COVID-19 Science Update released: April 30, 2021 Edition 87

The COVID-19 Science Update summarizes new and emerging scientific data for public health professionals to meet the challenges of this fast-moving pandemic. Weekly, staff from the CDC COVID-19 Response and the CDC Library systematically review literature in the WHO COVID-19 databaseexternal icon, and select publications and preprints for public health priority topics in the CDC Science Agenda for COVID-19 and CDC COVID-19 Response Health Equity Strategy.
Section headings in the COVID-19 Science Update align with the CDC Science Agenda for COVID-19.
Section headings in the COVID-19 Science Update have been changed to align
with the CDC Science Agenda for COVID-19.
Here you can find all previous COVID-19 Science Updates.
PEER-REVIEWED
Prevalence and clinical profile of severe acute respiratory syndrome coronavirus 2 infection among farmworkers, California, USA, June–November 2020. Lewnard et al. Emerging Infectious Diseases (March 3, 2021).
Key findings:
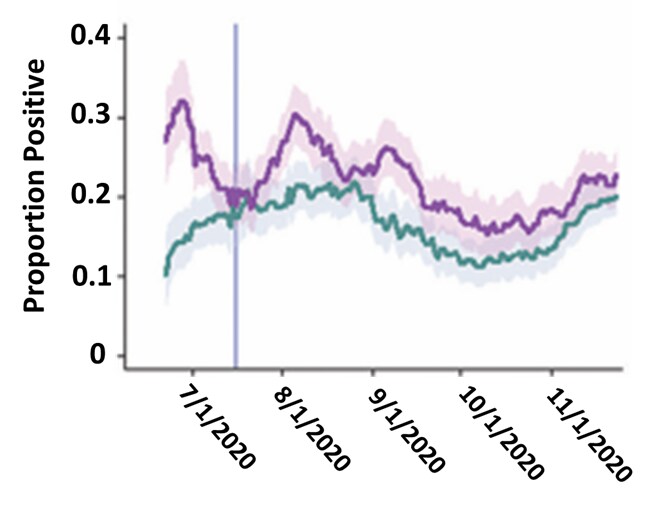
- Clinical surveillance found 28.5% (95% CI 20.1-37.4%) higher probability of SARS-CoV-2 infection among farmworkers (22.1%) compared with other adults from the same communities (17.2%), between June 15 and November 30, 2020 (Figure).
- Among farmworkers in a cross-sectional study, prevalence of current infection was 27.7% in those reporting >= 1 COVID-19 symptom in the prior 2 weeks compared with 7.2% in those without symptoms (adjusted OR 4.16; 95% CI 2.85-6.06).
Methods: Clinical surveillance of SARS-CoV-2 infection based on oropharyngeal swabs at a community and migrant health center in Monterey County, California (6,864 farmworkers and 7,305 other adults in the same communities). A cross-sectional study of farmworkers (n = 1,115) recruited at clinic visit and through outreach assessed for SARS-CoV-2 infection and SARS-CoV-2 symptoms. Limitations: Results not generalizable to all farmworkers.
Implications: SARS-CoV-2 vaccination and prevention efforts should prioritize farmworkers, who may be disproportionately impacted.
Figure:
Note: Adapted from Lewnard et al. Proportion of positive SARS-CoV-2 positive cases among farmworkers and other adults in the same communities. Shading: 95% CIs. Vertical line: start of cross-sectional study. Licensed under CC-BY-NC-ND.
Symptoms of anxiety, burnout, and PTSD and the mitigation effect of serologic testing in emergency department personnel during the COVID-19 pandemic.external icon Rodriguez et al. Annals of Emergency Medicine (February 4, 2021).
Key findings:
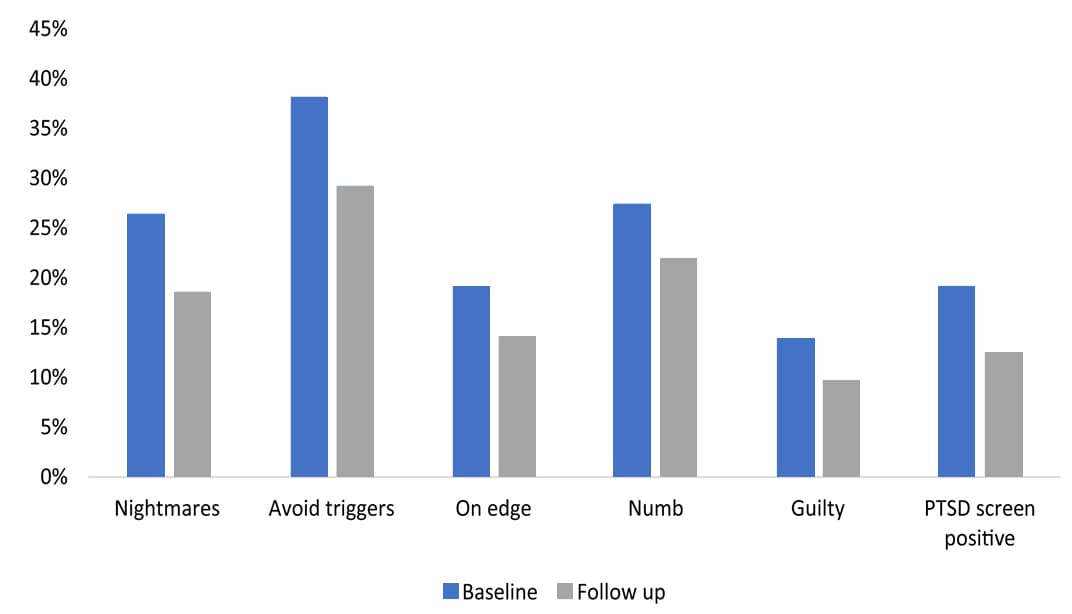
- 46% of emergency department (ED) personnel (N = 1,606) reported symptoms of emotional exhaustion and burnout.
- 308 (19.2%; 95% CI, 17.3%-21.1%) screened positive at baseline for increased risk of post-traumatic stress disorder (PTSD) by self-reporting symptoms such as having nightmares, avoiding triggers, and feeling on edge (Figure).
- Female respondents were more likely than males to report symptoms consistent with PTSD (odds ratio [OR] 2.03, 95% CI 1.49-2.78).
- Among respondents to both baseline and follow-up surveys, fewer personnel screened positive for PTSD risk following SARS-CoV-2 serological testing (reduction 6.5%; 95% CI 4.6%-8.5%).
- A positive serology test was associated with decreased anxiety (OR 2.83, 95% CI 1.28-6.25).
Methods: Prospective cohort study across 20 EDs in 15 states. Standardized questionnaires were administered, including a screening instrument for PTSD based on the Diagnostic and Statistical Manual of Mental Disorders 5th Edition (DSM-5), at baseline with follow-up ~3 weeks after testing for antibodies to SARS-CoV-2. Limitations: Short follow-up period; lack of control group.
Implications: PTSD symptoms were prevalent among ED staff and were compounded by the uncertainty of their SARS-CoV-2 status. Mitigation strategies and increased SARS-CoV-2 testing may reduce PTSD risk.
Figure:
Note: Adapted from Rodriguez et al. ED personnel responses to the DSM-5 PTSD screening instrument. May to July 2020: the proportion reporting “yes” to experiencing each symptom in the week prior to the baseline and follow-up surveys administered after serological testing for SARS-CoV-2 antibodies. Permission request in process.
Prevalence of SARS-CoV-2 antibodies among market and city bus depot workers in Lima, Peruexternal icon. Tovar et al. Clinical Infectious Diseases (April 21, 2021). Published in Annals of Epidemiologyexternal icon (November 2021).
Key findings:
- SARS-CoV-2 antibody positivity ranged from 27% to 73% in market workers at 8 different markets.
- SARS-CoV-2 antibody positivity was 11%, 32% and 47% among workers at 3 bus depots.
- Antibody positivity among bus drivers was 8%, 27%, and 42% at the corresponding depots.
Methods: Day-long SARS-CoV-2 antibody testing campaigns were conducted at 8 markets and 3 bus depots between June 5 and July 18, 2020. Participating market workers (n = 1,285) and bus depot workers (n = 488) received rapid SARS-CoV-2 antibody testing using the Standard Q COVID-19 IgG/IgM Duo. Prevalence of antibody positivity (combined IgG/IgM) was reported. Limitation: Sampling from the workplace can introduce healthy worker bias potentially underestimating past (or current) SARS-CoV-2 infection.
Implications: High prevalence of SARS-CoV-2 infection among market and bus depot workers suggests a critical need for prioritizing frontline workers for vaccination.
PREPRINTS (NOT PEER-REVIEWED)
A disproportionate epidemic: COVID-19 cases and deaths among essential workers in Toronto, Canada.external icon Rao et al. medRxiv (March 11, 2021).
Key finding:
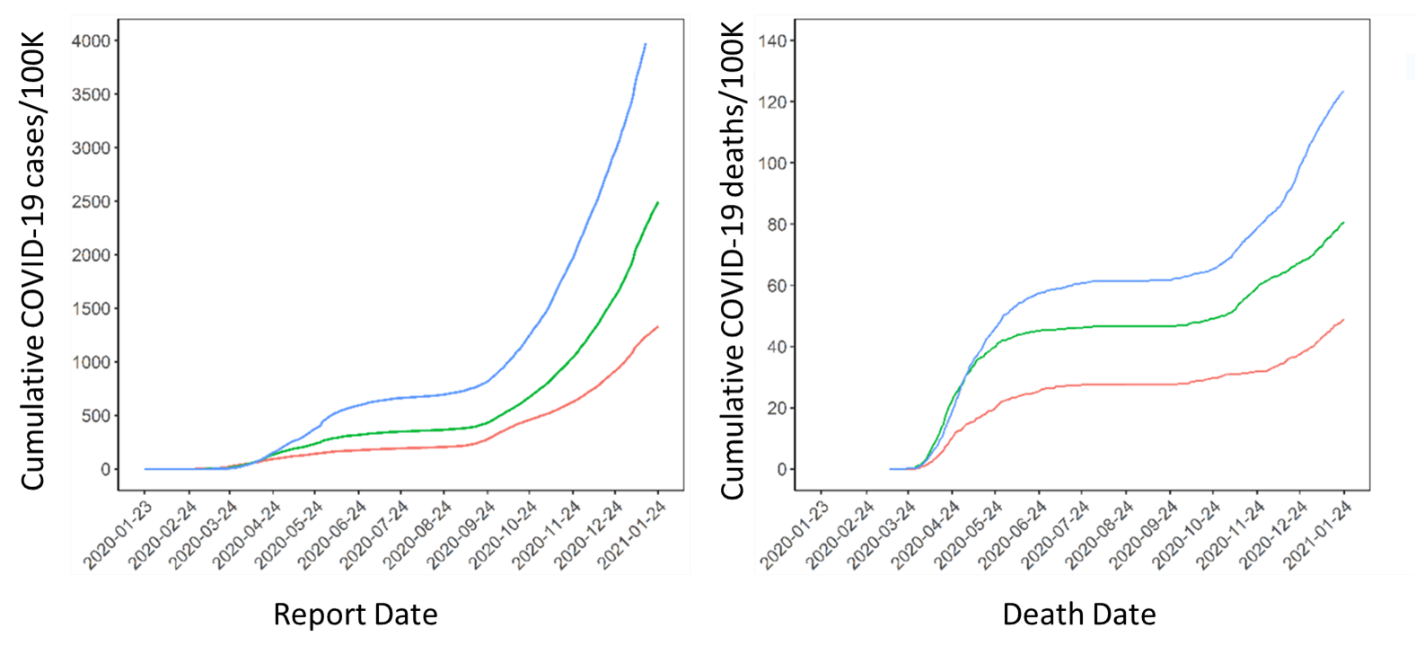
- Cumulative per capita cases and deaths were 3.3-fold and 2.5-fold higher, respectively, in neighborhoods with the highest proportion of essential workers compared with neighborhoods with the lowest concentration of essential workers (Figure).
Methods: COVID-19 cases (n = 74,477) and deaths (n = 2,319) between January 23, 2020 and January 24, 2021, in different Toronto neighborhoods compared by proportion of population (in tertiles) that were essential workers (including those in health, food, agriculture, transportation and manufacturing) based on census data. Limitations: Lack of generalizability of results.
Implications: Vaccination is needed to reduce COVID-19 case and death burden among essential workers; community-based interventions targeting neighborhoods with high proportions of essential workers may help reach this population.
Figure:
Note: Adapted from Rao et al. Cumulative per-capita COVID-19 cases and deaths by neighborhood-level proportion of essential workers. Essential worker proportions in neighborhoods were stratified by tertiles: Stratum 1 (27.8%; 95% CI 23.4-31.5), Stratum 2 (44.7%; 95% CI 40.0-50.0), Stratum 3 (62.9%; 95% CI 58.4%-68.0). Deaths are 7-day rolling averages. Data do not include residents of long-term care homes. Licensed under CC-BY-NC-ND 4.0.
Excess mortality associated with the COVID-19 pandemic among Californians 18-65 years of age, by occupational sector and occupation, March through October 2020external icon. Chen et al. medRxiv (January 22, 2021). Published in PLOS ONEexternal icon (June 4, 2021).
Key findings:
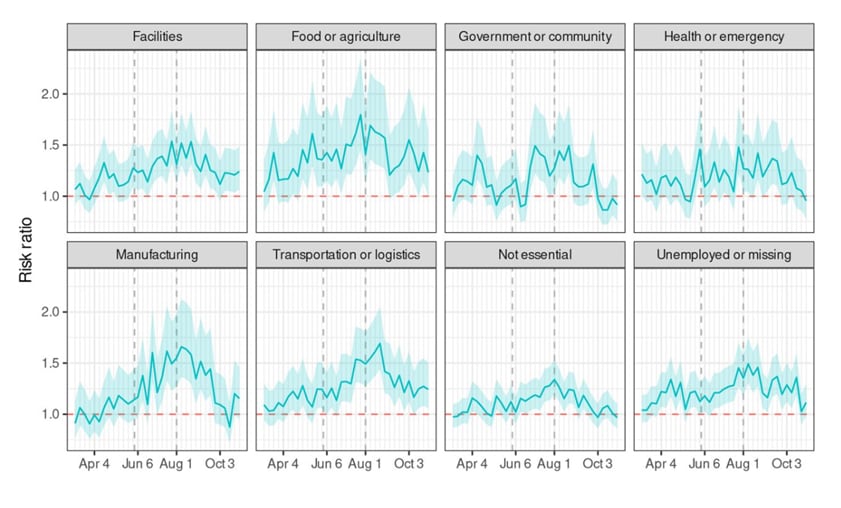
- Compared with prior to the pandemic, working-age Californians experienced 22% increased risk of mortality between March and October 2020.
- Increased mortality was seen among Asian adults (risk ratio [RR] 1.18, 95% CI 1.14-1.23), Black adults (RR 1.28, 95% CI 1.24-1.33), Latino adults (RR 1.36, 95% CI 1.29-1.44) and White adults (RR 1.06 95% CI 1.02-1.12).
- Increased mortality was seen across all sectors (RR 1.22, 95% CI 1.20-1.24) and was highest for essential workers in food/agriculture (RR 1.39, 95% CI 1.29-1.44) and transportation/logistics (RR 1.28, 95% CI 1.24-1.33) (Figure).
Methods: Death certificates were obtained from the California Department of Health for all deaths occurring on or after January 1, 2016. For decedents aged 18 to 65, occupations were categorized into 9 groups: facilities, food/agriculture, government/community, health/emergency, manufacturing, retail, transportation/logistics, not essential, and unemployed/missing. Excess deaths from March to October 2020 were recorded overall and for each sector. Limitations: Primary occupation on the death certificate may not match the individual’s most recent occupation; misclassification of occupation on death certificates due to broad categories or inaccurate reports.
Implications: In-person essential work may facilitate SARS-CoV-2 transmission and should be addressed through strict enforcement of health orders in workplace settings, protection of in-person workers, and prioritization of vaccine distribution.
Figure:
Note: Adapted from Chen et al. Risk ratios for death among Californians 18-65 years of age, by occupational sector, March through October 2020. The dashed vertical lines mark boundaries between phases of California’s major pandemic policies, lagged to acknowledge time from policy decisions to infection and death. The first phase corresponds to a period of sheltering in place, while the second phase corresponds to a period of reopening. Dashed horizontal line denotes RR 1. Used by permission of authors.
PEER-REVIEWED
COVID-19 mitigation with appropriate safety measures in an essential workplace: Lessons for opening work settings in the United States during COVID-19.external icon Haigh et al. Open Forum Infectious Diseases (February 22, 2021).
Key findings:
- Among workers at 3 manufacturing facility sites that implemented non-pharmaceutical interventions (NPIs) early in the pandemic, a single-day testing campaign found 7.5% of on-site employees tested positive for SARS-CoV-2 and 10.4% had inconclusive results.
- Rates of infection were highest at the site with the highest community case prevalence and lowest at the site with the lowest community case prevalence.
- Among employees with positive or inconclusive tests, 99% were asymptomatic when tested.
Methods: Single day PCR testing of 586 on-site employees at 3 manufacturing plants in Arizona, California, and New Hampshire between July and August 2020. NPIs began in January 2020 and included travel restrictions, handwashing, masking, HEPA filtration, on-site screening, expanded sick leave, requested self-isolation for symptoms, paid quarantine for COVID-19 illness and exposure, workbench shields, one-way walking paths, employee spacing, and availability of face shields and KN95 masks. Limitations: Compliance with NPIs not assessed; findings may not be generalizable.
Implications: In manufacturing settings with robust NPI, transmission was limited; however, screening testing suggests that asymptomatic cases may be missed.
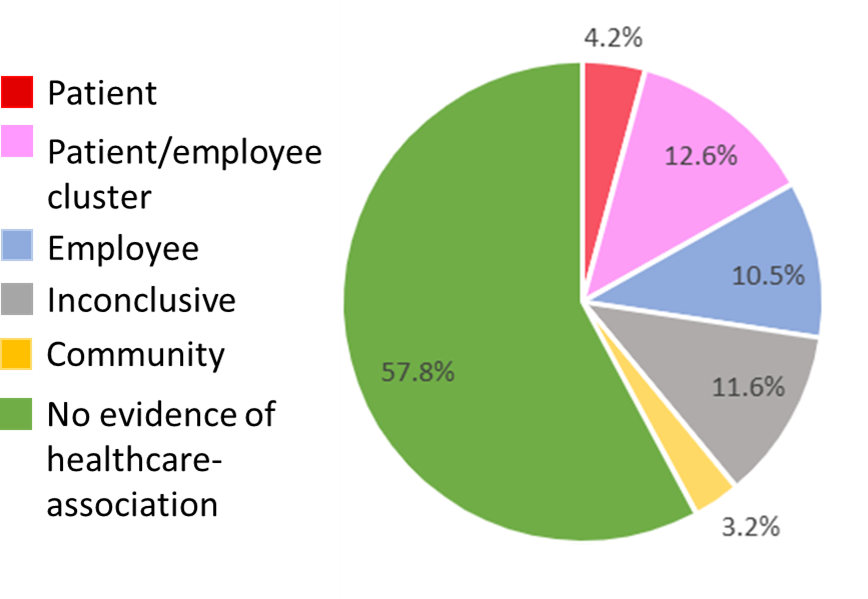
Viral sequencing reveals US healthcare personnel rarely become infected with SARS-CoV-2 through patient contactexternal icon. Braun et al. Clinical Infectious Diseases (April 15, 2021).
Key findings:
- Only 27.3% of healthcare personnel (HCP) SARS-CoV-2 infections were linked to patients, coworkers, or both.
- Only 4.2% could be linked definitively to a patient source (Figure).
- 61% were not healthcare-associated, including 3 where community transmission could be established (Figure).
Methods: Case series of 95 HCP with SARS-CoV-2 infections at a Wisconsin medical center between March and December 2020. Using exposure history and viral genome testing, infection source was inferred if known exposure or genomes matched closely. Limitations: Fewer than 10% of infected all employed HCP were studied; genomic testing performed only when no known exposure; biosamples unavailable for some patients.
Implications: The majority of HCP infections could not be linked to a patient or co-worker, suggesting HCP are more likely to be infected in the community than at work.
Figure:
Note: Adapted from Braun et al. Table 1. Likely source of infection among healthcare personnel. Permission request in progress.
PREPRINTS (NOT PEER-REVIEWED)
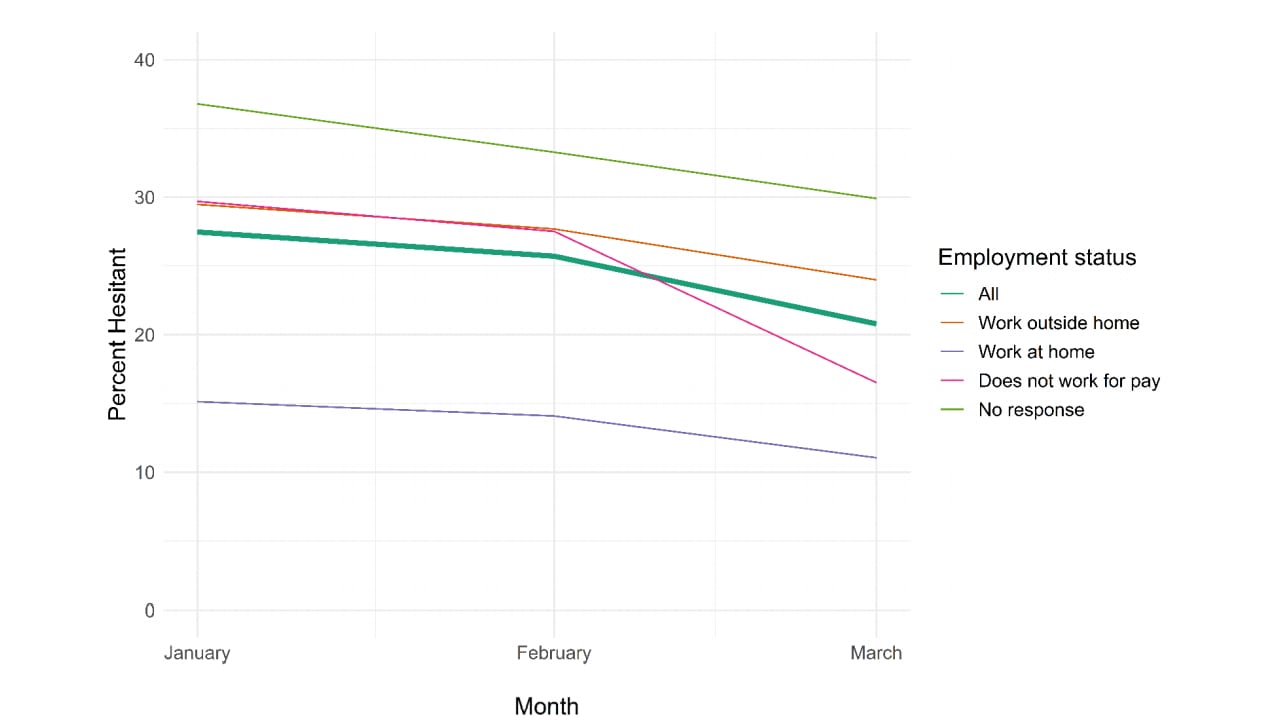
COVID-19 vaccine hesitancy January − March 2021 among 18 − 64-year-old U.S. adults by employment and occupationexternal icon. King et al. medRxiv (April 24, 2021). Published in Preventive Medicine Reports as COVID-19 vaccine hesitancy January-May 2021 among 18–64 year old US adults by employment and occupationexternal icon (December 2021).
Key findings:
- Among adults 18-64 years, vaccine hesitancy decreased from 27.5% (95% CI 27.3-27.6) in January 2021 to 22.1% (95% CI 21.9-22.2) in March 2021 (Figure).
- Vaccine hesitancy varied by occupational category, from 9.6% (95% CI 8.5-10.7) in the life/physical/social sciences to 46.4% (95% CI 45.1-47.7) in construction.
- Hesitancy was related to concern about side effects, not believing the need for a vaccine, lack of trust in the government or vaccines, or wanting to wait to see if the vaccine was safe.
Methods: A COVID-19 vaccine acceptance survey was administered to a random sample of Facebook users 18–64 years old stratified by region, January−March 2021. Percentages and risk ratios were estimated using a weighted Poisson regression. Limitations: White race and higher education were over-represented in the internet-based sample.
Implications: Though vaccine hesitancy is decreasing overall, there is still high hesitancy, especially in some occupational categories; addressing concerns about vaccine safety and trust will be critical for increasing vaccination rates.
Figure:
Note: Vaccine hesitancy overall and by employment status, in all 18-64 year olds and in those reporting they work outside home, work at home, do not work for pay, or did not respond with employment status in January (n = 791,716), February (n = 710,529) and March (732,308) 2021. Used by permission of authors.
PREPRINTS (NOT PEER-REVIEWED)
Psychological impact of the lockdown due to the COVID-19 pandemic in university workers: factors related to stress, anxiety, and depressionexternal icon. Salazar et al. International Journal of Environmental Research and Public Health (April 20, 2021).
Key findings:
- Early in the pandemic scores for depression in university workers:
- Were higher among women than men.
- Decreased as education level increased.
- Were higher among participants with a personal history of chronic illness than among those without a history of chronic illness.
- Decreased with age.
Methods: Cross-sectional online study of 677 Spanish university workers between April 8 and April 22, 2020 collected sociodemographic and occupational data in addition to housing, work, and health conditions. Levels of anxiety, stress, and depression were measured using various validated scales. Limitations: workers with worse physical or mental health may not have participated; findings may not be generalizable; participants were not asked about their previous history of anxiety, depression, or stress.
Implications: University workers with specific sociodemographic and occupational characteristics, as well as clinical disorders, may have been more at risk for depression, anxiety, and stress during the COVID-19 lockdown. Thus, it may be necessary to assess and monitor the mental health of these workers during and after a pandemic lockdown.
Detection, Burden, and Impact
- Kamalakannan et al. Health risks and consequences of a COVID-19 infection for people with disabilities: scoping review and descriptive thematic analysis.external icon International Journal of Environmental Research and Public Health (April 20, 2021). Scopus review of 58 articles describing increased risk of SARS-CoV-2 infection and health consequences among people with disabilities.
- Rossman et al. COVID-19 dynamics after a national immunization program in Israel.external icon Nature Medicine (April 19, 2021). In Israel, COVID-19 cases and hospitalizations decreased first in individuals ≥60 years old, followed by younger age groups, reflecting vaccination prioritization.
Natural History of SARS-CoV-2 Infection
- Tomkins-Tinch et al. SARS-CoV-2 reinfection in a liver transplant recipientexternal icon. Annals of Internal Medicine (April 20, 2021). A liver transplant recipient had 2 distinct SARS-CoV-2 infections separated by 111 days based on clinical findings and genomic sequencing . No antibody response was detected after the 1st infection.
- Hacisuleyman et al. Vaccine breakthrough infections with SARS-CoV-2 variants.external icon NEJM (April 21, 2021). More than 2 weeks following 2-dose COVID-19 mRNA vaccination, 2 women were found to have symptomatic SARS-CoV-2 infection with mutations including E484K in 1 patient and S477N in the 2nd patient, underscoring the continued need to prevent and diagnose SARS-CoV-2 even in vaccinated persons.
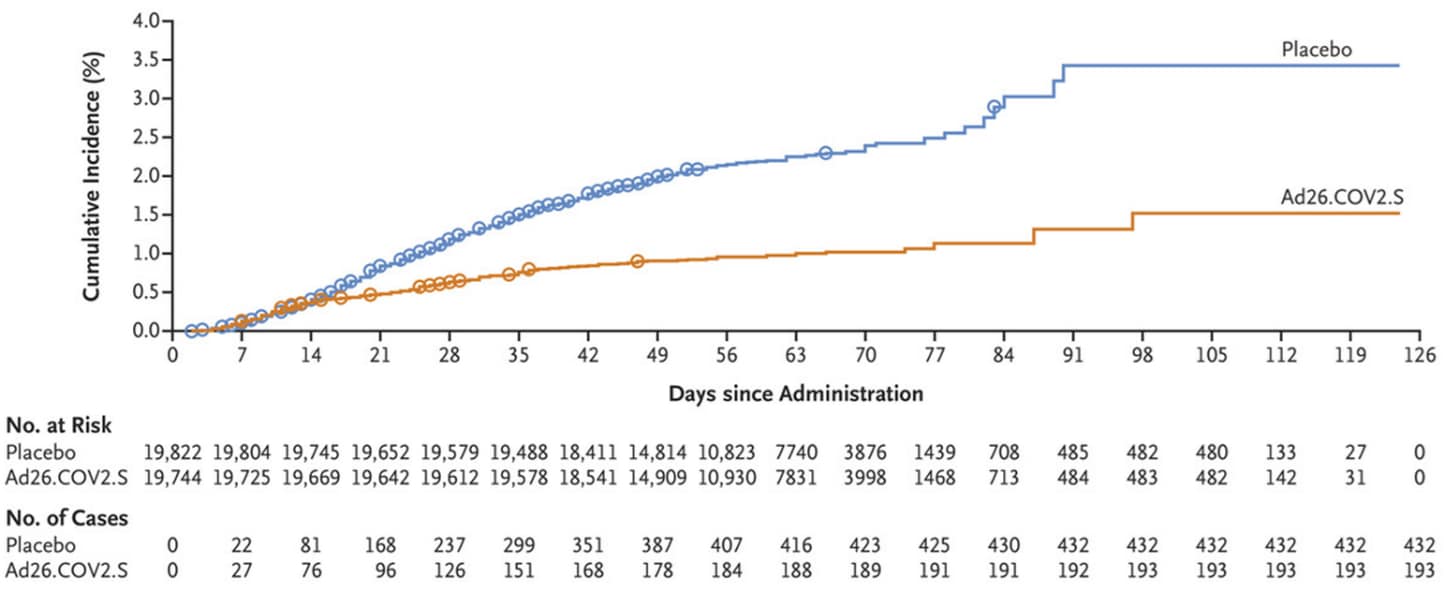
Prevention, Mitigation, and Intervention Strategies
- Sadoff et al. Safety and efficacy of single-dose Ad26.COV2.S vaccine against COVID-19.external icon NEJM (April 21, 2021). A phase 3 RCT (n = 39,321) found single-dose Ad26.COV2.S prevented moderate to severe–critical Covid-19 ≥14 days after vaccination (efficacy 66.9%; adjusted 95% CI 59.0-73.4). Thromboembolic events were more common in the vaccine group (11) than the placebo group (3); 1 vaccine recipient had transverse sinus thrombosis with cerebral hemorrhage.
Figure:
Note: Adapted from Sadoff et al. Cumulative incidence of moderate to severe–critical COVID-19 cases in participants who received placebo and Ad26.COV2.S. Circles indicate severe–critical cases. From the New England Journal of Medicine, Sadoff et al., Safety and efficacy of single-dose Ad26.COV2.S vaccine against COVID-19. April 21, 2021, online ahead of print. Copyright © 2021 Massachusetts Medical Society. Reprinted with permission from Massachusetts Medical Society.
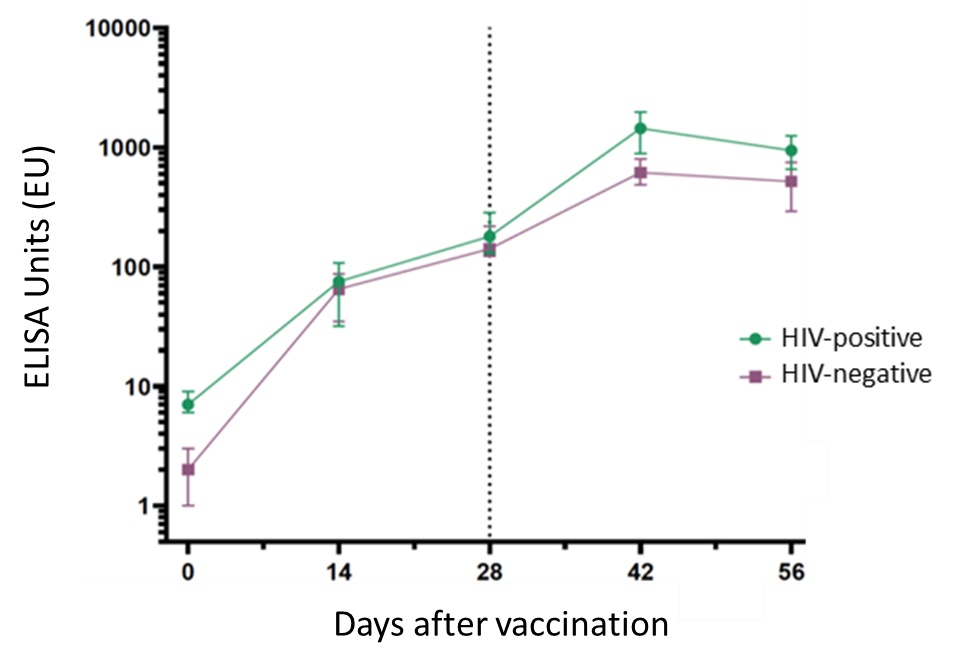
- Frater et al. Safety and immunogenicity of the ChAdox1 nCoV-19 (AZD1222) vaccine against SARS-CoV-2 in HIV infectionexternal icon. SSRN (Preprint, April 19, 2021). Published in The Lancet HIV as Safety and immunogenicity of the ChAdOx1 nCoV-19 (AZD1222) vaccine against SARS-CoV-2 in HIV infection: a single-arm substudy of a phase 2/3 clinical trialexternal icon (June 18, 2021). Following 2 doses of ChAdOx1 nCoV-29 vaccine administered 4-6 weeks apart, antibody and T cell responses in 54 HIV-positive men were comparable with 50 HIV-negative participants; no severe adverse effects were observed.
Figure:
Note: Adapted from Frater et al. SARS-CoV-2 IgG responses to spike protein at days 0, 14, 28, 42 and 56 after vaccination with ChAdOx1 in people with and without HIV. The threshold for a positive response is 10 ELISA Units (EU). Data points are medians; error bars represent 95% CI); vertical line at Day 28 marks timing of the second dose. Permission request in process.
- Herishanu, et al. Efficacy of the BNT162b2 mRNA COVID-19 vaccine in patients with chronic lymphocytic leukemia.external icon Blood (April 16, 2021). Only 27 of 52 patients with chronic lymphocytic leukemia (CLL) developed an antibody response following 2 doses of BNT162b2 vaccine, compared with all 52 sex-and age-matched healthy controls. 79.2% of patients in remission for CLL developed antibodies following vaccination compared with 16% of patients in treatment for CLL.
Disclaimer: The purpose of the CDC COVID-19 Science Update is to share public health articles with public health agencies and departments for informational and educational purposes. Materials listed in this Science Update are selected to provide awareness of relevant public health literature. A material’s inclusion and the material itself provided here in full or in part, does not necessarily represent the views of the U.S. Department of Health and Human Services or the CDC, nor does it necessarily imply endorsement of methods or findings. While much of the COVID-19 literature is open access or otherwise freely available, it is the responsibility of the third-party user to determine whether any intellectual property rights govern the use of materials in this Science Update prior to use or distribution. Findings are based on research available at the time of this publication and may be subject to change.