COVID-19 Science Update released: July 17, 2020 Edition 31

The COVID-19 Science Update summarizes new and emerging scientific data for public health professionals to meet the challenges of this fast-moving pandemic. Weekly, staff from the CDC COVID-19 Response and the CDC Library systematically review literature in the WHO COVID-19 databaseexternal icon, and select publications and preprints for public health priority topics in the CDC Science Agenda for COVID-19 and CDC COVID-19 Response Health Equity Strategy.
Here you can find all previous COVID-19 Science Updates.
Pregnant women may not be more susceptible to SARS-CoV-2 infection than other women but may be more at risk of severe illness or complications due to pregnancy. Our understanding of the effects of the virus on fetal and newborn health continue to evolve. These two reports describe ways that COVID-19 may impact health and post-partum outcomes among pregnant women and their newborn children.
PEER-REVIEWED
A. Pregnancy and postpartum outcomes in a universally tested population for SARS-CoV-2 in New York City: A prospective cohort studyexternal icon. Prabhu et al. International Journal of Obstetrics & Gynaecology (July 7, 2020).
Key findings:
- 4% of pregnant women tested positive for SARS-CoV-2 at labor and delivery admission;
- Of positive cases, 78.6% were asymptomatic; new symptoms/clinical worsening occurred post-partum among 13%.
- Black and Hispanic women comprised larger proportions of women diagnosed with COVID-19
- 7% with COVID-19 were Black vs 4.1% without COVID-19.
- 1% with COVID-19 were Hispanic vs 8.3% without COVID-19.
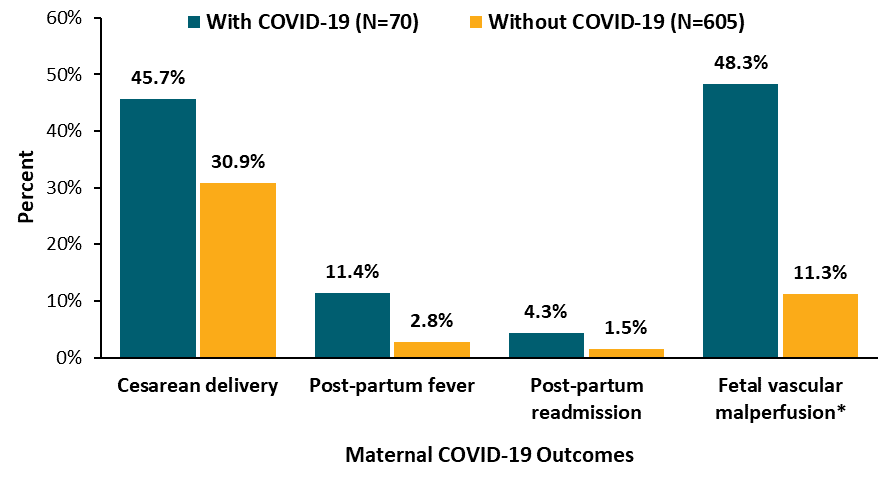
- Women with COVID-19 had higher rates of Cesarean delivery (45.7% with COVID-19 vs 30.9% without) and post-partum complications such as fever, hypoxia, and readmission (12.9% with COVID-19 vs 4.5% without) (Figure). None died.
- 71 of 73 infants born to women with COVID-19 were tested for SARS-CoV-2; none was positive. However, maternal COVID-19 was associated with fetal vascular malperfusion (48.3% with COVID-19 vs 11.3% without) (Figure).
Methods: Prospective cohort study of 675 pregnant women tested for SARS-CoV-2 and their infants, March 24-April 20, 2020. Study examined maternal SARS-CoV-2 prevalence and outcomes, neonatal outcomes, and placental pathology. Limitations: Possible biases in self-reported symptoms; high rates of missing data for race/ethnicity; only 1 site assessed placental pathology.
Figure:
Note: Adapted from Prabhu et al. Pregnant women with COVID-19 at delivery were more likely to experience Cesarean delivery, post-partum fever, hypoxia (n = 3, data not shown) and re-admission than women without COVID-19; *In one of three clinics, placental analysis showed higher rate of fetal vascular malperfusion associated with COVID-19 (48.3% of 29 cases vs 11.3% of 106 cases). Available via Wiley Public Health Emergency Collection through PubMed Central.
B. Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: national population based cohort studyexternal icon. Knight et al. BMJ (June 8, 2020).
Key findings:
- 10% of pregnant women admitted with SARS-CoV-2 infection needed respiratory support, and 5 (1%) died.
- Pre-term loss (n = 4), stillbirth (n = 3), or neonatal death (n = 2) was experienced by 2.1%.
- 59% of 266 women who gave birth did so via Cesarean delivery.
- 3 died from complications of COVID-19 and two from other causes.
- 56% were from Black or other racial/ethnic minority groups.
- 5% of 265 infants were positive for SARS CoV-2; 25% were admitted to neonatal unit, primarily due to pre-term birth. One was diagnosed with neonatal encephalopathy.
Methods: Prospective national cohort study of 427 pregnant women hospitalized with SARS-CoV-2 infection, between March 1 and April 14, 2020 that examined incidence of maternal hospital admission, infant infection and maternal and neonatal outcomes: 266 women gave birth during the study period. Testing for women and infants performed on blood, NP, or aspirate (infants only) samples; women were also defined as infected if they showed respiratory compromise along with radiographic changes characteristic of COVID-19. Limitations: Complete pregnancy/neonatal outcomes were not available due to the short timeframe; no comparison to uninfected population; women were tested only if symptomatic.
Implications for 2 studies (Prabhu et al. and Knight et al.): There is a disproportionate burden of COVID-19 among pregnant women from Black and other racial/ethnic minority groups though SARS-CoV-2 transmission to infants appears to be infrequent. Compared with uninfected pregnant women, those with COVID-19 had higher rates of post-partum complications and fetal vascular malperfusion.
Obesity, particularly severe obesity, is a plausible risk factor for complications associated with COVID-19. Patients who are underweight might also suffer higher rates of complications. Below we summarize two cohorts of patients hospitalized with COVID-19 in which obesity and underweight status were assessed as risk factors for mortality and severe morbidity.
PEER-REVIEWED
A. How important is obesity as a risk factor for respiratory failure, intensive care admission and death in hospitalised COVID-19 patients? Results from a single Italian centreexternal icon. Rottoli et al. European Journal of Endocrinology (July 1, 2020).
Key findings:
- Obesity (body mass index (BMI) ≥30 kg/m2) significantly increased the risk of:
- Respiratory failure (odds ratio [OR] 2.48, 95%CI 1.46-4.21; p = 0.001).
- Admission to the intensive care unit (ICU) (OR 5.28, 95% CI 2.81-9.91; p <0.001).
- Death (OR 2.35, 95% CI 1.17-4.75; p = 0.017).
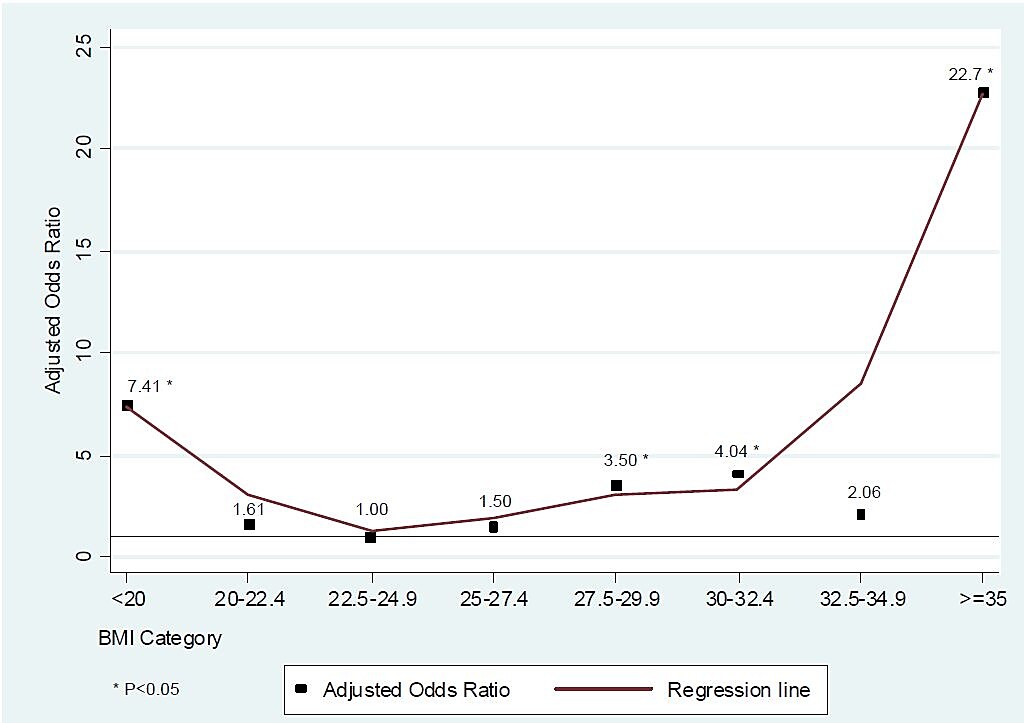
- Risk of death was significantly higher among patients with a BMI ≥35 kg/m2 and patients with a BMI <20 kg/m2 (Figure)
Methods: Retrospective cohort study of 482 consecutive COVID-19 patients, positive by RT-PCR, hospitalized during March 1-April 20, 2020 with BMI data available. Logistic regression analysis and Cox proportion Hazard models including demographic characteristics and comorbidities were carried out to predict the endpoints (onset of respiratory failure, admission to ICU and mortality) within 30 days of follow-up from symptom onset. Limitations: Not clear if weight was at time of admission or before symptom onset; participants from only one hospital; majority of patients are of Caucasian ethnicity.
Figure:
Note: From Rottoli et al. Adjusted odds ratios of categories of BMI versus a reference category (BMI 22.5-24.9) for the risk of death during follow-up. Republished with permission of Bioscientific Limited; permission conveyed through Copyright Clearance Center, Inc.
B. Obesity and COVID-19 in New York City: A retrospective cohort studyexternal icon. Goyal et al. Annals of Internal Medicine (July 6, 2020)
Key findings:
- Among patients hospitalized for COVID-19:
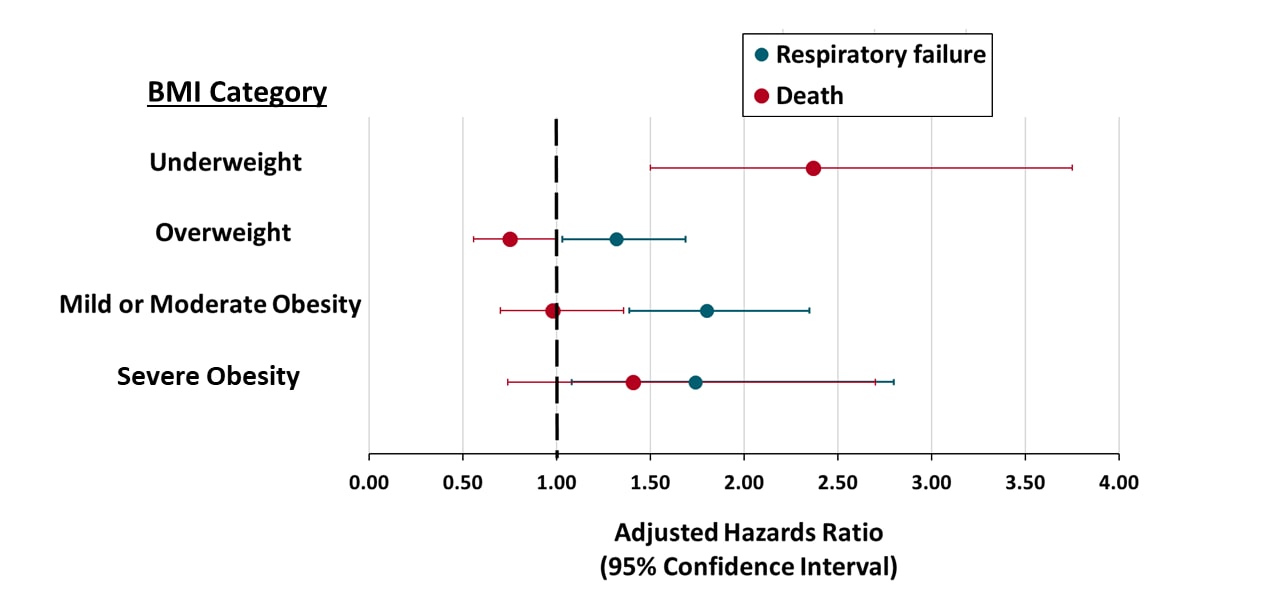
- Overweight and obesity categories were independent risk factors for respiratory failure, compared with normal body mass index (BMI) (Figure).
- BMI in the underweight range was associated with mortality (Figure).
- Median age of severely (“morbidly” in Goyal et al.) obese patients was younger (52.1 years) compared with other patients.
Methods: Retrospective observational cohort study of 1,687 hospitalized adult COVID-19 patients from 2 New York City hospitals, March 3-May 15, 2020. BMI was categorized as underweight (<18.5 kg/m2), normal (18.5-24.9 kg/m2), overweight (25.0-29.9 kg/m2), mild to moderate obesity (30.0-39.9 kg/m2), and severe obesity (≥40.0 kg/m2). Cox proportional hazard ratio model was used to assess the association of BMI to respiratory failure and mortality. Limitations: One location in the US.
Figure:
Note: Adapted from Goyal et al. Adjusted hazards ratio for hospitalized COVID-19 patients and outcome of respiratory failure and death compared with normal BMI. Data on hazards ratio for underweight and respiratory failure not available due to low case count. Available via American College of Physicians Public Health Emergency Collection through PubMed Central.
Implications for 2 studies (Rottoli et al. & Goyal et al.): In two studies based on hospitalized populations from two countries with differing population social and demographic characteristics, BMI greater than “normal” was associated with respiratory failure among COVID-19 patients. In both studies, as the level of BMI rose, the risk for mortality increased; this effect was more pronounced in Rottoli et al. Both studies found an association between underweight status and death.
PEER-REVIEWED
COVID-19 cases and deaths in federal and state prisonsexternal icon. Saloner et al. JAMA (July 8, 2020).
Key findings:
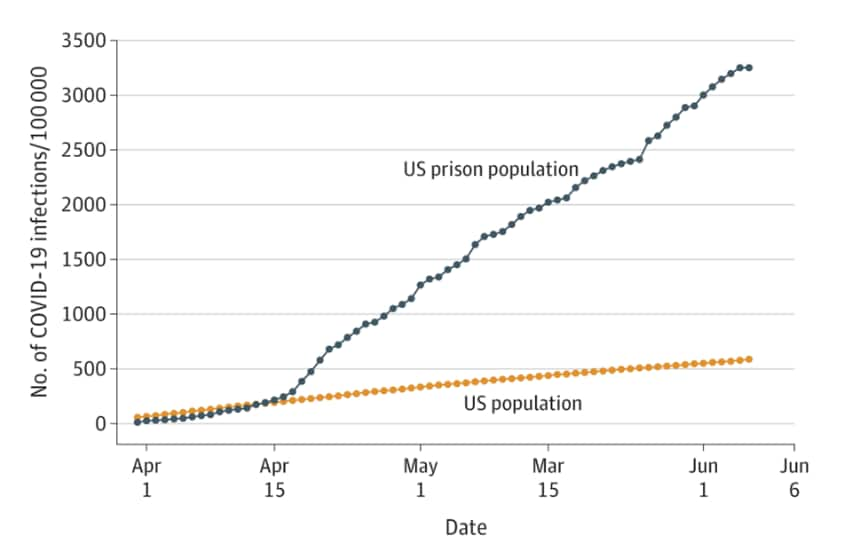
- 42,107 cases of COVID-19 were reported among prisoners:
- Case rate for prisoners (3,251 per 100,000) was 5.5 times higher than the US general population (587 per 100,000) (Figure).
- 510 prisoner deaths due to COVID-19 were reported:
- Crude death rate was 39 deaths per 100,000 prisoners (compared with the US population rate of 29 deaths per 100,000).
- Controlling for age and gender, the death rate was 3.0 times higher among prisoners than the rest of the US. population.
- Over the study period, mean daily case growth rate was 8.3% per day in prisons compared with 3.4 % per day in the US population (Figure).
Methods: Reported COVID-19 cases and presumed or confirmed deaths March 31-June 6, 2020 were used to calculate cumulative cases, case rates and deaths among federal and state prisoners. Limitations: Reported data may be subject to inaccuracies and delays; prison-based testing data not available; other types of detention facilities (e.g., jails) were not included.
Implications: COVID-19 case rates and deaths have been substantially higher and escalated more rapidly in prisons than in the US population. Improved infection prevention and control efforts can reduce transmission in these settings.
Figure:
Note: Adapted from Saloner et al. Trends in cumulative COVID-19 case rate per 100,000 people for state and federal prisons and US population. The COVID-19 case rate in prisons surpassed the US population on April 14, 2020. Reproduced with permission from JAMA. doi:10.1001/jama.2020.12528. Copyright©2020 American Medical Association. All rights reserved.
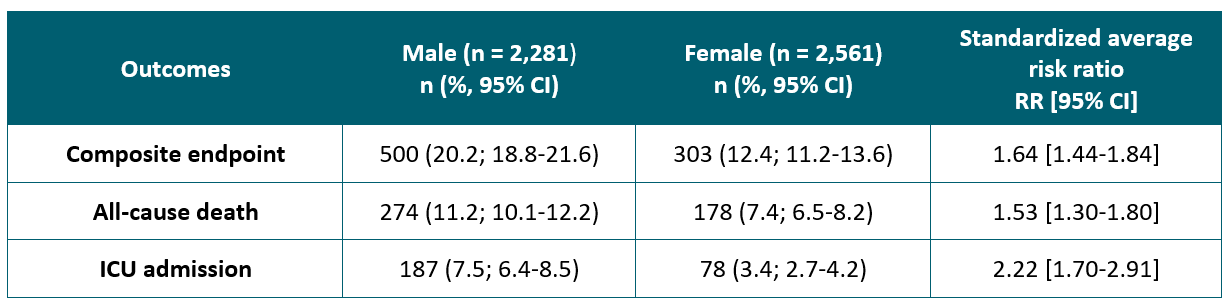
Association between male sex and outcomes of coronavirus disease 2019 (COVID-19) – A Danish nationwide, register-based studyexternal icon. Kragholm et al. Clinical Infectious Diseases (July 8, 2020).
Key findings:
- The risks for the 30-day composite outcome for men and women were 20.2% and 12.4%, respectively (Table).
- Male sex was significantly associated with all-cause death and ICU admission within 30 days after COVID-19 diagnosis compared with female sex (Table).
Methods: Nationwide registry-based follow-up study of 4,842 COVID-19 patients (2,281 male, 2,561 female) comparing 30-day composite outcome of all-cause death, severe COVID-19 diagnosis or intensive care unit (ICU) admission for men versus women, adjusted for age and comorbidity. Limitations: Non-randomized study; short study follow-up period.
Implications: Men with SARS-Cov-2 infection have greater mortality than do women. The excess risk was not explained by age and comorbidities.
Table:
Note: Adapted from Kragholm et al. Percent estimates, risk ratios, and 95% confidence intervals are adjusted for age and comorbidities. Reproduced by permission of Oxford University Press on behalf of the Infectious Diseases Society of America. Please visit: https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa924/5868546external icon.
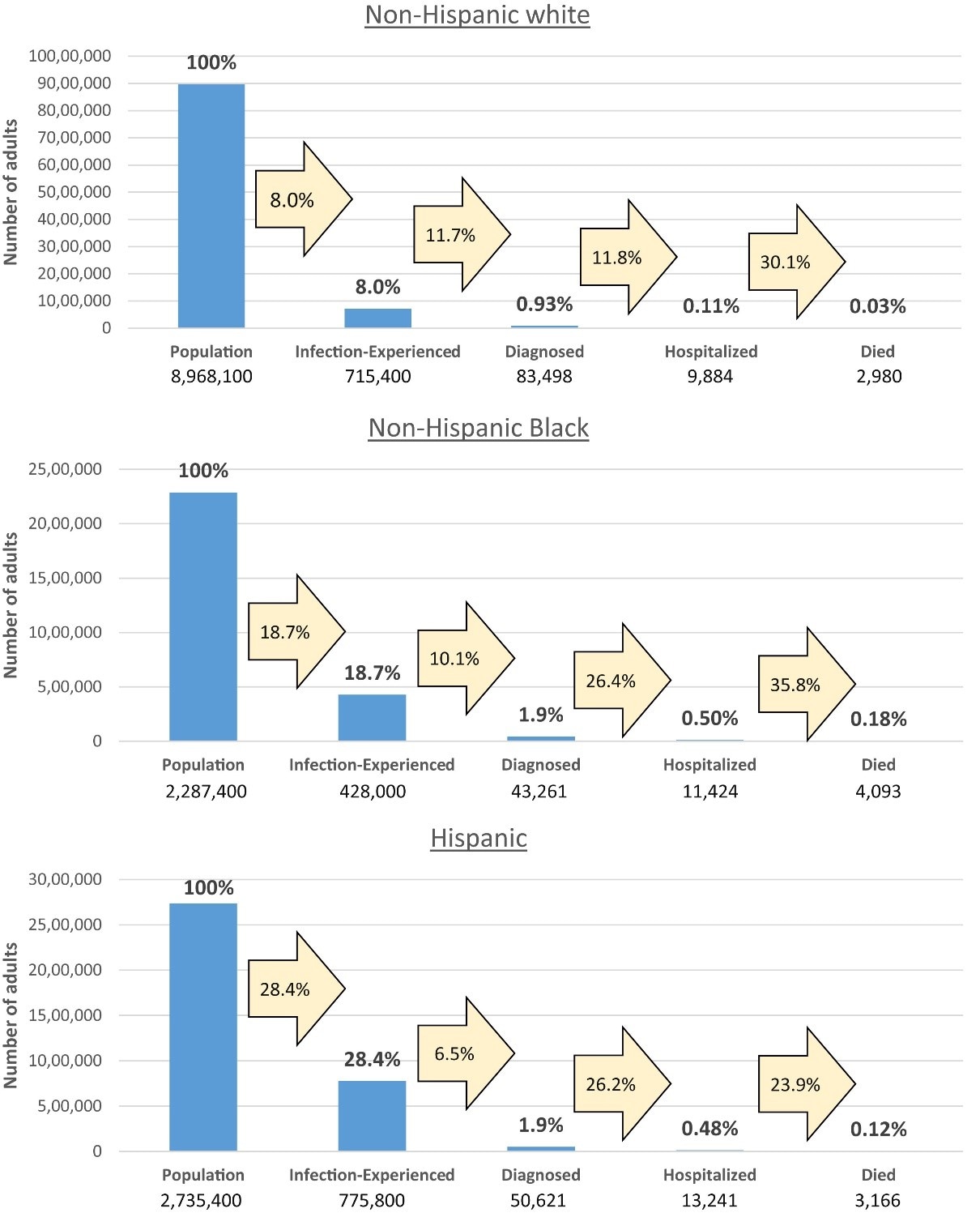
Assessing racial and ethnic disparities using a COVID-19 outcomes continuum for New York Stateexternal icon. Holtgrave et al. Annals of Epidemiology (June 20, 2020).
Key findings:
- Authors estimated 8.0% of White non-Hispanic, 18.7% of Black non-Hispanic, and 28.4% of Hispanic adults were infected with SARS-CoV-2.
- Compared with white non-Hispanics, Black non-Hispanic and Hispanic populations had higher proportions of COVID-19 diagnosis, hospitalization and death (Figure).
- Black non-Hispanic adults were 5.4 times, and Hispanic adults were 3.5 times more likely to die of COVID-19 compared with white non-Hispanic adults.
- Black non-Hispanic adults were 4.5 times, and Hispanic adults were 4.4. times more likely to be hospitalized as a result of COVID-19 compared with white non-Hispanic adults.
Methods: Evaluation of race and ethnicity, COVID-19 incidence and diagnosis, hospitalization, and fatality using an outcomes continuum of data from public and peer-reviewed data sources, New York State. Limitations: Data sources varied, race and ethnicity data were incomplete, estimates are not adjusted for factors such as comorbidities.
Implications: COVID-19 outcomes examined by race and ethnicity may be useful to identify health disparities and focus efforts to mitigate them.
Figure:
Note: Adapted from Holtgrave et al. Disparities in COVID-19 outcomes by race and ethnicity across a continuum of outcomes from infection to mortality. Blue histogram bars indicate the proportion of each race and ethnic subpopulation counted at each stage on the continuum; numbers inside beige arrows represent the proportion of people who moved from one stage to the next. This article was published in Annals of Epidemiology, Vol 48, Holtgrave et al., Assessing racial and ethnic disparities using a COVID-19 outcomes continuum for New York State, Page 9-14, Copyright Elsevier 2020. This article is currently available at the Elsevier COVID-19 resource center: https://www.elsevier.com/connect/coronavirus-information-centerexternal icon.
PREPRINTS (NOT PEER-REVIEWED)
Exposure assessment for airborne transmission of SARS-CoV-2 via breathing, speaking, coughing and sneezingexternal icon. Schijven et al. medRxiv (July 5, 2020).
Key findings:
- Calculated quantity of aerosols in descending order: sneezing once, coughing once, speaking for 20 minutes, and breathing for 20 minutes.
- Model results suggest exposure to SARS-CoV-2 via aerosols is possible, and exposure risk is increased in unventilated or indoor environments.
- Exposure probability strongly depends on the viral concentration in mucus and modeled scenario.
Methods: Exposure assessment model to estimate number of SARS-CoV-2 particles in aerosol droplets expelled during breathing, speaking, coughing, and sneezing in an unventilated indoor environment, and inhaled by one or more person with varying virus concentration, room size, and exposure time. Model inputs included published parameters of virus concentration, volume of aerosol droplets, and dose and exposure probabilities. Limitations: Assumed aerosol spread is constant over time and space; infectiousness of viral particles and dose response relationship not known.
Implications: Aerosol transmission of SARS-CoV-2 may be possible and should be considered in mitigation strategies and recommendations. Data on infectious virus in aerosols in various settings are needed to validate modelling efforts.
PEER-REVIEWED
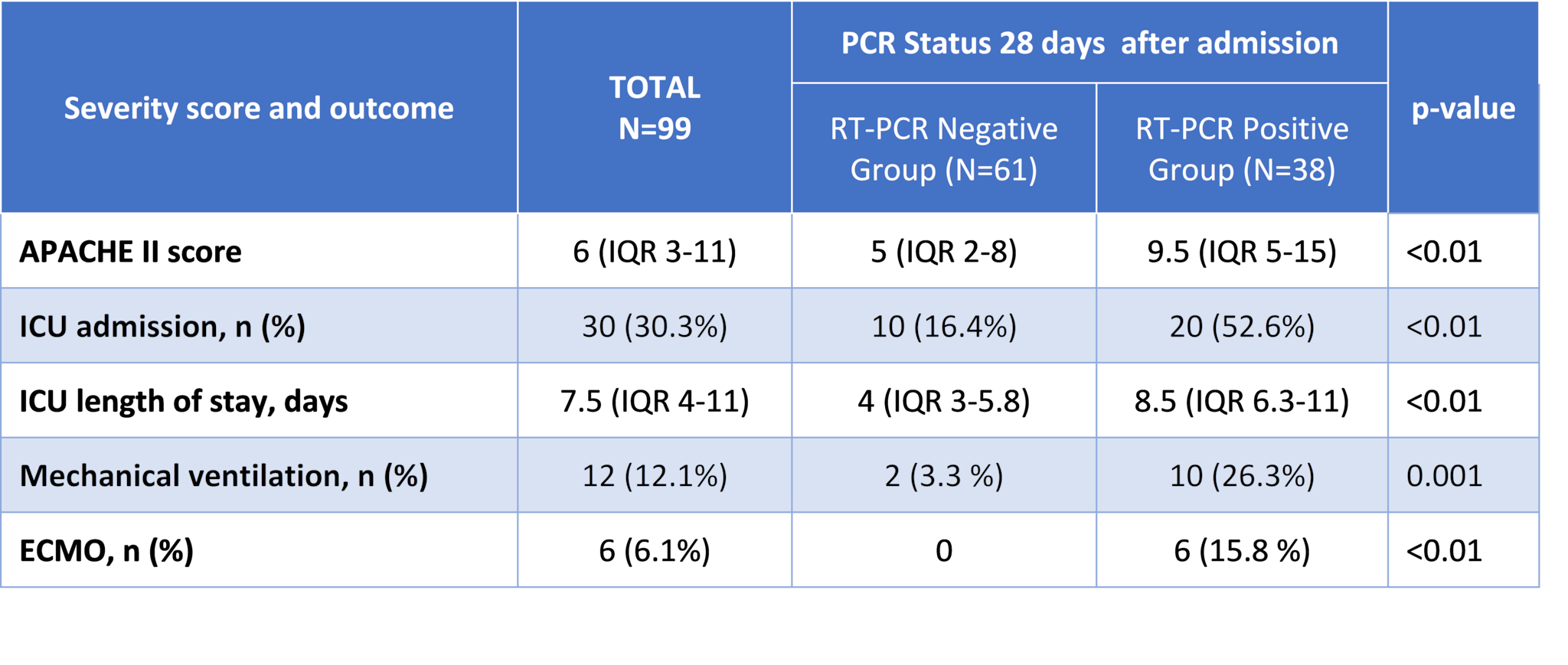
Clinical characteristics and factors associated with long-term viral excretion in patients with SARS-CoV-2 infection: a single center 28-day studyexternal icon. Shi et al. Journal of Infectious Diseases (July 2, 2020).
Key findings:
- 38 patients (38.4%) had positive RT-PCR results 28 days post-admission.
- Patients with persistent SARS-CoV-2 RNA positivity showed greater disease severity (Table).
- Male sex, immunoglobulin use, Acute Physiology and Chronic Health Evaluation II (APACHE II) score, and lymphocyte count <0.5×109/L were independent factors associated with prolonged SARS-CoV-2 RNA shedding, but not antiviral or corticosteroid therapy.
- Patients with fecal viral RNA-positivity had longer delay in viral RNA clearance from respiratory specimens.
Methods: Retrospective cohort study of 99 hospitalized COVID-19 patients. NP, sputum, or endotracheal aspirate and stool samples for PCR testing were collected daily for 28 days. Hazard ratios were estimated to evaluate factors associated with SARS-CoV-2 RNA shedding. Cessation of RNA shedding was defined as the occurrence of 2 consecutive RT-PCR negative results. Limitations: Short observation time; hospitalized patients likely represent more severe COVID-19; retrospective data collection; did not conduct viral cultures to assess if persistence of viral RNA was indicative of live virus or infectiousness.
Implications: SARS-CoV-2 RNA clearance time was associated with sex, immunoglobulin use, disease severity, and lymphocyte count and may be related to host immune response and inflammatory activation.
Table:
Note: Adapted from Shi et al. During hospitalization, 61 patients had respiratory specimens negative for SARS-CoV-2 RNA across more than 2 intervals (RTPCR-Negative Group) and 38 patients still tested positive for SARS-CoV-2 RNA (RTPCR-Positive Group). Abbreviations: APACHE II-Acute Physiology and Chronic Health Evaluation II; ICU-intensive care unit; ECMO-extracorporeal membrane oxygenation. Available via Oxford University Press Public Health Emergency Collection through PubMed Central.
PEER-REVIEWED
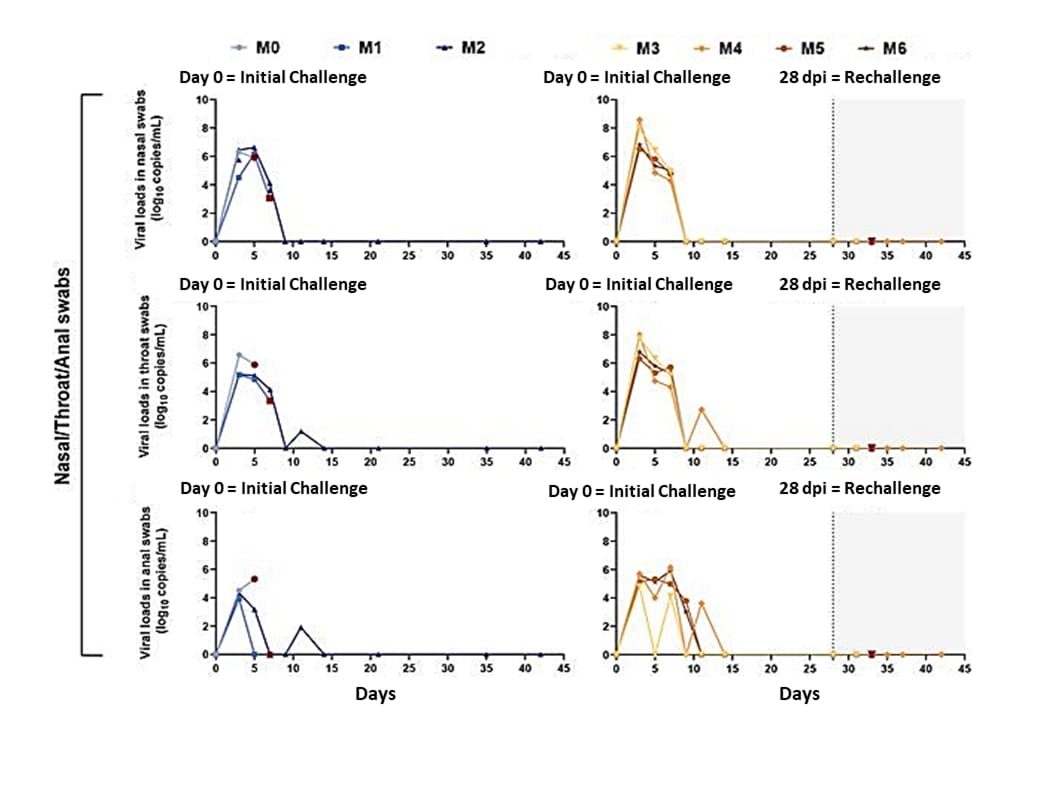
Primary exposure to SARS-CoV-2 protects against reinfection in rhesus macaquesexternal icon. Deng et al. Science (July 2, 2020).
Key findings:
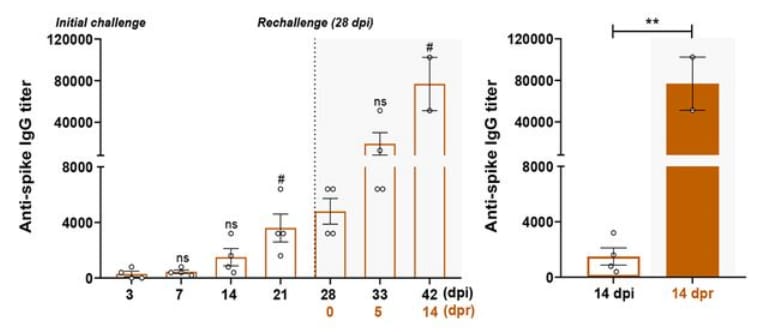
- Comparisons of humoral and cellular immunity between primary infection and re-challenge revealed enhanced neutralizing antibody and immune responses.
- Viral RNA in nasal, throat, and anal swabs of re-challenged monkeys were significantly lower than those of the initial infection (Figure 1).
- Titers of neutralizing antibodies exhibited enhancement at the time of re-challenge (Figure 2).
Methods: Seven adult rhesus macaques (M0 to M6,) examined in challenge–re-challenge study with tracking of clinical signs and viral replication to compare SARS-CoV-2 virus distribution and histopathological changes between initially infected and re-infected monkeys. Limitations: Animal study.
Figure 1
Note: Adapted from Deng et al. Viral RNA in nasal, throat, and anal swabs. Two rhesus macaques (M1, M2) were challenged at day 0 only (left-hand panels). Four (M3, M4, M5, M6) were challenged at day 0 and again with the identical strain at day 28 (right-hand panels). One macaque (M0) received initial challenge at day 28 as a control for time. dpi = days past initial challenge. From Deng et al. Science. DOI: 10.1126/science.abc5343. Reprinted with permission from AAAS.
Figure 2
Note: Adapted from Deng et al. Levels of specific IgG against the spike protein of SARS-CoV-2 increased over time in the four re-challenged monkeys (left-hand panel). Significantly increased levels of IgG were observed between the initial challenges and re-challenges as shown in the comparison between 14 days post initial challenge (dpi) and 14 days post re-challenge (dpr); **p <0.01); whisker bars were not defined. From Deng et al. Science. DOI: 10.1126/science.abc5343. Reprinted with permission from AAAS.
- Paterson et al. The emerging spectrum of COVID-19 neurology: clinical, radiological and laboratory findingsexternal icon. Brain. Describes five categories of neurological disorder among 29 of 43 patients diagnosed with COVID-19.
- Weizman et al. Use of wearable technology to enhance response to the COVID-19 pandemicexternal icon. Public Health. A biometric bracelet with a unique identifier and an infrared thermometer, GPS, and capacity to transfer data over a network would enable COVID-19 tracking in real-time.
- O’Callaghan et al. Developing a SARS-CoV-2 vaccine at warp speedexternal icon. JAMA. Discusses the proposed high-priority vaccine candidates designed to induce antibodies directed against the receptor-binding domain mechanisms and current status of five of the surface spike protein of SARS-CoV-2.
- Sette et al. Pre-existing immunity to SARS-CoV-2: the knowns and unknownsexternal icon. Nature Reviews Immunology. Pre-existing T cell immunity might be related to prior common cold coronavirus exposure for some people.
- Petersen et al. Comparing SARS-CoV-2 with SARS-CoV and influenza pandemicsexternal icon. Lancet Infectious Diseases. A review of SARS-Cov-2 spread using previous pandemics for context points out the importance of early action and longstanding infectious disease containment measures for epidemic control.
- Stanworth et al. Effects of the COVID-19 pandemic upon supply and use of blood for transfusionexternal icon. Lancet Haematology. Recommends policies to help plan for imbalances in blood supply in the COVID-19 pandemic.
- Sigel et al. Covid-19 and people with HIV infection: outcomes for hospitalized patients in New York Cityexternal icon. Clinical Infectious Diseases. Adverse outcomes associated with HIV infection for hospitalized COVID-19 patients were no different compared to demographically similar patients not infected with HIV.
- Han et al. Feasibility study of mixing throat swab samples for severe acute respiratory syndrome coronavirus-2 screeningexternal icon. Virologica Sinica. qRT-PCR testing results were still reliable when samples were diluted to six-fold, suggesting that mixing multiple throat swab samples might lower testing costs without compromising reliability of COVID-19 nucleic acid screening.
In the July 10, 2020 Science Update, the entry for Magleby et al.external icon, the labels on the figure for adjusted odds ratios for in-hospital mortality and intubation and mechanical ventilation were inadvertently switched with one another. The rates in the text are correct as written. The error has been corrected in the online version of the update.
Disclaimer: The purpose of the CDC COVID-19 Science Update is to share public health articles with public health agencies and departments for informational and educational purposes. Materials listed in this Science Update are selected to provide awareness of relevant public health literature. A material’s inclusion and the material itself provided here in full or in part, does not necessarily represent the views of the U.S. Department of Health and Human Services or the CDC, nor does it necessarily imply endorsement of methods or findings. While much of the COVID-19 literature is open access or otherwise freely available, it is the responsibility of the third-party user to determine whether any intellectual property rights govern the use of materials in this Science Update prior to use or distribution. Findings are based on research available at the time of this publication and may be subject to change.