several mosquitoes) infected with malaria from a malaria-endemic area to Palm Beach International Airport. Upon arrival these mosquitoes may have transmitted malaria to local residents.
In the scenario involving local Anopheles, these mosquitoes would have become infected by feeding on an individual carrying malaria gametocytes (as a result of malaria infection acquired abroad). These now-infected mosquitoes then would have gone on to infect other local residents in Palm Beach County. These two hypotheses have significant public health implications because such infected Anopheles pose a risk to the general population.
“Airport Malaria”
That is correct.
In any investigation of possible locally transmitted malaria, unreported travel to a malaria-endemic area must always be considered first. Often repeated questioning is required as well as inspection of travel documents such as passports in order to fully evaluate this possibility. With the large number of cases involved, unreported travel by all of the cases would have been unlikely, though.
Congenital malaria is excluded because of the patient’s ages. None of the patients had a compatible history of blood transfusion/transplantation or needle use.
The two most likely hypotheses would be “airport malaria” and infection by a local Anopheles mosquito. These hypotheses are compatible with the environmental conditions in Palm Beach County, favorable to mosquito breeding and survival, and with the fact that most patients had a history of outdoor exposure in the evenings or at night.
In the “airport malaria” scenario, an airplane may have carried a mosquito (or several mosquitoes) infected with malaria from a malaria-endemic area to Palm Beach International Airport. Upon arrival these mosquitoes may have transmitted malaria to local residents.
In the scenario involving local Anopheles, these mosquitoes would have become infected by feeding on an individual carrying malaria gametocytes (as a result of malaria infection acquired abroad). These now-infected mosquitoes then would have gone on to infect other local residents in Palm Beach County. These two hypotheses have significant public health implications because such infected Anopheles pose a risk to the general population.
The dates of onset of symptoms, between July 12 and September 14, are shown in the epi curve.
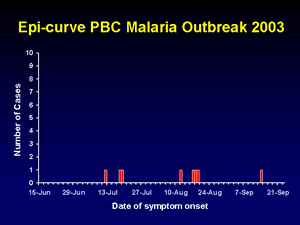
Epi curve of malaria cases, July - September 2003, Palm Beach County, Florida
Question 3: Based on that curve and what is known of the biology of P. vivax, the most likely occurrence is that all patients were infected by:
One individual Anopheles
That is incorrect. Please, try another answer.
Several Anopheles during a short time window (2 weeks or less)
That is incorrect. Please, try another answer.
Several Anopheles during a longer time window (more than 2 weeks)
That is correct.
Since P. vivax has an incubation period of 12-17 days, it is quite conceivable that there were several waves of infection, involving secondary transmission. In that scenario, the first patients were infected through the bites of local Anopheles. These patients later (after developing gametocytes) infected a second wave of mosquitoes, which, after a suitable maturation of the parasite (extrinsic cycle, duration 8-10 days), were able to infect the next wave of local residents. This scenario would have been possible by the semi-tropical conditions existing in Palm Beach County at that time of year. The first local mosquitoes to become infected would have fed on a gametocyte carrier whose infection would have been acquired abroad (returning traveler or migrant).
Given the extended duration of the outbreak, “airport malaria” is a less likely hypothesis because such outbreaks would be expected to be single source (and thus of shorter duration).
The microscopic diagnosis of P. vivax was confirmed by PCR. Parasite multilocus genotyping indicated that all parasites were the same strain, further supporting that the 8 infections originated from the same source. In that scenario, a person infected in an endemic country with P. vivax arrived in Palm Beach County and was bitten by local Anopheles mosquitoes, leading to the 2-3 cycles of local transmission in local residents (“autochthonous malaria”).
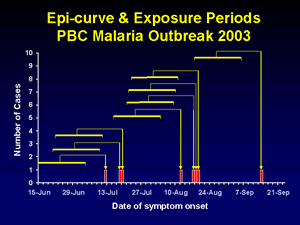
The epi curve shows three clusters of cases and exposure periods.
Question 4: What would be the next steps of the epidemiologic investigation? One or more answers may apply.
Search for additional cases (including possible index case) by blood surveys in 10% of the population
That is incorrect. Please, try another answer.
Search for additional cases (including possible index case) by review of medical/laboratory records and by surveillance for malaria and FUOs
That is correct.
An important next step consists of alerting the local health authorities and community, aiming to identify other infected individuals (especially if asymptomatic) and treating them to stop any further local transmission. In this outbreak this was done through the notification of local hospitals and health care providers, and community canvassing.
Review of hospital charts and facility records, though labor-intensive, is useful to identify any additional unreported cases of malaria or any missed cases (such as those with undiagnosed fever).
In the Palm Beach outbreak no additional cases nor index case was identified.
Blood surveys or surveys targeting immigrants would not have been practical nor helpful in this outbreak.
Confirmation of the presence of Anopheles and assessing their infection status would be interesting but not absolutely necessary. The entomological assessment and the appropriate level of activity is a highly debated topic. Trapping can identify the presence of competent vectors. But, this is often not necessary as areas that would be affected by such an outbreak will probably already have this data so additional trapping for this purpose can be a waste of resources. Trapping with the intent of identifying mosquitoes that contain the malaria parasite might also not be worthwhile. The setting of a small focus of infected mosquitoes as compared to a large background pool makes the finding of an infected mosquito highly improbable. And, as no test has perfect sensitivity and specificity, in this situation of such a low prevalence of infected mosquitoes, a positive test for the presence of malaria may be a false positive.
Search for additional cases (including possible index case) by canvassing community
That is correct.
An important next step consists of alerting the local health authorities and community, aiming to identify other infected individuals (especially if asymptomatic) and treating them to stop any further local transmission. In this outbreak this was done through the notification of local hospitals and health care providers, and community canvassing.
Review of hospital charts and facility records, though labor-intensive, is useful to identify any additional unreported cases of malaria or any missed cases (such as those with undiagnosed fever).
In the Palm Beach outbreak no additional cases nor index case was identified.
Blood surveys or surveys targeting immigrants would not have been practical nor helpful in this outbreak.
Confirmation of the presence of Anopheles and assessing their infection status would be interesting but not absolutely necessary. The entomological assessment and the appropriate level of activity is a highly debated topic. Trapping can identify the presence of competent vectors. But, this is often not necessary as areas that would be affected by such an outbreak will probably already have this data so additional trapping for this purpose can be a waste of resources. Trapping with the intent of identifying mosquitoes that contain the malaria parasite might also not be worthwhile. The setting of a small focus of infected mosquitoes as compared to a large background pool makes the finding of an infected mosquito highly improbable. And, as no test has perfect sensitivity and specificity, in this situation of such a low prevalence of infected mosquitoes, a positive test for the presence of malaria may be a false positive.
Search for additional cases (including possible index case) by screening immigrants and undocumented workers
That is incorrect. Please, try another answer.
Confirm presence of Anopheles in areas where the patients live
That is correct.
An important next step consists of alerting the local health authorities and community, aiming to identify other infected individuals (especially if asymptomatic) and treating them to stop any further local transmission. In this outbreak this was done through the notification of local hospitals and health care providers, and community canvassing.
Review of hospital charts and facility records, though labor-intensive, is useful to identify any additional unreported cases of malaria or any missed cases (such as those with undiagnosed fever).
In the Palm Beach outbreak no additional cases nor index case was identified.
Blood surveys or surveys targeting immigrants would not have been practical nor helpful in this outbreak.
Confirmation of the presence of Anopheles and assessing their infection status would be interesting but not absolutely necessary. The entomological assessment and the appropriate level of activity is a highly debated topic. Trapping can identify the presence of competent vectors. But, this is often not necessary as areas that would be affected by such an outbreak will probably already have this data so additional trapping for this purpose can be a waste of resources. Trapping with the intent of identifying mosquitoes that contain the malaria parasite might also not be worthwhile. The setting of a small focus of infected mosquitoes as compared to a large background pool makes the finding of an infected mosquito highly improbable. And, as no test has perfect sensitivity and specificity, in this situation of such a low prevalence of infected mosquitoes, a positive test for the presence of malaria may be a false positive.
Test local Anopheles for infection with malaria parasites
That is correct.
An important next step consists of alerting the local health authorities and community, aiming to identify other infected individuals (especially if asymptomatic) and treating them, to stop any further local transmission. In this outbreak this was done through the notification of local hospitals and health care providers, and community canvassing.
Review of hospital charts and facility records, though labor-intense, is useful to identify any additional unreported cases of malaria or any missed cases (such as those with undiagnosed fever).
In the Palm Beach outbreak no additional cases nor index case were identified.
Blood surveys or surveys targeting immigrants would not have been practical nor helpful in this outbreak.
Confirmation of the presence of Anopheles and assessing their infection status would be interesting but not absolutely necessary.The entomological assessment and the appropriate level of activity is a highly debated topic. Trapping can identify the presence of competent vectors. But, this is often not necessary as areas that would be affected by such an outbreak will probably already have this data so additional trapping for this purpose can be a waste of resources. Trapping with the intent of identifying mosquitoes that contain the malaria parasite might also not be worthwhile. The setting of a small focus of infected mosquitoes as compared to a large background pool makes the finding of an infected mosquito highly improbable. And, as no test has perfect sensitivity and specificity, in this situation of such a low prevalence of infected mosquitoes, a positive test for the presence of malaria may be a false positive.
Surveys of local health facilities and hospital charts, and community canvassing did not identify any additional cases, or index case.
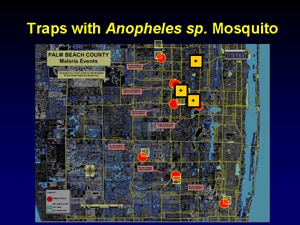
Mosquito traps placed near homes of 8 patients; in 3 locations Anopheles mosquitoes were caught
Mosquito traps were set within a one-mile radius of the homes of the patients, and Anopheles quadrimaculatus and An. crucians, both potential vectors of malaria, were found near at least 3 homes (figure). None of the mosquitoes were positive for malaria (by sporozoite ELISA).
In addition to the investigations described above, the local health authorities:
- Conducted sensitization campaigns in local communities, including groups at increased risk of infection (e.g., homeless camps)
- Intensified surveillance for suspected malaria at local health facilities (including hospitals and physician offices)
- Continued existing mosquito control practices, and conducted additional insecticide spraying (both ground and aerial) within a radius of 3 miles around the suspected transmission areas.
Main Points
In the United States, malaria has been eliminated but it can be reintroduced because travelers and immigrants may have malaria and local Anopheles mosquitoes can transmit malaria.
The risk is particularly high in areas where local climatic conditions allow survival of the Anopheles during a large part (or the totality) of the year, and where a large population of travelers or immigrants from endemic areas are found.
The most practical way to prevent re-introduction is through vigilant surveillance and investigations of all cases of malaria without known exposure (such as those described here).
Once local transmission is identified, aggressive surveys and canvassing of hospitals and communities are needed to identify and treat all cases, and thus interrupt local transmission.
Vector control measures (e.g., insecticide spraying) might play an additional, adjunct role.
That is incorrect. Please, try another answer.