COVID-19 Science Update released: April 1, 2020 Edition 1

The COVID-19 Science Update summarizes new and emerging scientific data for public health professionals to meet the challenges of this fast-moving pandemic. Weekly, staff from the CDC COVID-19 Response and the CDC Library systematically review literature in the WHO COVID-19 databaseexternal icon, and select publications and preprints for public health priority topics in the CDC Science Agenda for COVID-19 and CDC COVID-19 Response Health Equity Strategy.
Here you can find all previous COVID-19 Science Updates.
PEER-REVIEWED
Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italyexternal icon. Onder et al. JAMA (March 23, 2020; Correction external iconon April 10, 2020).
Key findings:
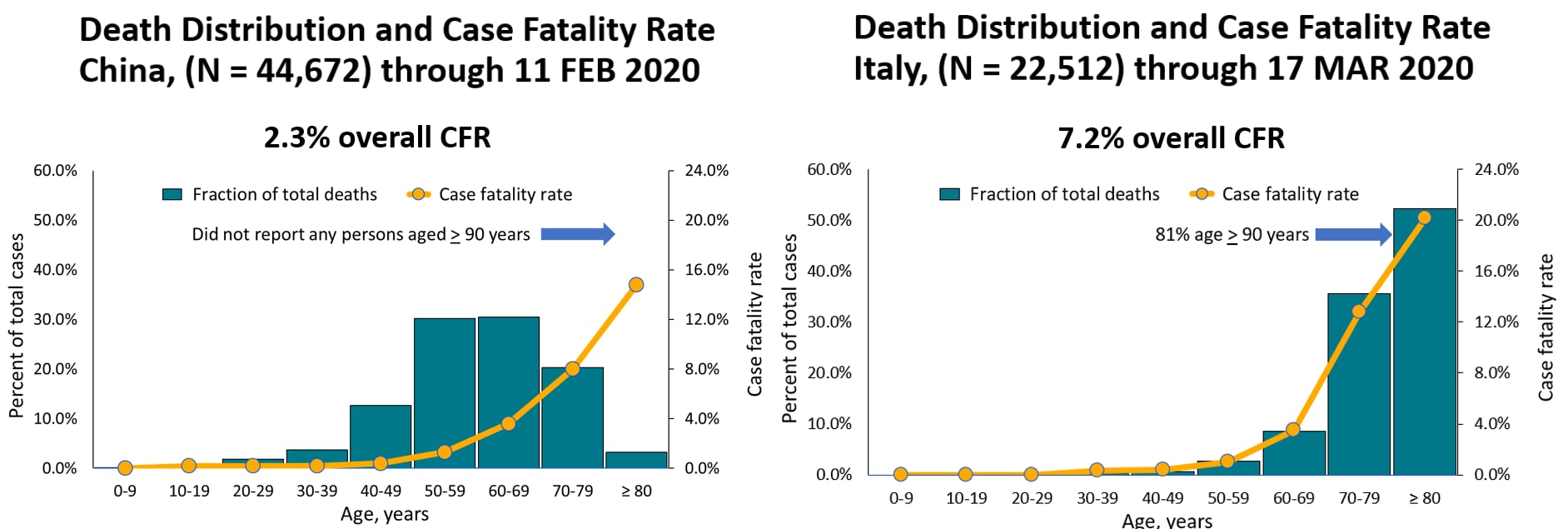
- COVID-19 crude case fatality rates (CFR) were higher in Italy (7.2%) than China (2.3%) (Figure 1).
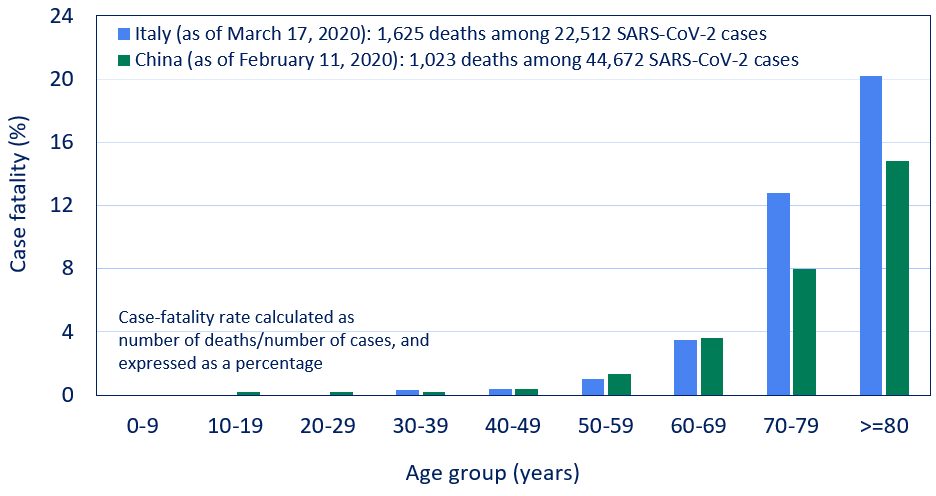
- Age-stratified CFRs remained higher in Italy among persons aged ≥70 years (Figure 2).
- The fraction of deaths among persons aged ≥70 years was greater in Italy (38%) than China (12%).
- CFR differences by country:
- Population age structure.
- Burden of comorbidities.
- Definition of COVID-19 deaths (i.e., attribution of death to COVID-19).
- Testing strategies (e.g., In Italy, testing focused on severely symptomatic patients).
Methods: Comparison of crude and age-stratified CFRs among COVID-19 cases in Italy (n = 1,625 deaths through March 17, 2020) and China (n = 1,023 deaths through February 11, 2020). Limitations: China did not report data for persons ≥90 years.
Implications: Population age structure and comorbidities need to be considered when assessing CFRs. Standardized testing and case reporting practices can help increase the utility of CFR comparisons between countries.
Figure 1
Note: Adapted from Zhang et al. (Vital Surveillances: The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) — China, 2020external icon; China CDC Weekly Reports) and from Onder et al. Reproduced with permission from JAMA doi:10.1001/jama.2020.4683. Copyright©2020 American Medical Association. All rights reserved.
Figure 2
Note: Adapted from Onder et al. Case fatality rate by age group in Italy and China. Reproduced with permission from JAMA doi:10.1001/jama.2020.4683. Copyright©2020 American Medical Association. All rights reserved.
Knowledge and perceptions of COVID-19 among the general public in the United States and United Kingdom: A cross-sectional online surveyexternal icon. Geldsetzer, P. Annals of Internal Medicine (March 20, 2020).
Key findings:
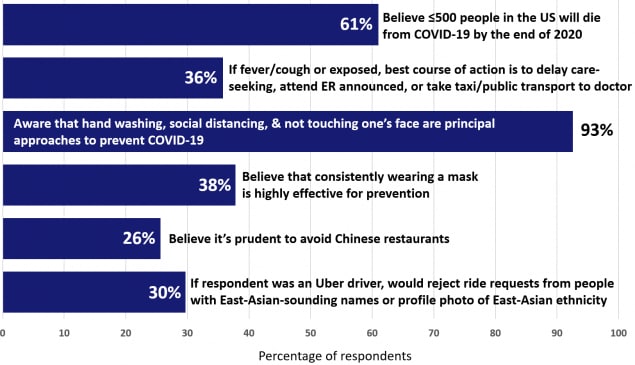
- Underestimation of the death toll: 61% of US respondents thought estimated deaths at ≤ 500 in 2020.
- Correct identification of prevention approaches: 93% identified washing hands, social distancing, avoiding touching one’s face (Figure).
- Some prejudicial beliefs identified: about 30% would avoid Chinese restaurants, or reject Uber customers with East-Asian names or profile pictures
Methods: Cross-sectional online survey among 2,986 US and 2,988 UK adults, February 23 to March 2, 2020.
Implications: US adults have strong understanding of prevention measures, but poor understanding of the likely death toll, which may limit cooperation with restrictions. Efforts to combat biases may be warranted.
Figure:
Note: Adapted from Geldsetzer, P. Available via American College of Physicians Public Health Emergency Collection through PubMed Central.
PEER-REVIEWED
Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2)external icon. Li et al. Science (March 16, 2020).
Key Findings:
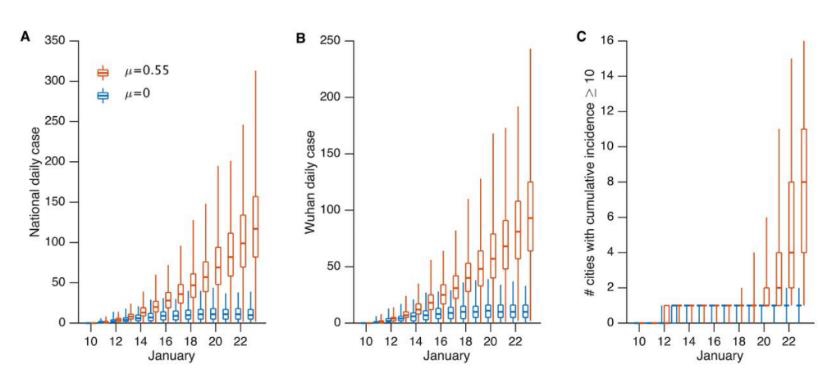
- Before emplacement of travel restrictions in China on January 23, 2020, model suggests 86% of COVID-19 infections were among “undocumented” (i.e., undiagnosed) persons who were infectious but had very mild or asymptomatic illness and this went unrecognized.
- Modeling suggests asymptomatically infected persons were half as contagious as persons with clinical (documented) illness but were the source of 79% of documented cases.
- During travel restrictions, the fraction of undocumented infections declined to 35%.
Methods: Modeled prevalence and contagiousness of undocumented COVID-19 across China. Sensitivity analyses conducted.
Implications: Contagious infections among persons with no or little evident illness facilitated spread of COVID-19 within China, which reinforces the value of testing and social distancing as prevention measures.
Figure:
Note: From Li et al. Simulated outbreak spread under two scenarios with differing transmission rates (µ) showing estimated case counts and credible 95% CIs: RED evolution of cases in a hypothetical outbreak using estimated per-individual infectiousness for “undocumented” persons with µ = 0.55, and BLUE the same hypothetical outbreak but undocumented infections are not contagious with µ = 0. (A) Daily documented cases in all cities. (B) Daily documented cases in Wuhan city. (C) Number of cities with ≥10 cumulative documented cases. Licensed under CC-BY 4.0.
PEER-REVIEWED
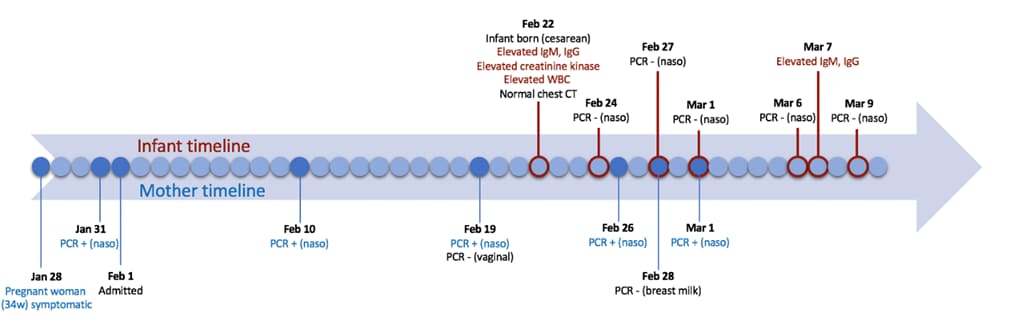
Possible vertical transmission of SARS-CoV-2 from an infected mother to her newborn.external iconDong et al. JAMA (March 26, 2020).
Key Findings:
- An infant born by caesarian section to a mother with COVID-19 exhibited elevated anti-SARS-CoV-2 IgM antibodies (IgM is not transferrable to fetus via placenta) two hours post-delivery (Figure).
- Mother’s vaginal secretions at delivery and breast milk were negative by for SARS-CoV-2 RNA.
- Infant had serial negative tests for SARS-CoV-2 RNA by NP swabs and a normal chest CT.
Methods: Case report from Renmin Hospital, in Wuhan China. Mother and infant underwent chest CT. NP swabs tested by RT-PCR. Limitations: IgM assays can be falsely positive in infants (IgM values declined in this report seems more rapidly than expected, see commentaryexternal icon).
Implications: Consistent with existing published dataexternal icon, there continues to be no evidence of perinatal SARS-CoV-2 transmission.
Figure:
Note: Adapted from Dong et al. Shows a timeline of clinical findings for the mother (bottom, blue) and infant (top, red). Text “naso” refers to nasopharyngeal. Reproduced with permission from JAMA doi:10.1001/jama.2020.4621. Copyright©2020 American Medical Association. All rights reserved.
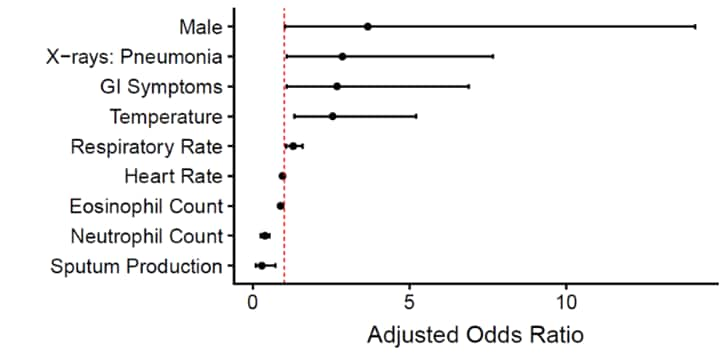
Epidemiological and clinical predictors of COVID-19external icon. Sun et al. Clinical Infectious Diseases (March 25, 2020).
Key Findings:
- Several clinical factors derived from readily available clinical data were associated with lab-confirmed COVID-19 among patients presenting for care (Figure).
- Predictive models performed well (AUC ≥0.88) with parsimonious sets of these clinical covariates.
Methods: Multivariable logistic regressions predicted individual risk of SARS-CoV-2 infection in Singapore during January 26 to February 16, 2020 (n = 788, with n = 54 lab-confirmed COVID-19 cases). Limitations: Definitions lacking for “significant” heart rate and respiratory rate; lab values and ranges not described.
Implications: Readily available clinical data may help identify persons with COVID-19 when they present to care and before testing. Further refinement of this approach may improve rapid and accurate triage.
Figure:
Note: Adapted from Sun et al. Figure shows AORs with 95% CIs for key covariates of Model 2, which predicted positive COVID-19 cases using only demographic data, clinical findings, and laboratory test results as covariates (AUC 0.88 95% CI, 0.83-0.93). Adapted and reproduced by permission of Oxford University Press on behalf of the Infectious Diseases Society of America. Please visit: https://academic.oup.com/article/71/15/786/5811426/external icon. OUP and the IDSA are not responsible or in any way liable for the accuracy of the adaptation. Licensee is solely responsible for the adaptation in this publication/reprint.
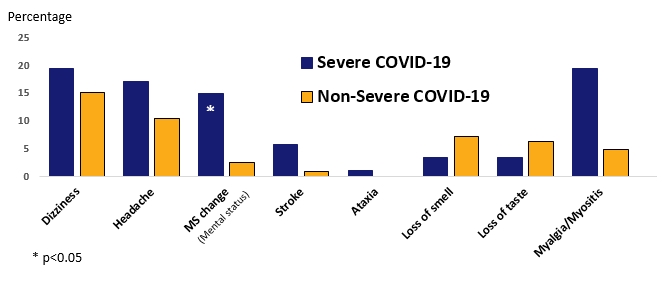
Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China: A retrospective case series study.external iconMao et al. JAMA Neurology (April 10, 2020).
Key findings:
- Among hospitalized adults with COVID-19, 36% had neurological symptoms or myositis.
- Among those with severe COVID-19, 5%–20% had mental status changes, stroke, or myositis.
Methods: Case series of 214 hospitalized adults with lab-confirmed COVID-19 in three hospitals in Wuhan, China; 41% had severe illness (January 15 to February 19, 2020).
Implications: The high prevalence of neurologic conditions among hospitalized COVID-19 patients may warrant post-hospitalization needs for physical rehabilitation and skilled nursing.
Figure:
Note: Adapted from Mao et al. Nervous system symptoms among patients with COVID-19. Reproduced with permission from JAMA Neurol. doi:10.1001/jamaneurol.2020.1127. Copyright©2020 American Medical Association. All rights reserved.
PEER-REVIEWED
Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: An observational cohort studyexternal icon. To et al. Lancet Infectious Diseases (March 23, 2020).
Key Findings:
- Patient-collected saliva (“posterior oropharynx”, PO) demonstrated highest viral load (VL) at symptom onset (5.2 log10 copies per mL at presentation) and then declined steadily thereafter (Figure 1).
- RNA was detected in PO samples ≥20 days after symptom onset in one-third of survivors.
- Peak VL levels tended to be higher among older patients (Figure 2).
Methods: 23 patients with lab-confirmed COVID-19 in Hong Kong self-collected first morning “deep throat” saliva samples by clearing throat and expectorating under nurse supervision.
Implications: Self-collected oropharyngeal saliva samples may be feasible and more acceptable. High VL at illness onset is consistent with other reports. Older persons may be more infectious than younger persons.
Figure 1
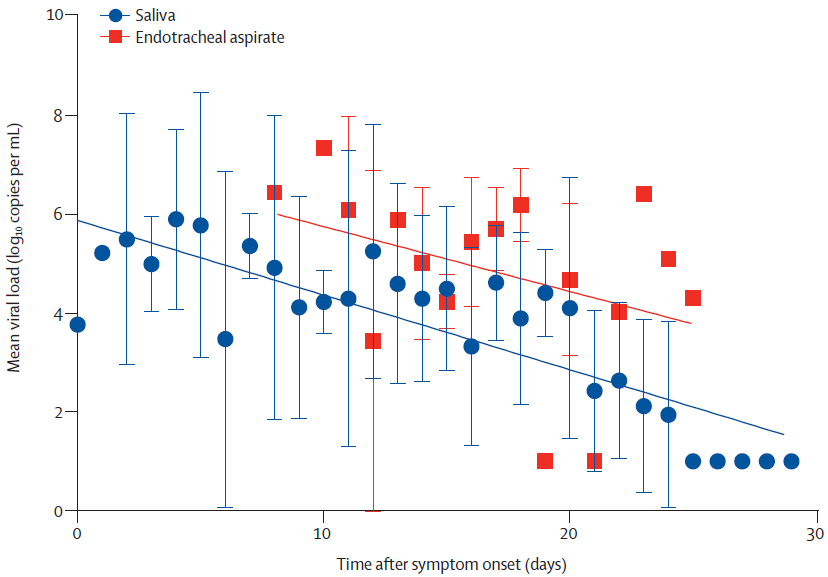
Figure 2
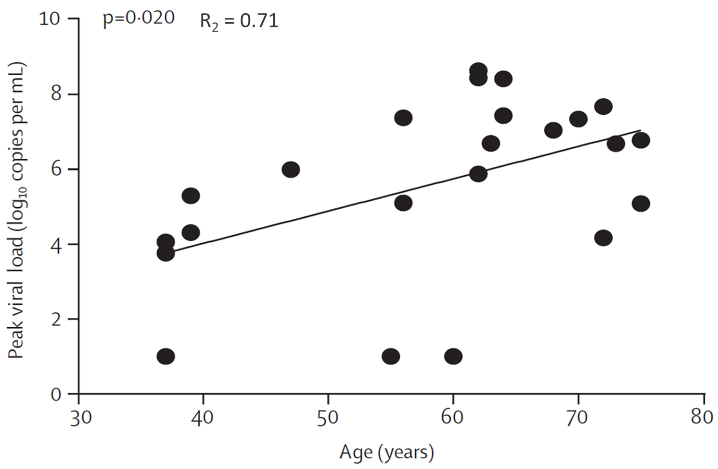
Note: Adapted from To et al. Figure 1. Temporal profile of serial viral load for all patients (n=23). Figure 2. Correlation between peak viral load and age. This article was published in Lancet Infectious Diseases, Volume 20, Issue 5, To et al., Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: An observational cohort study, P565-574, Copyright Elsevier 2020. This article is currently available at the Elsevier COVID-19 resource center: https://www.elsevier.com/connect/coronavirus-information-centerexternal icon.
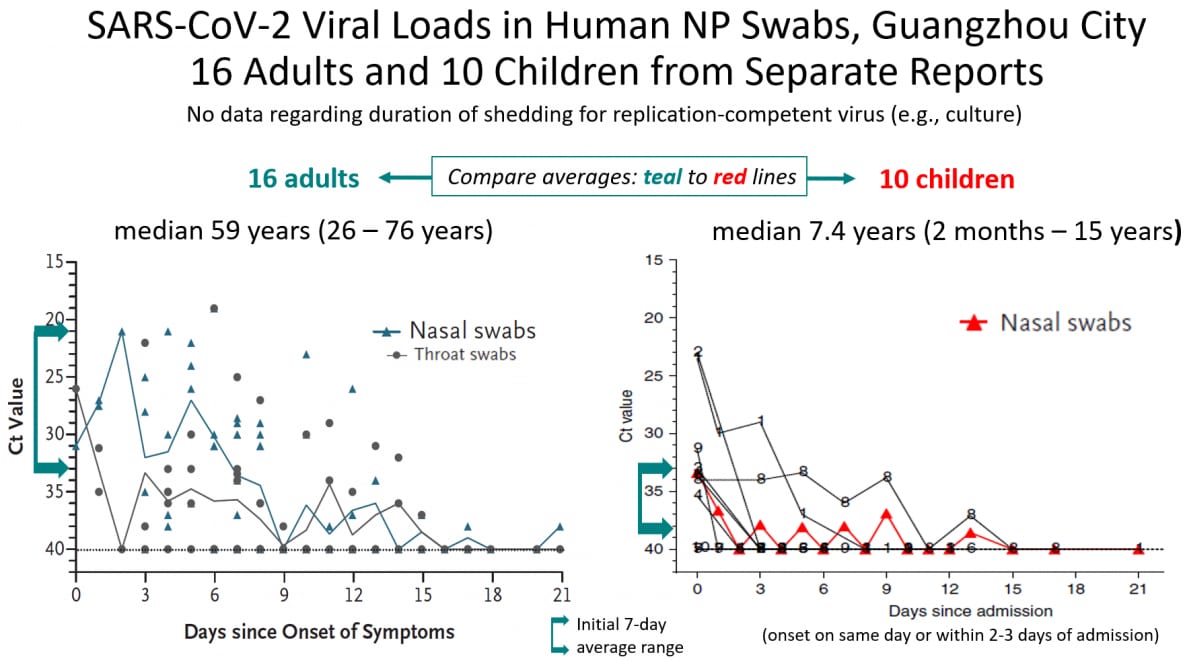
Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding.external iconXu et al. Nature Medicine (March 13, 2020).
Key findings:
- Among 10 children with lab-confirmed SARS-CoV-2 infection with relatively mild symptoms and few laboratory abnormalities, Ct values in serial NP swabs were lower than among a sample of 16 adult residents from the same city (Guangzhou).
Methods: Case series of hospitalized children identified through screening of contacts. Limitations: Small convenience sample and viral cultures not performed.
Implications: Children may have lower SARS-CoV-2 viral burden in nasopharynx after illness onset and during illness, and thereby be less infectious than adults.
Figure:
Note: Adapted from Zou et al. (SARS-CoV-2 viral load in upper respiratory specimens of infected patientsexternal icon, NEJM) and Xu et al available from NEJM 2020; 382:1177-1179. DOI: 10.1056/NEJMc2001737. Copyright © 2020 Massachusetts Medical Society. Reprinted with permission from Massachusetts Medical Society. Xu et al. available via Nature Public Health Emergency Collection through PubMed Central.
- Lurie et al. Developing COVID-19 vaccines at pandemic speedexternal icon. NEJM. On developing a vaccine for COVID-19 at “pandemic” speed compared with traditional vaccine development paradigm.
- Dong et al. Public mental health crisis during COVID-19 pandemic, China. Emerging Infectious Diseases. On the importance of including emergency psychological crisis interventions during (COVID-19) pandemic preparedness & response.
- Day M. COVID-19: Identifying and isolating asymptomatic people helped eliminate virus in Italian villageexternal icon. Universal and repeat testing along with implementation of quarantine/isolation of positive cases (including 50%-75% of asymptomatic persons) reduced transmission in a completely isolated village of 3000 people in northern Italy.
Disclaimer: The purpose of the CDC COVID-19 Science Update is to share public health articles with public health agencies and departments for informational and educational purposes. Materials listed in this Science Update are selected to provide awareness of relevant public health literature. A material’s inclusion and the material itself provided here in full or in part, does not necessarily represent the views of the U.S. Department of Health and Human Services or the CDC, nor does it necessarily imply endorsement of methods or findings. While much of the COVID-19 literature is open access or otherwise freely available, it is the responsibility of the third-party user to determine whether any intellectual property rights govern the use of materials in this Science Update prior to use or distribution. Findings are based on research available at the time of this publication and may be subject to change.