The Economics of Injury and Violence Prevention

Health economics examines the costs and consequences of health issues, connecting public health science to real-world applications. It is used to develop policies and programs that promote healthy lifestyles and positive health outcomes that are also cost-effective for individuals, states, and the nation.
CDC’s Injury Center applies health economics to the study of opioid overdoses, suicide, child abuse and neglect, intimate partner violence, older adult falls, traumatic brain injury, motor vehicle crashes, and other causes of injuries and violence. We use health economics to identify, measure, value, and compare the costs and consequences of injuries and prevention strategies.
The 2019 cost of injury in the U.S. was $4.2 trillion, according to a report in CDC’s Morbidity and Mortality Weekly Report. The costs include spending on health care, lost work productivity, as well as estimates of cost for lost quality of life and lives lost.
A separate report estimates the cost of fatal injuries for states. The states with the highest per capita 2019 cost of fatal injuries were West Virginia, New Mexico, Alaska, and Louisiana. The states with the lowest fatal injury costs were New York, California, Minnesota, Nebraska, and Texas. All states face substantial avoidable costs due to injury deaths.
You can use WISQARS to explore data on fatal and nonfatal cost of injury:
- Select a filter, such as data year, age, and geography
- Compare costs by mechanism and intent of injury
- Save and share cost data files
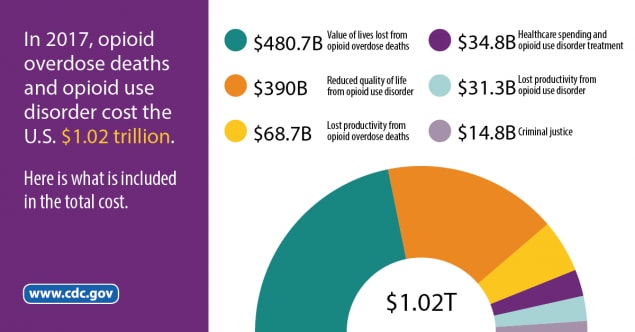
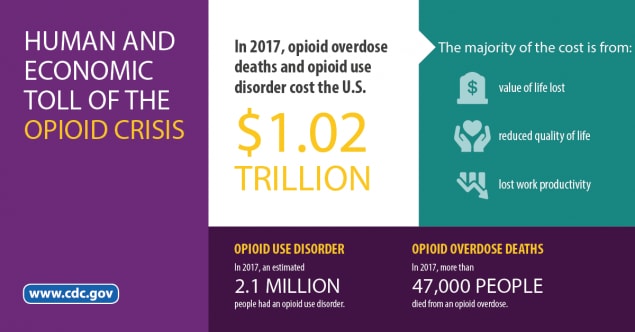
Fatal opioid overdoses and opioid use disorder cost the United States $1.02 trillion in 2017. The most complete accounting to date of America’s opioid crisis was released by CDC in the journal Drug and Alcohol Dependence. Costs for spending on health care, opioid use disorder treatment, criminal justice, and lost work productivity, as well as estimates of cost for lost quality of life and lives lost were computed in this study.
This CDC study expands and updates two prior estimates of the cost of the opioid crisis: a 2016 CDC economic cost study and a 2017 report released by the White House Council of Economic Advisors. In 2017, more than 2.1 million people over age 12 had an opioid use disorder, and over 47,000 opioid overdose deaths occurred.
Key findings include:
- The value of life lost due to overdose deaths was $480.7 billion.
- Opioid use disorder accounted for $471.0 billion.
- Almost $35 billion was spent on health care and opioid use disorder treatment.
- Healthcare costs were $31.3 billion
- Opioid use disorder treatment was $3.5 billion
- Criminal justice spending accounted for $14.8 billion.
For more information on Opioid Overdose, visit www.cdc.gov/opioids.
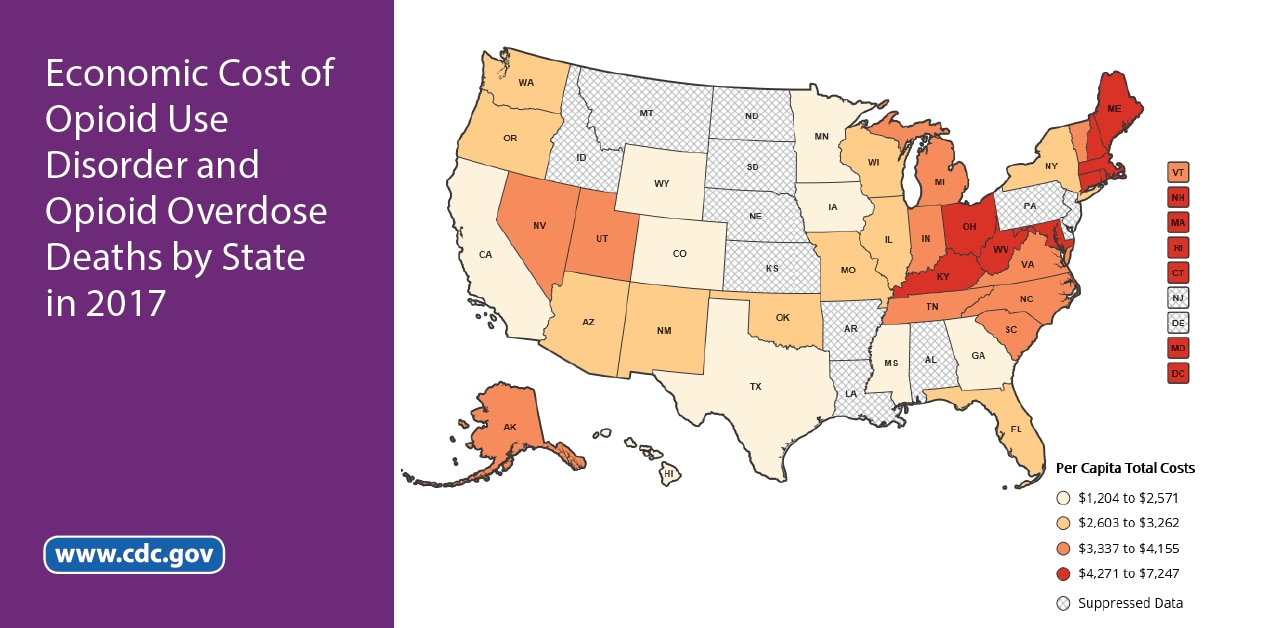
Fatal opioid overdoses and opioid use disorder had a significant economic impact on some states in 2017. Researchers focused on the state-level opioid crisis in a report in CDC’s Morbidity and Mortality Weekly Report. The costs were computed by state for spending on health care, opioid use disorder treatment, criminal justice, and lost work productivity, as well as estimates of cost for lost quality of life and lives lost.
You can explore a data map of the state-level costs of opioid use disorder and fatal opioid overdoses in 2017:
- Select a state to view costs of opioid use disorder and fatal opioid overdoses
- Compare cost data across states
- Save and share state-level cost data as a table or image
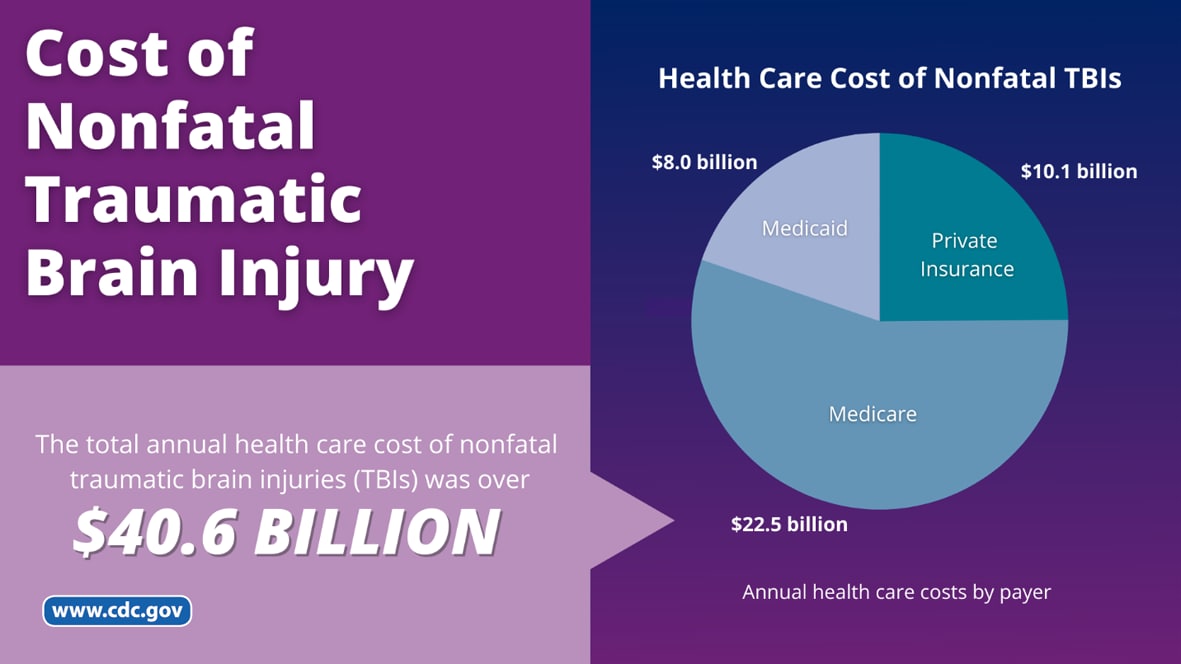
Traumatic brain injury (TBI) is a disruption in the normal function of the brain that can be caused by a bump, blow, or jolt to the head, or penetrating head injury. Everyone is at risk for a TBI. TBIs substantially contribute to health care costs each year. A CDC study in the journal Medical Care estimated the annual health care cost of nonfatal TBIs by severity level among children and adults in 2016 during the year following a TBI diagnosis.
Key findings include:
- The total annual health care cost of nonfatal TBIs was over $40.6 billion.
- Healthcare costs include $10.1 billion by private insurance, $22.5 billion by Medicare, and $8 billion by Medicaid.
- More than 2 million nonfatal injuries were related to TBI.
Unintentional and violence-related injuries cause more than 240,000 deaths among people of all ages in the United States each year. Unintentional injuries are the leading cause of death for people ages 1-44.
A greater number of people experience nonfatal injuries each year. Nonfatal injuries can cause life-long mental, physical, and financial problems.
Fatal and nonfatal injuries are costly. A recent CDC study estimated the medical care cost of U.S. fatal and nonfatal injuries by type of injury.
- The average medical cost of all fatal injuries was approximately $41,570 per hospitalized patient and $6,880 per emergency department patient. Each year approximately 50,000 people die in hospitals from injuries, and approximately 30,000 die in emergency departments from injuries.
- The average one-year medical cost of all nonfatal injuries per person initially treated in an emergency department was approximately $6,620. Each year there are approximately 28 million emergency department visits for nonfatal injuries.
Injuries can cause lost productivity at work. A recent CDC study estimated the lost work productivity cost of U.S. nonfatal injuries by type of injury.
People treated for nonfatal injuries in an emergency department lose on average 11 days of work, valued at $1,590 per person.
Youth violence takes a toll on individuals, families, and communities—and comes at a high economic cost to the nation. A new research letter in JAMA Pediatrics reports on the economic costs of youth violence, finding that costs rose from $105 billion in 2015 to $122 billion in 2020. The greatest share of the costs were firearm homicides among males.
More than 30,000 people are killed in motor vehicle crashes each year in the United States. These injuries and deaths have a high economic impact for states. Many evidence-based strategies can significantly reduce the number of injuries and deaths from motor vehicle crashes and their related costs.
See the cost of deaths from motor vehicle crashes and which age groups and types of road users account for the largest portion of these costs in each state: State-Specific Costs of Motor Vehicle Crash Deaths.
Calculate the expected number and monetized value of 14 effective motor vehicle injury prevention interventions with MV PICCS 3.0: Motor Vehicle Prioritizing Interventions and Cost Calculator for States (MV PICCS).

Motor Vehicle Prioritizing Interventions Cost Calculator for States (MV-PICCS)

An estimated 1,720 children died from abuse and neglect in 2017, and about 674,000 children were identified as victims of child abuse or neglect by child protective service agencies. Safe, stable, nurturing relationships and environments are essential to preventing child abuse and neglect, and policies and programs supportive of children and families can help.
Estimate the local health and financial impact of selected child abuse and neglect prevention programs by state. These programs are among those with the best available evidence and have published per-child or per-family costs: Child Abuse and Neglect (CAN) Prevention Program Cost Calculator.

Child Abuse and Neglect (CAN) Prevention Program Cost Calculator

A recent CDC study showed that the estimated medical cost of older adult falls across the U.S. healthcare system is $50 billion annually. This includes $38 billion paid by Medicare and Medicaid and $12 billion paid by private and other payers.
Older adult falls can be prevented. Initiatives like Stopping Elderly Accidents, Deaths, and Injuries (STEADI) can improve health and decrease the future economic burden of older adult falls. STEADI recommendations include screening older adults to identify their fall risk, assessing at‐risk individuals to identify their modifiable fall risk factors, and intervening by using effective strategies to reduce fall risk factors.
Cost of Injuries
- Economic Burden of US Youth Violence Injuries
- Average lost work productivity due to nonfatal injuries by type in the USA
- Average medical cost of fatal and nonfatal injuries by type in the USA
- Cost of Injury Reports: Customize and Generate Data Tables
- Economic cost of injury, United States, 2019
- State-level economic costs of fatal injuries, United States, 2019
Cost of Violence
- Lifetime economic burden of intimate partner violence among US adults
- Short-term lost productivity per victim: intimate partner violence, sexual violence, or stalking
- Lifetime economic burden of rape among US adults
- The impact of the low-income housing tax credit on children’s health and wellbeing in Georgia
- The economic burden of child maltreatment in the United States, 2015
- Cost-benefit analysis of two child abuse and neglect primary prevention programs for US states
- Economics and violence against children, findings from the Violence Against Children Survey in Nigeria
- Effect of the earned income tax credit on hospital admissions for pediatric abusive head trauma, 1995-2013
- Paid family leave’s effect on hospital admissions for pediatric abusive head trauma
- Annual cost of U.S. hospital visits for pediatric abusive head trauma
Cost of Unintentional Injuries
- State-Level Economic Costs of Opioid Use Disorder and Fatal Opioid Overdose — United States, 2017
- Costs of Nonfatal Traumatic Brain Injury in the United States, 2016
- Estimating the Economic Burden Related to Older Adult Falls by State
- Medical costs of fatal and nonfatal falls in older adults
- Preventing deaths and injuries from house fires: A cost-benefit analysis of a community-based smoke alarm installation programme
- The Economic Burden of Prescription Opioid Overdose, Abuse, and Dependence in the United States, 2013
- Payments for opioids shifted substantially to public and private insurers while consumer spending declined, 1999-2012
- A cost-benefit analysis of three older adult fall prevention interventions