COVID-19 Science Update released: September 4, 2020 Edition 45

The COVID-19 Science Update summarizes new and emerging scientific data for public health professionals to meet the challenges of this fast-moving pandemic. Weekly, staff from the CDC COVID-19 Response and the CDC Library systematically review literature in the WHO COVID-19 databaseexternal icon, and select publications and preprints for public health priority topics in the CDC Science Agenda for COVID-19 and CDC COVID-19 Response Health Equity Strategy.
Here you can find all previous COVID-19 Science Updates.
PEER-REVIEWED
Cluster of SARS-CoV-2 infections linked to music clubs in Osaka, Japan: Asymptomatically infected persons can transmit the virus as soon as 2 days after infection.external icon Sugano et al. Journal of Infectious Diseases. (August 25, 2020). Publishedexternal icon in Clinical Infectious Diseases (December 14, 2020).
Key findings:
- Asymptomatic persons with COVID-19 transmitted infection from 2–4 days after exposure.
- The period from exposure to symptom onset in 40 cases ranged from 2–17 days with a median of 7 days.
- 53% of cases attending only one music club were infected via transmission from asymptomatic persons.
Methods: Investigation of a cluster of 108 COVID-19 cases among persons visiting music clubs one or more times in February, 2020 (no mask use). Investigators focused on persons attending ≥2 clubs to determine period from exposure to ability to transmit SARS-CoV-2. Limitations: Information self-reported; genome sequencing not available; viral loads not assessed; exposure outside of clubs unknown.
Implications: Mitigation efforts, including avoiding crowding, improved ventilation, mask use, and hand hygiene are needed for effective control of COVID-19. Such short generation times (i.e., 2 days) may preclude usual contact tracing and require mass notification with precautionary quarantine to contain transmission.
Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19.external icon Garrigues et al. Journal of Infection. (August 25, 2020).
Key findings:
- The most frequently reported persistent symptoms were fatigue (55%), dyspnea (42%), loss of memory (34%) and concentration (28%) and sleep disorders (30.8%).
- Of persons working prior to COVID-19, 69% had returned to work.
- Except for pain, there was no statistically significant difference between ward and ICU groups.
Methods: Single-center study between March 15 and April 14, 2020 assessing persistent COVID-19 symptoms in 279 post-hospital discharge patients (mean 110.9 days after hospitalization) with phone questionnaire to assess post-discharge clinical symptoms and quality of life. Differences between ward and ICU patients were evaluated. Limitations: Limited sample size and response rate; single center.
Implications: Symptoms may persist after SARS-CoV-2 infection. For some COVID-19 patients, long-term follow-up and assessing their need for rehabilitation programs might be needed.
Key findings:
- 441 respondents reported moderate (274, 12.5%) or severe (167, 7.2%) symptoms of depression and/or anxiety in the previous two weeks during shutdown.
- Women were more likely than men to report depression and/or anxiety (51.6% vs 41%; p = 0.001).
- With adjustment for current social support and demographics, elevated risk for mild (aOR 1.65, 95% CI 1.06-2.57) and moderate (aOR 2.62, 95% CI 1.55-4.45) mental health symptoms was seen in persons with a history of intimate partner violence relative to those without.
- There was no association between time during shutdown and mental health symptoms.
Methods: Cross-sectional sample of 2,081 California adults over two weeks following the state stay-at-home order (enacted March 19, 2020). Logistic regression was used to assess associations between time in shutdown, history of partner and sexual violence, and severity of depression and/or anxiety. Limitations: Findings based on cross-sectional analyses; online rapid surveys might reduce inclusion of persons affected by mental health issues; current intimate partner violence not assessed.
Implications: COVID-19 and associated shutdowns might be associated with worsening mental health. Findings suggest the potential value of social support interventions.
PREPRINTS (NOT PEER-REVIEWED)
Assessment of the risk of SARS-CoV-2 reinfection in an intense re-exposure settingexternal icon. Abu-Raddad et al. medRxiv (August 26, 2020).
Key findings:
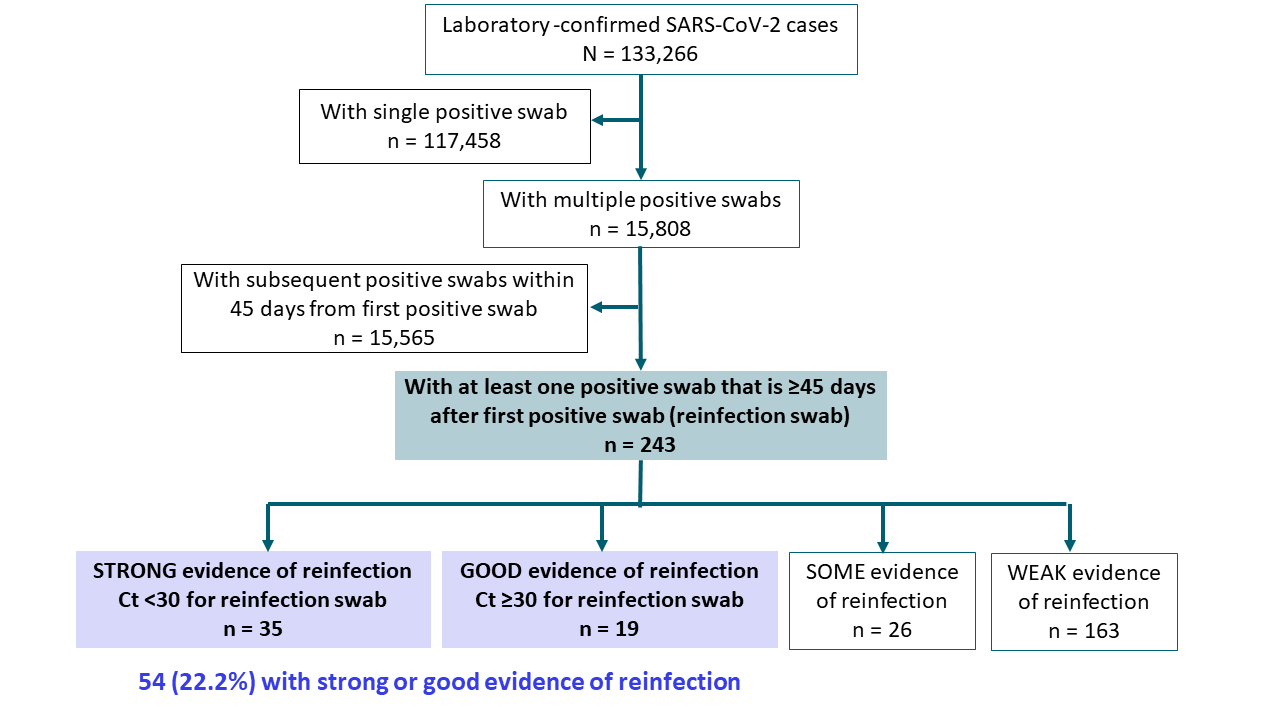
- 243 (0.18%) of 133,266 persons with laboratory-confirmed COVID-19 had at least one positive swab ≥45 days after the first positive swab; 54 (22.2%) had “strong” or “good” evidence of reinfection (Figure).
- Risk of reinfection estimated at 0.04% (95% CI 0.03%-0.05%); estimated incidence rate 1.09 (CI 0.84-1.42%) per 10,000 person-weeks.
Methods: Surveillance study in a high-prevalence population (Qatar) from February 2 to August 12, 2020 using a centralized, national database of SARS-CoV-2 cases. All laboratory-confirmed cases with at least 1 RT-PCR-positive test ≥45 days after initial positive test were investigated and classified by degree of evidence of reinfection: strong, good, some, or weak based on pattern and magnitude of the change in PCR Ct. Swabs with Ct <30 (suggestive of active recent infection) were considered strong evidence of reinfection. Limitations: Evidence of reinfection used epidemiological criteria based upon serial molecular testing only; viral culture, serial serology, and sequencing were not performed.
Implications: SARS-CoV-2 reinfection during the first few months post-primary infection appears to be rare. Standard criteria to determine what constitutes a reinfection is needed to guide investigations such as this.
Figure:
Note: Adapted from Abu-Raddad et al. Results of evaluation of reinfection status. Used by permission from the author.
Enhanced understanding of transmission patterns and the potential impact of respiratory viral infections are critical for prevention and management of COVID-19, seasonal influenza, and other respiratory infections.
PEER-REVIEWED
A. Rapid decline of seasonal influenza during the outbreak of COVID-19external icon. Young et al. European Respiratory Journal Open Research (August 17, 2020).
Key findings:
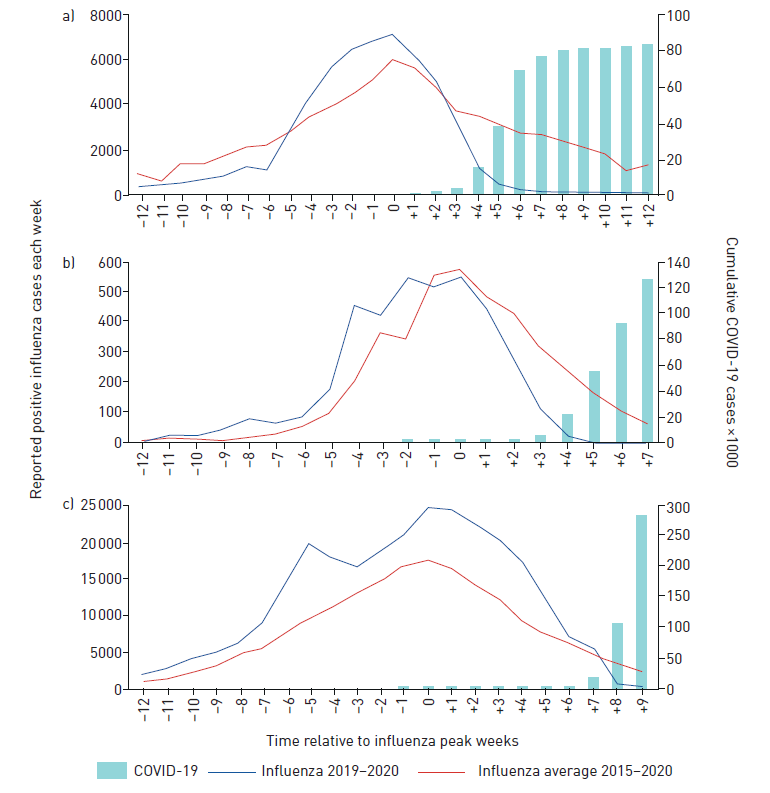
- In China and Italy, COVID-19 cases rose substantially within 4 weeks after the influenza peak, correlating with a steep decline in reported influenza cases compared to prior years (p = 0.004 and p = 0.001 for China (Figure a) and Italy (Figure b), respectively).
- The United States had a steeper decline in the 7 weeks following the influenza peak compared to prior years (p = 0.003).
- The delay in the COVID outbreak relative to China and Italy might have contributed to the later decline.
Methods: Influenza and COVID-19 incidence data for China, Italy, and the United States were obtained from the World Health Organization website. Rate of decline of influenza in each country was calculated using linear regression from the influenza peak to weeks 4 and 7 after the peak for the 2019/2020 season compared with 2015 to 2019 flu seasons. Limitations: Mechanisms explaining decline in influenza cases during the COVID-19 outbreak might be multifactorial; case data (both influenza and COVID-19) could be influenced by testing and reporting capacities in each country; coinfection data not provided.
Figure:
Note: Adapted from Young et al. Reported influenza cases in a) China, b) Italy and c) US in 2019/2020 compared to the mean for 2015–2019 influenza seasons in weeks prior to and following peak reporting. Influenza cases are shown on the left y-axis. COVID-19 cases are shown on the right y-axis. Licensed under CC BY-NC 4.0.
PREPRINTS (NOT PEER-REVIEWED)
B. Concomitant marked decline in prevalence of SARS-CoV-2 and other respiratory viruses among symptomatic patients following public health interventions in Australia: Data from St Vincent’s Hospital and associated screening clinics, Sydney, NSWexternal icon. Marriott et al. Clinical Infectious Diseases (August 25, 2020).
Key findings:
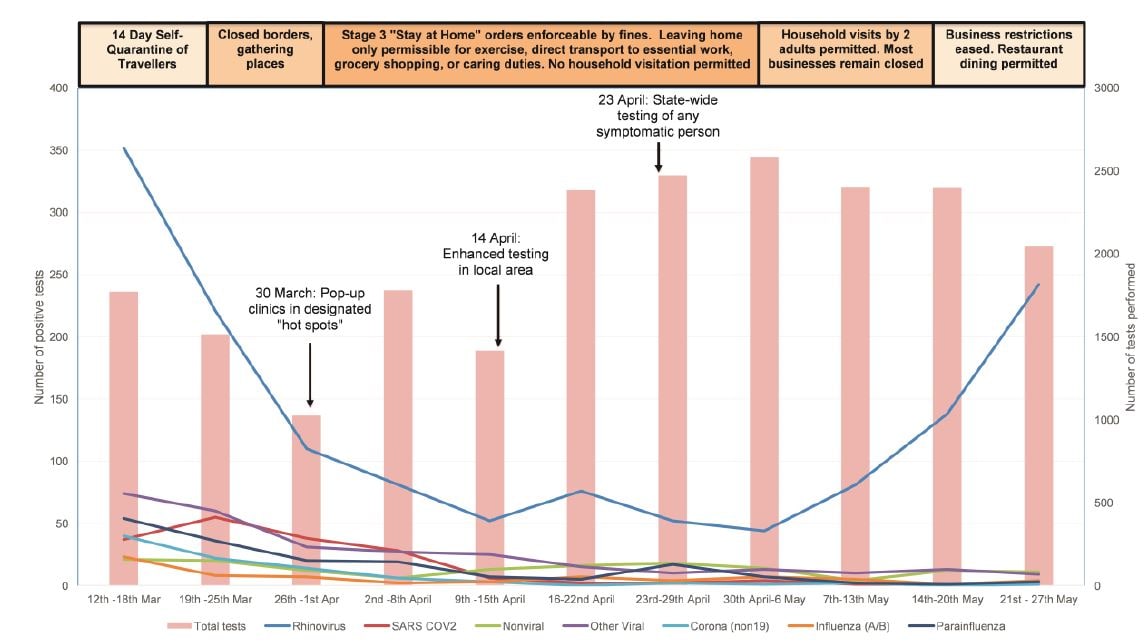
- The proportion of persons testing positive for any respiratory pathogen declined markedly, from 32.5% in week one to 3.1% in week eight following travel bans and physical distancing, and rising again to 12.9% in week 11 as social control measures were relaxed (p <0.001 for each subsequent week, compared to baseline), (Figure).
- Rhinovirus declined from 19.9% to 1.7%, then rose again to 11.8% by late May.
- Parainfluenza declined from 3.0% to 0.1%.
- Non-SARS-COV-2 coronaviruses declined from 2.3% to <0.1%.
- Among persons with SARS-CoV-2, 5% had co-infection with other respiratory pathogens, rhinovirus most commonly. No persons were coinfected with SARS-CoV-2 and other non-pandemic coronaviruses.
Methods: Australian study of 21,808 persons with respiratory symptoms, contact with persons with SARS-CoV-2, or who were healthcare workers tested between March 12 and May 27, 2020. Testing for SARS-CoV-2 and other respiratory infections was performed with a multiplex PCR assay during introduction and subsequent relaxation of social and physical protection controls. Limitations: SARS-CoV-2 testing criteria changed during the study period; results might not be generalizable; unable to determine which protective measures affected epidemiology of infection; limited co-infection data.
Figure:
Note: From Marriot et al. Positive results on multiplex PCR by study week. The left y-axis is number of positive NP swabs for each respiratory pathogen as indicated by colored lines. The right y-axis is number of NP swabs performed on unique patients. Nonviral pathogens include Bordetella pertussis, Mycoplasma pneumoniae, and Pneumocystis jirovecii. Other Viral pathogens include adenoviruses, enteroviruses, respiratory syncytial virus, and human metapneumovirus. Reproduced by permission of Oxford University Press on behalf of the Infectious Diseases Society of America. Please visit: https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa1256/5897048external icon
Implications of both studies (Young et al. & Marriot et al.): These studies as well as a Research Letter by Wong et al. demonstrate that implementation of protective measures during the COVID-19 pandemic might have had an important impact on prevalence of respiratory infections, including seasonal influenza and SARS-CoV-2. Changes in the prevalence of circulating respiratory viruses might provide a useful indicator of success of ongoing measures, including physical distancing restrictions.
PEER-REVIEWED
Duration of infectiousness and correlation with RT-PCR cycle threshold values in cases of COVID-19, England, January to May 2020external icon. Singanayagam et al. Eurosurveillance. (August 13, 2020).
Key findings:
- Median duration of virus shedding by culture after symptom onset was 4 days.
- The culture-positivity rate peaked at symptom onset and was significantly higher during week 1 than week 2 (74% vs 20%, p = 0.002).
- Ten days after symptom onset, the probability of culturing virus declined to 6.0% (95% CI 0.9%-31.2%).
- Samples taken during the presymptomatic phase were as likely to be culture-positive as those taken during the symptomatic phase.
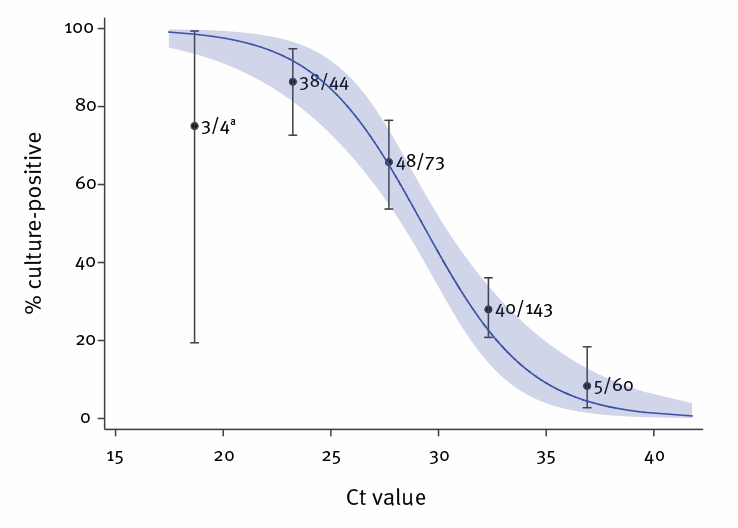
- The ability to recover infectious virus was strongly related to Ct value, as the estimated OR of finding infectious virus decreased by 0.67 for every unit increase in Ct value (Figure).
- There was no difference in Ct values in those with asymptomatic, mild-to-moderate, or severe illness (p = 0.79).
Methods: Analysis of upper respiratory tract specimens collected between January and April 2020 from 425 symptomatic and 62 asymptomatic persons. RT-PCR Ct values were related to viral culture. Limitations: Recall bias on date of symptom onset might have influenced the relation of virus detection to symptom onset; virus culture is dependent on technical factors that might limit comparability to data from other labs; nonsystematic sampling; only 8% had severe disease.
Implications: All persons with COVID-19 regardless of symptoms may transmit infection. Based on the data presented here on the presence of culturable virus, transmission is most likely during the period from symptom onset through 10 days after symptom onset. Further studies are needed on the dynamics of transmission, especially for persons with asymptomatic infection.
Figure:
Note: From Singanayagam et al. Relationship between RT-PCR Ct value and culture positivity in mixed effects logistic regression analysis. Licensed under CC-BY.
PREPRINTS (NOT PEER-REVIEWED)
SARS-CoV-2 specific memory B cells frequency in recovered patient remains stable while antibodies decay over timeexternal icon. Vaisman-Mentesh et al. medRxiv (August 25, 2020).
Key findings:
- Receptor binding domain (RBD)-specific memory B cells were stable over six months in recovered patients, whereas antibody levels declined (Figure 1).
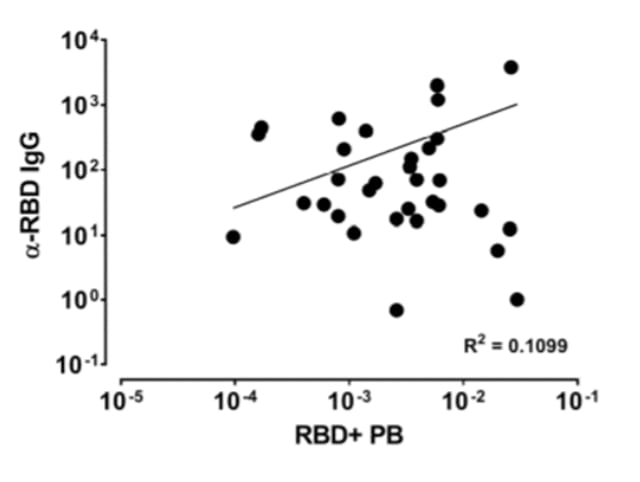
- Frequency of SARS-CoV-2-specific B cell plasmablasts (activated B cells) were correlated with IgG levels (Figure 2).
Methods: Blood samples from 54 patients with symptomatic COVID-19, 57 recovered COVID-19 patients, and 26 healthy controls were tested by ELISA to determine the levels of RBD-specific antibodies (IgG, IgM, and IgA). Memory B cells were isolated from plasmablasts in recovered patients. Limitations: Follow-up period limited generalizability; some analyses limited to subsets of patients.
Implications: Memory B cells may indicate protection against SARS-CoV-2 reinfection. Long-term follow-up of recovered patients may inform the duration of protection.
Figure 1
Note: Adapted from Vaisman-Mentesh et al. A: RBD-specific memory B cell levels in 30 patients over 6 months after symptom onset. B: Antibody levels in 51 patients after symptom onset. mBC – memory B cells. RBD- receptor-binding domain; Rs-Spearman rank correlation coefficient. Licensed under CC 4.0.
Note: Adapted from Vaisman-Mentesh et al. Correlation between memory B cell plasmablasts and level of IgG in 31 patients. RBD-receptor-binding domain; PB-plasmablast; R2-variance from Spearman correlation (R = 0.3315). Licensed under CC 4.0
Clinical Treatment and Outcomes
- Shanbhag et al. COVID-19 presenting as severe rhabdomyolysis with normal renal functionexternal icon. A young adult with a previous history of influenza-associated rhabdomyolysis developed COVID-19-associated rhabdomyolysis while maintaining normal renal function and urine output.
- Busani et al. Two fatal cases of acute liver failure due to HSV-1 infection in COVID-19 patients following immunomodulatory therapies.external icon Clinical Infectious Diseases. Two adults developed fatal liver failure caused by Herpes Simplex Virus-1 after treatment of SARS-CoV-2-associated respiratory failure with tocilizumab, an interleuken-6 receptor antagonist.
New Tools for Policy and Practice
- Slaoui et al. Developing safe and effective COVID vaccines — Operation Warp Speed’s Strategy and Approach.external icon Operation Warp Speed’s process to safely and effectively demonstrate strategies for delivering 300 million safe and effective vaccine doses by mid-2021.
- Jones et al. Two metres or one: what is the evidence for physical distancing in COVID-19?external icon Reviews evidence behind the recommendation for 2 meters (6 feet) of physical distancing and suggests a nuanced approach to distancing based on the type and location of the activity.
- Delaunay et al. Evaluation of testing frequency and sampling for SARS-CoV-2 surveillance strategies in long-term care facilities.external icon Journal of the American Medical Directors Association. Models optimal testing in long-term care facilities for settings of low transmission as weekly testing of 50% of asymptomatic residents and staff.
- Rhee et al. Duration of SARS-CoV-2 infectivity: When is it safe to discontinue isolation?external icon Clinical Infectious Diseases. Evidence that most infected persons are most contagious right before and after symptom onset; for mild to moderate infection, duration of infectiousness is about 10 days after symptom onset.
- Buntin et al. Safely reopening schools—Learning amid a pandemic.external icon Outline of several interventions to facilitate safe school reopening, including mask wearing, grouping small numbers of students together, and changing absence policies.
Immunology
- Takahashi et al. Sex differences in immune responses that underlie COVID-19 disease outcomes.external icon Certain cytokines and chemokines were higher in males infected with SARS-CoV-2; T-cell activation was greater in women infected with SARS-CoV-2.
Respiratory Viruses
- Wong et al. Abrupt subsidence of seasonal influenza after coronavirus disease outbreak, Hong Kong, China. Emerging Infectious Diseases. Social distancing interventions undertaken to halt the spread of COVID-19 correlated with rapid reduction of influenza A and B infections in Hong Kong, China.
- Singh et al. COVID-19 and influenza co-infection: Report of three cases.external icon Three adult patients with SARS-CoV-2 and influenza coinfection are described, including clinical presentation, treatment, and outcomes.
Disclaimer: The purpose of the CDC COVID-19 Science Update is to share public health articles with public health agencies and departments for informational and educational purposes. Materials listed in this Science Update are selected to provide awareness of relevant public health literature. A material’s inclusion and the material itself provided here in full or in part, does not necessarily represent the views of the U.S. Department of Health and Human Services or the CDC, nor does it necessarily imply endorsement of methods or findings. While much of the COVID-19 literature is open access or otherwise freely available, it is the responsibility of the third-party user to determine whether any intellectual property rights govern the use of materials in this Science Update prior to use or distribution. Findings are based on research available at the time of this publication and may be subject to change.