Congolese Refugee Health Profile
Priority Health Conditions
A list of priority health conditions to consider when caring for or assisting Congolese refugees.
Background
Group Origins, Language and Literacy, Religious Beliefs, Caste System, Family and Kinship, Gender Roles, Cultural Approach to Healthcare
Population Movements
From DRC to Burundi, Rwanda, Tanzania, and Uganda, From DRC to the United States
Healthcare Access and Conditions in Refugee Camps
Immunizations, Reproductive Health, Sexual-and Gender- Based Violence, Female Genital Cutting
Medical Screening of US-Bound Refugees
Visa Medical Examination, Pre-Departure Medical Screening, Pre-Embarkation Checks, Surveillance, Post-Arrival Medical Screening
Health Information
General Health Information, Communicable Disease, Non-Communicable Disease, Nutrition, Mental Health
Priority Health Conditions
Available data indicate that the health conditions listed below are priority health conditions that healthcare providers should consider when caring for or assisting Congolese refugees. These conditions are considered more prevalent among this population.
Background
History of Conflict
The Democratic Republic of the Congo (DRC, formerly known as Zaire) is located in central Africa and is the largest country by land mass in sub-Saharan Africa 1. For nearly 2 decades, DRC has been divided by armed conflict as a result of the First and Second Congo Wars (1996–1997 and 1998–2003,) and the Kivu Conflicts in eastern DRC (2004–present).
Following the Rwandan genocide in 1994, millions of Rwandan refugees flooded into the eastern DRC. In 1996, Rwanda and Uganda invaded eastern DRC in an effort to locate the remaining perpetrators of the genocide, who were believed to be hiding in camps there. A coalition comprised of the Ugandan and Rwandan armies, along with Congolese opposition leader Laurent Kabila, eventually defeated Congolese dictator Mobutu Sese Seko and his army, and Laurent Kabila became president of DRC, ending the First Congo War in 1997. In 1998, President Kabila ordered Rwandan and Ugandan forces to leave the eastern DRC, fearing invasion of the resource-rich territory by the 2 regional powers 1. This move sparked the beginning of the Second Congo War. With the involvement of 9 African countries and more than 20 armed militia groups, the Second Congo War is often referred to as “Africa’s World War” and is considered to be the deadliest global conflict since World War II 2.
Despite the official end of the Second Congo War in 2003, various rebel groups and rogue elements of the Congolese army continue to commit serious human rights abuses in eastern DRC, primarily in the provinces of North and South Kivu, Orientale, and Katanga 2. Kivu province is ethnically diverse, with groups having a history of persecution (primarily the Banyamulenge and Tutsi) making up the majority in the region 2. The Banyamulenge, Congolese of Rwandan origin, have faced a long history of discrimination in DRC and, along with ethnic Tutsi and Hutu from Rwanda, are often denied citizenship and other rights. These groups have also been discriminated against based on their perceived association with Rwandan-backed rebel groups, which many blame for the unrest in the region 2. Other groups, such as the Bembe and Bashi, have also faced persecution on a smaller scale due to their large presence in the conflict area. The ongoing unrest and instability in DRC has been described by the United Nations as one of the world’s worst humanitarian crises and continues to cause hundreds of thousands of displaced persons to seek refuge in neighboring countries, including Burundi, Rwanda, Tanzania, and Uganda 2.
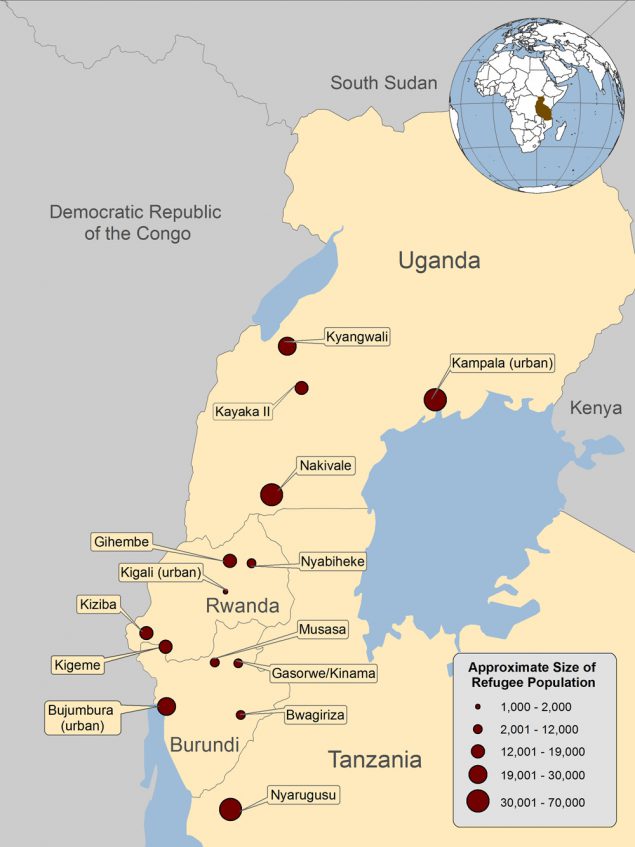
Figure 1: Location of the Democratic Republic of Congo, Burundi, Rwanda, Tanzania, and Uganda
Language and Literacy
While French is the official language of DRC and 4 national languages are considered to be primary languages (Lingala, Kiswahili, Kikongo, and Tshiluba) 1, the majority of refugees resettling through the United States Refugee Admissions Program (USRAP) will speak Kinyarwanda, because they are from eastern DRC 2. Many Congolese refugees are multilingual, speaking their native language as well as Kiswahili or other regional languages. Refugees are often exposed to English through school and the media; however, proficiency in English is expected to be minimal. Data from surveys conducted by the Resettlement Support Center in Africa (RSC-Africa) show that 59% of Congolese refugees have no oral English skills and an even greater percentage have no ability to read (65%) or write (66%) in English 3. Most Congolese adults arriving through the USRAP will not have had access to secondary education. Data from RSC-Africa show that 70% of Congolese over 18 years of age reported not having a high school diploma or higher level of education. Similar results from an assessment of 416 refugees, conducted by the Centers for Disease Control and Prevention (CDC) and the International Organization of Migration (IOM) (unpublished data), show that 14% of refugees in Rwanda had no formal education at all, 54% had some primary schooling, 31% had a high school diploma, and 1% had a university degree. It is known that girls attend schools at lower rates in DRC, so it is likely that the majority of refugees with no primary or high school education and low literacy levels are female.
Religious Beliefs
Approximately 70% of the general population in DRC is Christian and refugees being referred for US resettlement are overwhelmingly Christian (95%), with 80% of those Christians identifying as Protestant 2. Of these, a large majority identify as Pentecostal and Seventh Day Adventists. Approximately 4% of refugees identify as Muslim. Few refugees follow indigenous beliefs exclusively; however, traditional belief systems are sometimes incorporated into religious practices and are familiar to a majority of Congolese 2.
Family and Kinship
A typical Congolese household includes not only immediate family, but generally also includes extended family and sometimes those not related by blood. The Congolese interpret family in a much broader sense than Westerners. Children are considered a sign of prosperity and good fortune for the community, so families are often large, with a fertility rate of 5 children born per Congolese woman 1. Care and discipline of children are considered shared responsibilities of the whole community, therefore it is not uncommon for adults who are not biologically related to a child to correct poor behavior and provide input on their upbringing.
Gender Roles
In the past, gender roles have typically been well defined, with men protecting and providing for the family and women traditionally taking care of children and tending to household chores. However, as the conflict in DRC expanded in the mid-1990’s, traditional roles began to change as women were forced to become the primary source of financial support for the family. It is no longer uncommon for Congolese women to work outside of the home, usually selling handcrafts or running small businesses. While education is accessible to both genders in urban areas, there continues to be a male bias and women still tend to remain unequal in most sectors of society 2.
Cultural Approach to Health Care
Western medicine is generally well-received in Congolese culture, although significant barriers (e.g., geographic location to health centers, high cost) often prevent access to quality healthcare and treatment within the DRC 2. As a result, the Congolese may seek traditional medicines in lieu of, or in combination with, Western therapies. Medical infrastructure is limited mostly to urban areas and care is only delivered after payment in cash, therefore an inability to access or pay for care may lead patients to use herbal medicines or consult with traditional spiritual healers (Feticheur) to resolve illnesses. Christian Congolese are known to rely heavily on prayer 2. Mental illness is often considered a curse (sometimes believed to be caused by supernatural elements or the result of witchcraft) and is not openly discussed. For more information on mental health, refer to the mental health section of this profile.
Additional Resources
For more information about the orientation, resettlement and adjustment of Congolese refugees, visit the Cultural Orientation Resource Center, which is maintained by the organization of the same name.
Population Movements
Movement Out of DRC to Burundi, Rwanda, Tanzania, and Uganda
Since January 2013, UNHCR reports that more than 400,000 Congolese nationals have sought refuge outside of DRC 4. Although Congolese refugees reside in many different countries in sub-Saharan Africa, the 4 primary host countries providing asylum to Congolese refugees are Uganda (113,000), Rwanda (68,000), Tanzania (59,000), and Burundi (38,000) 4. There are several large refugee camps or settlement areas within each host country, with Nakivale (Uganda) and Nyarugusu (Tanzania) holding the largest number of Congolese refugees in the “Great Lakes” region of central/eastern Africa (Figure 2). The majority of Congolese refugees from DRC live in camp-based settings; however, a growing number in Rwanda and Uganda are now living in settlements in urban settings as encampment policies are lifted and host governments are allowing more refugees to move freely within the country. For example, Uganda has experienced a fivefold increase in the number of refugees living in Kampala from 2007–2013, with 48,000 Congolese now living in Uganda’s capital city. In the beginning of 2012, an escalation of conflict in the Kivu region of DRC resulted in almost 70,000 new refugee arrivals into camps in Burundi, Rwanda, and Uganda. As fighting continues, the numbers are expected to grow.
Figure 2. Location and size of major refugee populations in Burundi, Rwanda, Tanzania, and Uganda, 2013*
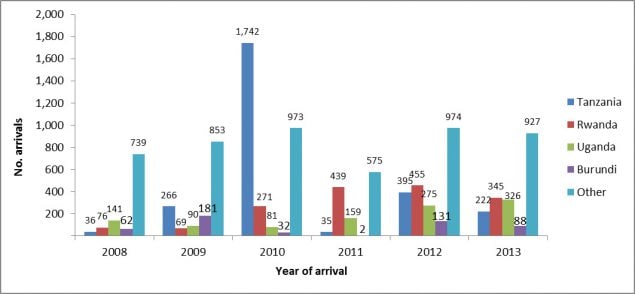
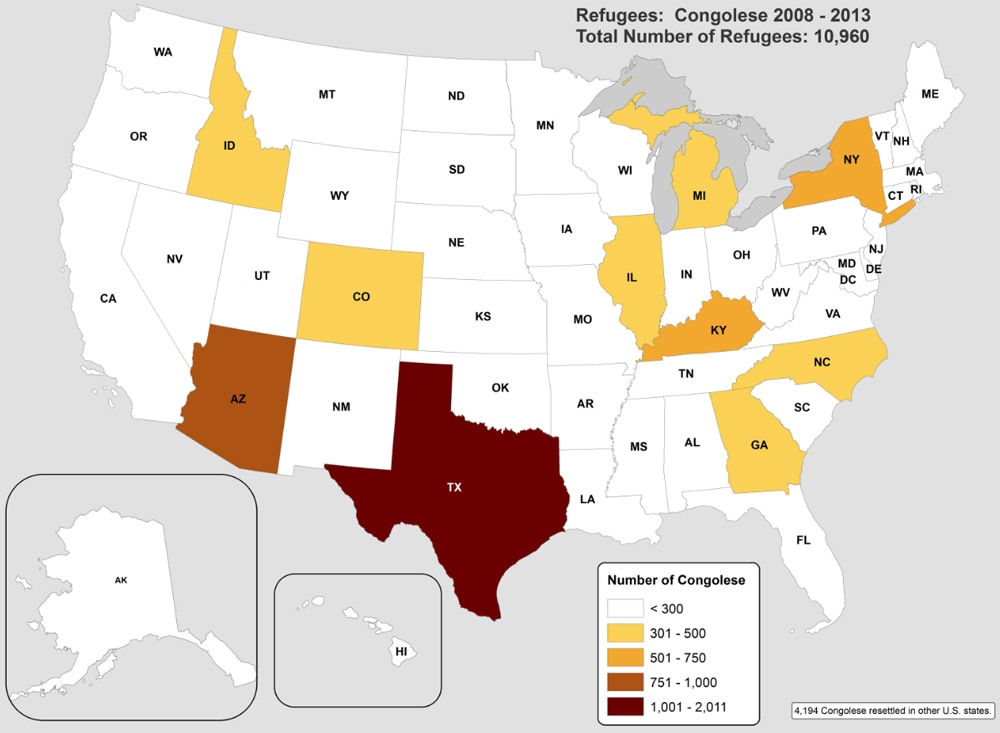
Resettlement of Congolese Refugees in the United States
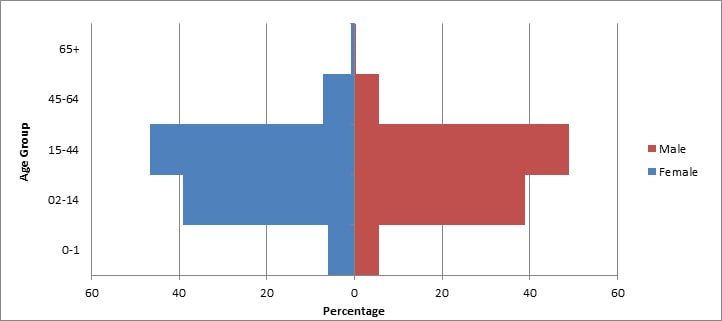
In 2000, the USRAP began resettling small numbers of Congolese refugees in the United States, with the largest caseloads coming from Tanzania 5. From 2008–2013, approximately 11,000 Congolese refugees arrived in the United States from 36 countries (Figure 3). Refugees have been resettled in multiple states, with Texas, Arizona, Kentucky, and New York each receiving ≥6% of total arrivals (Figure 4). However, once refugees arrive in a state, they are free to relocate elsewhere, and secondary migration to join an already established Congolese community is common. Most (55%) Congolese refugees who resettled in the United States during this period were young adults aged 15–44 years and 40% were children under 15 years old (Figure 5). Because of the long history of violence in DRC and the recent escalation of conflict in the Kivu region, durable solutions such as repatriation do not appear likely for Congolese refugees anytime in the near future. In 2012, the US Bureau of Population, Refugees, and Migration (PRM) announced a new initiative to resettle approximately 50,000 Congolese refugees in the United States over the next 5 years (2013–2018).
Figure 3: Congolese refugee arrivals in the US, 2008–2013 (n=10,960)
Figure 5: Age distribution for Congolese refugees originating from refugee camps in Burundi, Rwanda, Tanzania, and Uganda, 2008–2012 (N=4,938)
Healthcare Access and Conditions in Refugee Camps
Refugee camps in Burundi, Rwanda, Tanzania, and Uganda (the 4 top countries sending Congolese refugees to the United States) each have different nongovernmental organizations (NGOs) that provide inpatient and outpatient medical care and community health education to camp residents. UNHCR collects health information in refugee camps and reports this information in their Health Information System (HIS). Some services offered by the NGOs include pediatrics and integrated management of childhood illness, reproductive health, psychiatric consultation, emergency medical services and referrals, basic laboratory services, tuberculosis (TB) management (directly observed therapy with first-line agents), voluntary testing and counseling for human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) with referral services for antiretroviral treatment, and nutrition promotion.
Immunizations
Burundi, Rwanda, Tanzania, and Uganda administer vaccines in line with the World Health Organizations (WHO) Expanded Program on Immunization. Precise estimates of vaccine coverage in camps are difficult to obtain because the exact number of people living in the camps is not known. Supplemental mass immunization campaigns are also carried out by NGOs following announcements from the host country governments. If appropriate documentation from the refugee is available, the vaccinations given to that person will be noted on the US Department of State’s form DS-3025, which is included in the health information packet provided to each refugee before he or she departs. DS forms are the forms used by physicians to complete the overseas medical screening examinations. The health information packet is supplied by IOM and contains the refugees’ medical screening examination information for reference upon the refugees’ arrival in the United States. Additionally, IOM’s Pre-Departure Medical Screening Form will note vaccination information for individual refugees. All vaccination information will also appear in CDC’s Electronic Disease Notification system (EDN).
Reproductive Health
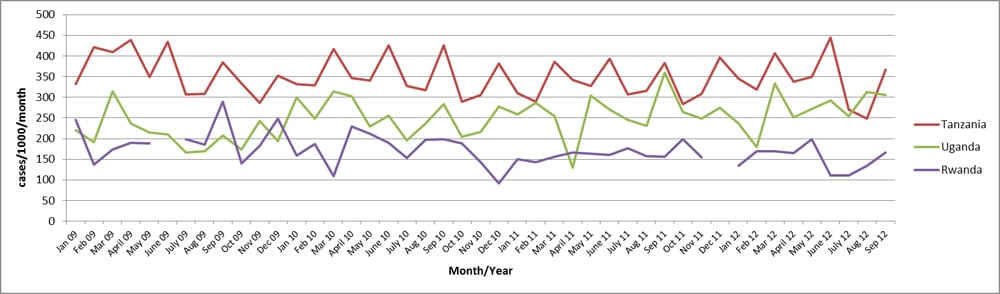
Birthrates in refugee camps in Rwanda, Tanzania, and Uganda vary considerably (Figure 6). There are no data available for Burundi. The percent of births that are attended by a skilled midwife or a health worker with midwifery skills varies depending on the camp and country. In 2012 the percentages of births attended by a skilled attendant in the refugee camps were: 100% for Burundi, 92% for Rwanda, 100% for Tanzania, and 93% for Uganda 6. It should be noted that the above statistics apply to refugees from multiple countries that are living in the camps in Burundi, Rwanda, Tanzania, and Uganda, not refugees exclusively from DRC. Additionally, Congolese refugees may not feel comfortable discussing sexuality and gynecological issues with non-family members, especially male clinicians.
Figure 6: Crude birth rates in refugee camps in Rwanda, Tanzania, and Uganda by month, 2009–2012
The conflict in eastern DRC has been marked by numerous human rights abuses, including sexual and gender-based violence (SGBV). Reports include gang rapes, sexual slavery, purposeful mutilation of women’s genitalia, and killing of rape victims 7. One study estimated that 48 women are raped every hour in DRC, which is a little over 1,150 women a day 8. According to a population-based study conducted in the eastern DRC in 2010, rates of reported sexual violence were 40% among women, and 24% among men. In addition to sexual violence, 20% of the adult population in the study reported serving as combatants at some point in their lifetime, the majority of whom reported being conscripted into armed groups 9. The brutality of such sexual violence has resulted in unprecedented rates of trauma, physical injury including fistula, pregnancy, infertility, genital mutilation, and HIV/AIDS and other sexually transmitted diseases. 50% of rape victims in the DRC are believed not to have access to medical treatment 10.
The threat of SGBV is also present in the refugee camp environment, particularly where women and girls must travel on foot outside the camps to collect firewood, risking harassment, rape, and other abuses. Service providers in Rwanda noted that limited work opportunities force some women and girls into abusive relationships or “survival sex,” i.e., coerced sex in exchange for temporary access to food, shelter, or protection. Additionally, a refugee’s access to mental health services in these camps is often extremely limited; in 1 camp, 1 psychological nurse may be responsible for 16,000 refugees 11).
The psychosocial consequences of being raped are devastating. Fear, shame, insomnia, and nightmares are frequently noted among sexual violence survivors. In eastern DRC, rape is highly stigmatized and social problems include spousal abandonment, inability to marry, and ostracism by the community. Spousal and community abandonment can lead to isolation and homelessness 12.
However, despite experiences of SGBV being common within the Congolese refugee population, SGBV is an extremely sensitive issue, and associated with much shame. Service providers with experience treating these patients recommend that public health officials not ask intrusive personal questions upon the patient’s initial screening and early visits, but wait until the patient trusts the service providers.
While much attention has been paid to sexual violence allegedly committed by paramilitary personnel and soldiers, intimate partner sexual violence (IPSV) has been less visible. A Demographic and Health Survey conducted in 2007 suggests that this is a particularly large problem in the DRC, with approximately 35% of women reporting IPSV 13. From a nationally representative household survey conducted in all 11 provinces of DRC in 2010, the total number of women estimated to have suffered IPSV ranged from 3.07 million to 3.37 million, with the number of women reporting IPSV roughly 1.8 times the number of women reporting rape 14. This result is in line with international research indicating that intimate partner sexual violence is the most pervasive form of violence against women 15.
Female Genital Cutting
The practice of female genital cutting (FGC, also referred to as female genital mutilation), which is the partial or total removal of the external female genitalia or other injury to the female genital organs for cultural, religious, or non-therapeutic reasons, is known to exist in the DRC, but current data on the prevalence of FGC are not available (WHO). However, in a 2007 report, UNICEF stated that the prevalence of FGC in the DRC was estimated to be less than 5% 16.
Medical Screening of US-Bound Refugees
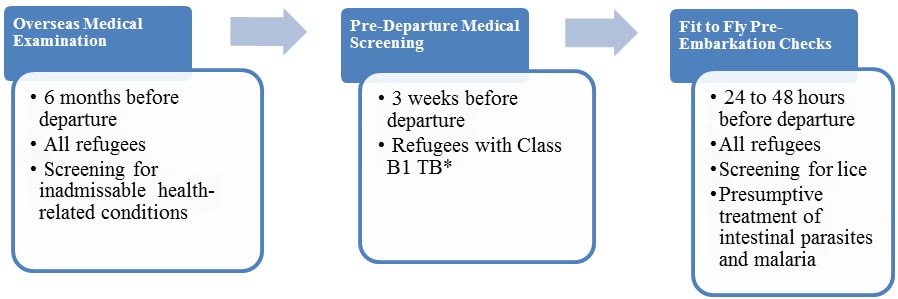
Congolese refugees who have been identified for resettlement in the United States receive medical assessments (Figure 7). Some assessments occur several months prior to the refugees’ departure and some occur immediately before departure to the United States.
Figure 7: Medical assessment of United States-bound Congolese refugees
Overseas Medical Examination
As overseas medical examination is mandatory for all refugees coming to the United States and must be performed according to the CDC’s Technical Instructions. The purpose of the medical examination is to identify applicants with inadmissible health-related conditions, and they are performed by panel physicians who are selected by US Department of State consular officials. CDC provides the regulatory and technical oversight and training for all panel physicians. Information collected during the refugee overseas medical examination is reported to EDN and is available to state refugee health programs in the states where the refugees are resettled.
Refugees do not have to receive any vaccines before they are admitted into the United States. Vaccines given to Congolese refugees during the overseas medical examination vary depending on the country where they reside during the examination.
Pre-Departure Medical Screening
Congolese refugees receive a pre-departure medical screening about 3 weeks before leaving for the United States if they have been previously diagnosed with class B1 TB (TB fully treated using directly observed therapy, or abnormal chest x-ray with negative sputum smears and cultures, or extrapulmonary TB). The screening includes a repeat physical examination with a focus on TB signs and symptoms, chest x-ray, and sputum collection for acid-fast bacilli smear microscopy.
Pre-Embarkation Checks
IOM clinicians perform 2 pre-embarkation checks within 48 hours of the refugee’s departure for the United States to assess his or her fitness for travel. During this assessment, the clinician administers presumptive therapy for intestinal parasites (worms) and malaria. Presumptive therapy is treatment of individuals who have a high likelihood of asymptomatic or sub-clinical infection without, or prior to, results from confirmatory laboratory tests.
Congolese refugees departing from Kenya, Tanzania, Uganda, and Rwanda receive pre-departure treatment for soil-transmitted helminths, schistosomiasis, and malaria according to current CDC guidance. Except when contraindicated, refugees are treated for soil-transmitted helminths with a single dose of albendazole, schistosomiasis with standard dose of praziquantel (divided into two doses for better tolerance), and malaria with a 6-dose schedule of artemether-lumefantrine. Management of Strongyloides in Congolese refugees is deferred until the refugee’s arrival in the United States. Guidance for this is available in the Domestic Intestinal Parasite Screening Guidelines. Refugees from sub-Saharan Africa are normally given presumptive treatment for infection with Strongyloides with ivermectin; however, since DRC is a Loa loa-endemic country, Congolese refugees should not receive presumptive ivermectin for strongyloidiasis prior to departure because of the risk of encephalopathy.
Information on presumptive therapy for intestinal parasites will be noted on IOM’s Pre-Departure Medical Screening Form, which is included in the packet provided to each refugee before he or she departs. Information on presumptive therapy for intestinal parasites given to refugees will also appear in EDN.
Surveillance
Active surveillance for communicable diseases of public health significance (such as TB) takes place through all phases of overseas medical processing. This surveillance is designed to identify refugees with conditions that may result in deferred travel or other interventions. In addition, when disease outbreaks occur in the camps, IOM coordinates with the local implementing partners to identify refugees in the resettlement program who may be affected. Depending on the nature of the disease outbreak, various interventions may then be used, such as deferral of travel, additional vaccinations, and presumptive or directed therapy.
Post-Arrival Medical Screening
Once refugees have arrived in the United States, CDC recommends that they receive a post-arrival medical screening (domestic medical screening) within 30 days. The Office of Refugee Resettlement reimburses providers for screenings conducted during the first 90 days after arrival. The purpose of these more comprehensive examinations is to identify conditions for which refugees may not have been screened during their overseas medical examinations. The examinations also introduce refugees to the US healthcare system. CDC provides guidelines and recommendations while state health departments oversee and administer the domestic medical screenings. State refugee health programs determine who conducts the examinations within their jurisdiction; these may be performed by health department personnel or private physicians. Data from the screenings are collected by most state health departments.
Health Conditions for Healthcare Providers to Consider in Post-Arrival Medical Screening of Congolese Refugees (h4)
In addition to the standard guidelines for post-arrival medical screening of newly arriving refugees, clinicians should consider the following health conditions.
Malaria
According to the current United States domestic screening guidelines for malaria, refugees who have received presumptive treatment prior to departure need no further evaluation for malaria unless they demonstrate signs or symptoms of infection. CDC recommends that Congolese refugees originating from other sub-Saharan African countries who have not received pre-departure therapy either receive presumptive treatment when they arrive or have laboratory screening with a blood smear.
Strongyloidiasis
CDC currently recommends that all United States-bound Congolese refugees either be presumptively treated OR tested and treated (if positive) for strongyloidiasis after arrival in the United States. Currently, only Congolese refugees departing from Kenya receive pre-departure treatment for strongyloidiasis.
The treatment of choice for Strongyloides infection is ivermectin, a single dose for 2 consecutive days. However, the management of Strongyloides infection in the Congolese refugees is complicated by the possibility of co-infection with the parasite Loa loa, also known as “eye worm.” Persons with a high blood level (microfilarial load) of Loa loa who are given ivermectin therapy can develop severe encephalopathy. Although this is rare, CDC recommends that a patient originating from, or transiting through, a Loa loa endemic country be tested prior to ivermectin use to ensure that he or she does not have a high microfilarial load. Please refer to the list of Loa loa-endemic countries.
Use one of these three approaches to address Strongyloides infection in Congolese who are at risk of co-infection with Loa loa infection:
- Presumptive treatment with ivermectin after testing for Loa loa – To diagnose Loa loa, a daytime blood smear (thick and thin, same test as for malaria) can be done between 10 a.m. and 2 p.m. If there are no Loa loa parasites observed, ivermectin may be safely used to presumptively treat the refugee.
- Presumptive treatment with “high-dose” albendazole without testing for Loa loa – Presumptively treat refugees with “high-dose” albendazole without testing for Loa loa infection. The dosing recommended for treatment of Strongyloides infection is albendazole 400 mg twice a day for 7 days.
- Test for Strongyloides, Loa loa and treatment if positive – Test the refugee for Strongyloides infection and only treat (for Strongyloides) those whose results are positive. Serology is the most sensitive test for detecting Strongyloides infection. Stool ova and parasite examination or stool agar culture may be used as additional tests but should not be used alone because of poor sensitivity. Those with positive test result (for Strongyloides) could either be treated with ivermectin (if a daytime blood smear is negative as described above) or with the 7-day course of albendazole.
For more information, please see the Domestic Intestinal Parasite Guidelines for refugees.
Schistosomiasis
Refugees originating in sub-Saharan Africa without a contraindication receive a treatment dose of praziquantel prior to departure, which presumptively treats a majority of infected individuals. Currently, those Congolese refugees from the asylum countries of Tanzania, Rwanda, Uganda, and South Africa should be receiving praziquantel prior to departure. However, a treatment dose of praziquantel is not 100% effective and any refugee with signs or symptoms of active disease, most often, a persistently elevated eosinophil count, may need further evaluation for schistosomiasis. Please see Presumptive Treatment and Screening for Strongyloidiasis, Schistosomiasis, and Infections Caused by Soil-Transmitted Helminths for Refugees for additional information on domestic medical screening.
Filariasis
The filarial diseases are caused by nematodes transmitted to humans, most commonly through black flies and mosquitoes. The 3 most common infections, all endemic to DRC, are loiasis, lymphatic filariasis, and onchocerciasis. The filarial infections are common in the DRC and co-infection is common. They may persist for a decade or more and some of the complications may be permanent. Most people infected with these nematodes will never develop symptoms. The most common clinical sign in refugees is a persistent elevated eosinophil count. Therefore, these parasites need to be considered in Congolese refugees with a persistent elevated eosinophil count and in those with symptoms more specific to each nematode.
Loiasis, (also known as “eye worm”), caused by the parasitic roundworm Loa loa, is transmitted by red (chrysops) flies and is endemic through most of DRC although it is particularly common in certain focal areas. Most infected individuals have no symptoms, but common clinical manifestations include an increased eosinophil count, recurrent episodes of transient itchy swellings (local angioedema) usually found on the limbs or near joints and sometimes referred to as “Calabar swellings”, and “eye worm”. Eye worm is the visible migration of the adult worm across the surface of the eye which may be associated with eye congestion, itching, pain, and light sensitivity. Other symptoms include generalized itching, hives, muscle pains, joint aches, fatigue, and the visible migrating worm under the surface of the skin. Infection does occur in the absence of an elevated eosinophil count.
Lymphatic filariasis, most commonly caused by the nematode Wuchereria bancrofti, is transmitted to humans by mosquito vectors. Lymphatic filariasis is distributed throughout DRC as well as all major East African countries of asylum. Most infected persons will never develop symptoms. The most common clinical manifestations are a persistently elevated eosinophil count, and a lymphedema that usually affects the legs but also occurs in the arms, breasts, and genitalia (especially hydrocele or swelling of the scrotum in males). Infection does occur in the absence of an elevated eosinophil count. When the swelling is accompanied by hardening and thickening of the skin it is commonly referred to as elephantiasis. This condition predisposes patients to bacterial infections.
Onchocerciasis, caused by Onchocerca volvulus, is transmitted to humans through the bite of a blackfly. Onchocerciasis is found throughout most of DRC as well as in areas of Burundi, Rwanda, Tanzania, and Uganda. Common clinical manifestations include generalized itching, nodules under the skin, rashes and, most concerning, visual changes (commonly known as “river blindness”). When larva die within the eye they initially cause reversible lesions of the cornea. However, with time they may result in permanent clouding of the cornea and blindness. In addition, inflammation of the optic nerve may occur, resulting in vision loss. Although an elevated eosinophil count is common, infection does occur in the absence of an elevated count.
Diagnosis and treatment of filariasis is complicated and beyond the scope of this document. Further information on each parasite may be obtained at the CDC Division of Parasitic Diseases. CDC also offers diagnostic and treatment assistance.
African Trypanosomiasis
African trypanosomiasis, also known as sleeping sickness, is an insect borne infection transmitted by tsetse flies. It is caused by microscopic parasites of the species Trypanosoma brucei. There are two subspecies of T. brucei, T.b. Rhodensiense (East African) and T.b. gambiense (West African). Refugees from the DRC may be at risk of West African trypanosomiasis (Trypanosoma brucei gambiense) where West African sleeping sickness is endemic, although most of the refugees report being from non-endemic areas of DRC. Depending on migration route, refugees may also be at risk for T.b. Rhodensiense which is most endemic in Tanzania, Uganda, Malawi and Zambia. T.b. Rhodensiense is less common and has a more acute onset and would be observed at the time of migration or shortly following arrival and would be characterized by fevers, headache, muscle and joint aches, enlarged lymph nodes and is frequently accompanied by a large sore (a chancre) at the bite site. There is relatively rapid clinical decline without treatment with mental disorientation, other neurologic symptoms, coma resulting in death within months.
T.b. gambiense, more common and of greater concern in refugees, since it is more common and may be more insidious occurring months to years after after infection. Symptoms of West African trypanosomiasis typically emerge and include fever, rash, swelling of the hands and face, headaches, fatigue, myalgias and arthralgias, pruritis, and lymphadenopathy. As disease progresses, weight loss ensues with progressive confusion, personality changes, daytime sleepiness with nighttime sleep disturbances, and other neurologic signs and symptoms such as paralysis, ataxia, and balance problems. If left untreated, neurologic symptoms will progress until eventually death occurs, usually years after initial infection.
The diagnosis should be considered in any refugee with potential exposure and unexplained signs or symptoms such as weight loss and neurologic decline.
More information on the biology, diagnosis, and treatment of these diseases may be found on the CDC Parasitic diseases website. CDC also offers diagnostic and treatment assistance.
Syphilis
Given the low prevalence of syphilis in the Congolese refugee population (Table 5), screening for syphilis should follow the current CDC domestic refugee medical screening guidelines. That is, providers should rely on the results of the pre-departure testing, if it is available.
Repeat screening should be done domestically with a nontreponemal test (e.g., Venereal Disease Research Laboratory [VDRL] or rapid plasma reagin [RPR]) in the following situations:
- For all refugees ≥15 years old if overseas results are not available.
- For children <15 years old who are at risk (i.e., mother who tests positive for syphilis) should be evaluated according to the Congenital Syphilis section of the CDC Sexually Transmitted Diseases Treatment Guidelines, 2010.
- Any refugee who has a history of sexual assault
Refugees with positive nontreponemal screening test results should have confirmatory treponemal testing.
HIV Infection
HIV testing is offered to refugees by many state health departments. The current domestic refugee screening guidelines for HIV recommend universal screening of refugees after arrival. This is especially important since in January 2010, the requirement for HIV testing of adult refugees prior to US resettlement was removed. The known history of sexual violence in the Congolese refugee population and data that indicate relatively higher rates than most refugee populations reinforce the importance of HIV screening in Congolese refugees.
Chlamydia and Gonorrhea
The current Refugee Domestic Screening Guidelines for Sexually Transmitted Diseases suggest routine screening for chlamydia in women ≤25 years old who are sexually active, or testing refugees for chlamydia and gonorrhea if there are known risk factors or signs of infection.
There are limited data available on rates of chlamydia and gonorrhea in Congolese refugees (Table 5). Given the lack of data and well-documented high rates of sexual violence, it is reasonable to extend screening for chlamydia and gonorrhea to both female and male adult refugees as well as any child with a history of sexual abuse or signs of infection (e.g., leukesterase).
Chronic Viral Hepatitis
The most common chronic viral hepatitis encountered in refugees is hepatitis B. Clinicians should screen all Congolese refugees for chronic infection with hepatitis B virus on arrival to the U.S., as recommended in the CDC Guidance for the U.S. Domestic Medical Examination for Newly Arriving Refugees. Some Congolese refugees may have received one or more doses of hepatitis B vaccine. Hepatitis B surface antibody may be positive if measured after the first or second dose of vaccination and does not necessarily indicate long-term immunity. Congolese refugees generally do not receive the full hepatitis B series prior to migration, with the exception of refugees departing from Kenya (since September 2013). Even if vaccinated, refugees should be screened for hepatitis B infection if previous results are not available since vaccination does not protect a person with precedent infection. If the refugee is not infected with hepatitis B virus, and has not received an acceptable full course of hepatitis B immunization, the vaccine course should be completed according to ACIP guidelines. More information and guidance about hepatitis B infection and prevention in refugees is available in the domestic screening guidance. There are no published or other available screening data on the prevalence of hepatitis C in Congolese refugees and screening guidelines remain consistent with the broader screening guidelines for arriving refugees.
Anemias
Anemia is frequently caused by multiple factors such as nutritional deficiency (e.g., low iron intake), parasitic infections such as hookworm and malaria, thalassemias, and hemoglobinopathies, although it may indicate other underlying diseases (e.g., cancer, ulcers). There will be an expected higher rate of sickle cell anemia (SCA) in Congolese refugees based on available country prevalence data, and physicians may consider screening for SCA, especially in refugees found to have anemia. Screening may lead to appropriate management and monitoring of those with SCA as well as to counseling of those who have sickle cell trait.
In addition, glucose-6-dehydrogenase (G-6-PD) deficiency, an enzyme deficiency, is common in certain populations and has been estimated to occur in 19% of the population of the DRC 17. Unlike most inherited hematologic disorders which result in anemia (e.g., decreased hemoglobin or change in indices such as MCV or RDW), G-6-PD deficiency is not evident on routine blood testing or blood smears. Under certain circumstances, G-6-PD deficiency may result in acute hemolytic anemia, usually after a refugee with this condition is exposed to certain medications, foods, or even infections. Therefore, certain medications with strong oxidizing potential [PDF – 1 page] (e.g., primaquine for malaria, dapsone) should be avoided if the patient’s G-6-PD status is unknown (or the patient should be tested for G-6-PD deficiency before he or she takes the medication). Other common oxidizing medications should also be used with caution or avoided in this population, including sulfa-based medications; unless the patient’s G-6-PD status is known.
Alpha thalassemia should also be considered in patients with an anemia.
Hypertension, Dyslipidemia, and Diabetes
Routine blood pressure screening and monitoring is suggested in newly arriving Congolese refugees, as with all populations. Diabetes should be considered when there are risk factors (e.g., obesity) or other common signs are present (e.g., hyperglycemia on blood chemistry, glucosuria). Lipid screening should be considered according to United States’ guidelines.
Health Information
This section describes the disease burden for specific diseases among the Congolese refugee community. The data sources for this section include the International Organization of Migration (IOM), United Nations High Commissioner for Refugees (UNHCR) Health Information System (HIS), CDC’s Electronic Disease Notification System (EDN), a CDC pilot assessment of Congolese refugees in Rwanda in September 2012, and data from domestic screening exams provided by state health departments.
Communicable Disease
Malaria
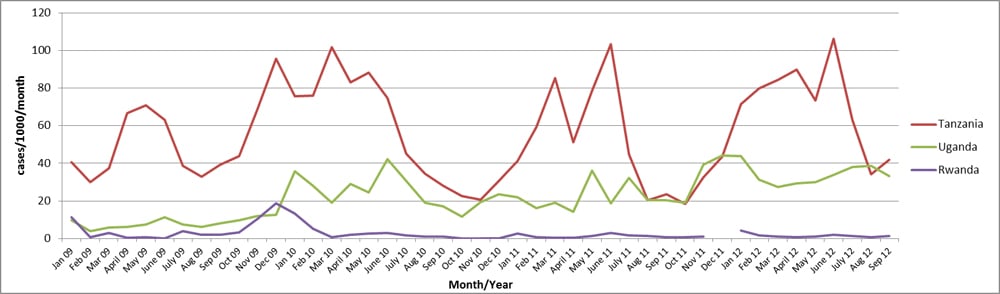
Although malaria is common in DRC, the rate of malaria in refugees will better reflect their country of asylum (Figure 8). Therefore, certain populations will have very low rates of malaria prior to migration, such as the Congolese in Rwanda, where most populations are located in high altitude areas which have no malaria transmission. Conversely, populations originating in Tanzania, Uganda, Burundi, and Zambia are more likely to have had more recent malaria exposure. According to refugee health screening data from health departments in 5 Congolese refugee-receiving states, of the 321 Congolese refugees screened, 4 (1.2%) tested positive for malaria. For more information on malaria screening for Congolese refugees refer to the Health Conditions to Consider in Post-Arrival Medical Screening of Congolese Refugees: Malaria section of this profile.
Figure 8: Incidence rates of confirmed malaria cases in refugee camps in Rwanda, Tanzania, Uganda, and by month, 2009–2012
Parasitic infections
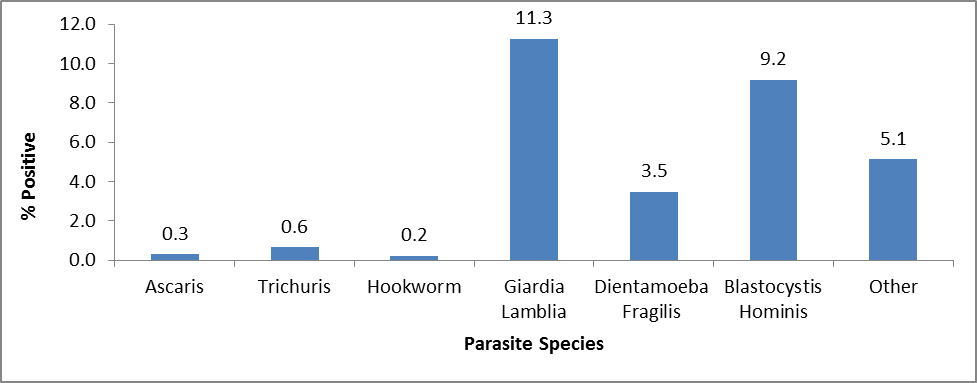
Domestic medical screening data from 4 states have shown a number of parasitic infections that can be diagnosed in Congolese refugees (Figure 9). The following section describes some of the most common parasitic infections among Congolese refugees.
Strongyloidiasis
Strongyloidiasis is a parasitic nematode infection that is common in Congolese refugees and is known to persist for more than 50 years in the human host. Infection is frequently asymptomatic but may lead to morbidity and, when the infected individual is immunosuppressed, even result in death. Unlike most parasites that are unable to replicate in the human host, Strongyloides is able to replicate, causing infection that may persist for decades. If strongyloidiasis is not detected promptly after an infected refugee’s arrival, data indicate that the average time to diagnosis in the United States is more than 5 years after migration 18. Strongyloides hyperinfection syndrome may occur many years after an infected refugee migrates to a non-endemic setting, with case reports occurring >50 years after a refugee’s last known exposure 19, 20, 21. Hyperinfection syndrome, triggered when large numbers of parasites infiltrate internal organs, results in fatality rates exceeding 50%. The syndrome is generally induced when an individual is placed on corticosteroids, although other immunosuppressive conditions (such as cancer and transplant chemotherapeutic immunosuppression) may also trigger it 19, 21. Data from newly arrived Congolese refugees from 1 resettlement state found that 37.5% of 267 specimens tested positive (Figure 12). Testing of specimens for Strongyloides was performed if the refugee was not presumptively treated overseas and if a test was available at the state laboratory. For more information on Strongyloides screening for Congolese refugees, refer to the Health Conditions to Consider in Post-Arrival Medical Screening of Congolese Refugees: Strongyloidiasis section of this profile.
Schistosomiasis
Schistosomiasis, caused by S. hematobium and S. mansoni, is common in DRC populations. In addition, infection may be found in all countries of asylum including Burundi, Rwanda, South Africa, Tanzania, Uganda, and Zambia. Untreated infection generally lasts more than a decade but can persist up to 30 years. Schistosomiasis is associated with liver cirrhosis and resulting clinical complications (S. mansoni, S. japonicum), squamous cell carcinoma of the bladder (S. haematobium), and urinary tract obstruction and renal failure (S. haematobium). Potentially devastating clinical manifestations occasionally occur when the parasite egg enters a refugee’s systemic circulation and travels to a normally sterile site within the body, causing severe inflammation. Eggs may travel to any part of the body, including the brain and spinal cord, where the inflammatory response to the egg may cause paralysis or myelitis. Data obtained from newly arrived Congolese refugees from 2 resettlement states found a 5.6% seroprevalence in 1,279 tested specimens, although not all Congolese refugees were screened for schistosomiasis (Figure 12). Testing of specimens for schistosomiasis was done if the refugee was not presumptively treated overseas. For more information on schistosomiasis presumptive treatment during the Pre-Departure Medical Screening of Congolese refugees refer to the Pre-Departure Medical Screening section of this profile.
Figure 9: Parasites identified by stool ova and parasite examination in Congolese refugees during domestic medical examinations in 4 states from 2010–2013 (n=1,347)
Non-Communicable Disease
Splenomegaly
In early 2014, the International Organization for Migration (IOM) noted high rates of splenomegaly in refugees undergoing screening in Uganda. Cases were reported to be primarily asymptomatic, clustered in families, and exclusively occurring in refugees from Democratic Republic of the Congo (DRC). This clinical finding was particularly common in the Kyangwali, a Resettlement Camp in Uganda, where it was noted that 16% of refugees had splenic enlargement. IOM, with the assistance of the U.S. Centers for Disease Control and Prevention (CDC), began offering additional diagnostic testing and empiric treatment for refugees with palpable splenomegaly during pre-departure medical examinations to better understand the increase in cases. Clinical evaluation is currently taking place to identify with certainty the etiology and to ascertain potential causes such as acute malarial, schistosomiasis, leishmaniasis, hepatic disease (i.e., hepatitis C), and non-infectious etiologies (such as thalassemias).
Although etiology is currently unknown, one potential cause is chronic, repeated infections with malaria (when severe, termed “Hyperreactive Malaria Splenomegaly (HMS) Syndrome”). While the investigation is ongoing, all refugees with positive malaria tests are receiving treatment for acute malaria. In addition, all refugees will be presumptively treated with artemether-lumefantrine (which will treat blood stage malaria parasite) immediately before departure to the United States.
Malaria-associated splenomegaly and HMS are complications of recurrent malaria infections. Although the specific pathophysiology is unknown, evidence suggests that repeated exposure to malaria antigens elicits an exaggerated immune response, excessive IgM production, and eventual splenic deposition that results in splenomegaly. Patients with HMS may not have active signs of malaria or detectable parasite in their blood if tested for malaria (e.g., may have negative blood smears or rapid malaria tests [RDTs]). Symptoms of HMS can be quite variable and may consist solely of abdominal fullness or palpable splenomegaly. However, the degree of splenomegaly, at times, can be severe, reaching lengths of 20 cm and leading to fatal complications, if left unmanaged. Fatal complications include splenic rupture following minor trauma or secondary bacterial infections due to underlying hematological abnormalities (i.e., severe hypersplenism, leukopenia).
All refugees who underwent HMS therapy prior to departure should receive follow-up testing after arriving in the United States. These patients should receive laboratory testing, including repeat IgM testing and repeat ultrasonography. In addition, all refugees who have presumed malaria-associated splenomegaly or HMS should be tested for G6-PD. If the G6-PD is normal, patients should be treated with a 2-week course of primaquine for the potential hepatic phase of non-falciparum malaria. Persons with a large spleen should also be reminded not to participate in physical activities that can cause trauma (i.e., contact sports).
Based on the results of the ongoing investigation, CDC may issue additional recommendations for the monitoring and/or treatment of relocated refugees with HMS. For further information, see CDC guidelines regarding diagnostic testing for malaria, as well as post-arrival guidance on the management of malaria and its complications in refugee populations.
Anemias
As in other refugee populations, anemia in the Congolese is frequently multifactorial. In contrast, however, Congolese are expected to have higher rates of sickle cell disease (SCD) and trait. The DRC, along with Uganda, Cameroon, Gabon, Ghana, and Nigeria, are considered to have the highest overall burden of SCD in Africa 22. The overall prevalence of sickle cell anemia (SCA, including trait and disease) in the DRC is estimated to be between 20–30% 22. In 2010 an estimated 79% (~242,200) of neonates with SCA were born in sub-Saharan Africa, with 2 African countries and 1 Asian country (Nigeria, DRC, and India) representing 57% (~353,500) of the annual number of newborns with SCA globally 22. A significant number of those with SCD and its variants will experience a sickle crisis when they travel to even modest altitudes (>4,400 feet), and this should be considered for those moving to United States cities that are in higher altitudes (e.g., Denver, Salt Lake City) 23. In addition, data from a pilot health assessment conducted in refugee camps in Rwanda in 2012 showed that 5% of refugees had mild, moderate, or severe iron deficiency anemia (unpublished CDC data). Several refugee camps in Rwanda are located at higher elevations (>2,000m); therefore, adjustments for altitude were made by using WHO/CDC criteria for all locations to prevent underestimates of anemia in the Rwanda cohort. Cases of moderate and severe anemia were low (1% and 0.3%, respectively) after hemoglobin values were adjusted for gender, age, and camp elevation. For more information on anemia screening for Congolese refugees, refer to the Congolese Health Conditions to Consider in Post-Arrival Medical Screening of Congolese Refugees: Anemia section of this profile.
Nutrition
Data from a pilot health assessment conducted in Rwanda in 2012 showed a relatively low rate of malnutrition in refugees located in 3 refugee camps, as well as in urban refugees living in Kigali (unpublished CDC data). Of children aged 6–59 months from all Rwanda locations, 5% met the criteria for moderate acute malnutrition. No children in this age group had severe acute malnutrition from any location in Rwanda. Of children aged 5–19 years, 3% met criteria for severe acute malnutrition and 6% met criteria for moderate acute malnutrition. Acute malnutrition as defined by BMI was more prevalent in the camps than among the urban refugee population; however, 55% of adult refugees screened from the urban population were overweight or obese by the same index. Overall, the prevalence of malnutrition among children aged 6–59 months in the Rwanda cohort was lower than rates among other refugee groups resettling from other parts of Africa. Prevalence rates of acute malnutrition (i.e., “wasting”) in children 6–59 months have been as high as 12.3% and 8.2% in certain camp locations in Ethiopia and Kenya, respectively (26). However, since prevalence rates for moderate and severe anemia in the Rwanda cohort were also low (1% and 0.3%, respectively), this suggests a lower risk of overall nutritional deficiencies in this population than in other United States-bound refugee groups. It should be noted that these are Rwanda-specific data only and may not reflect the nutritional status of Congolese refugees resettling from other countries.
Hypertension, Dyslipidemia, and Diabetes
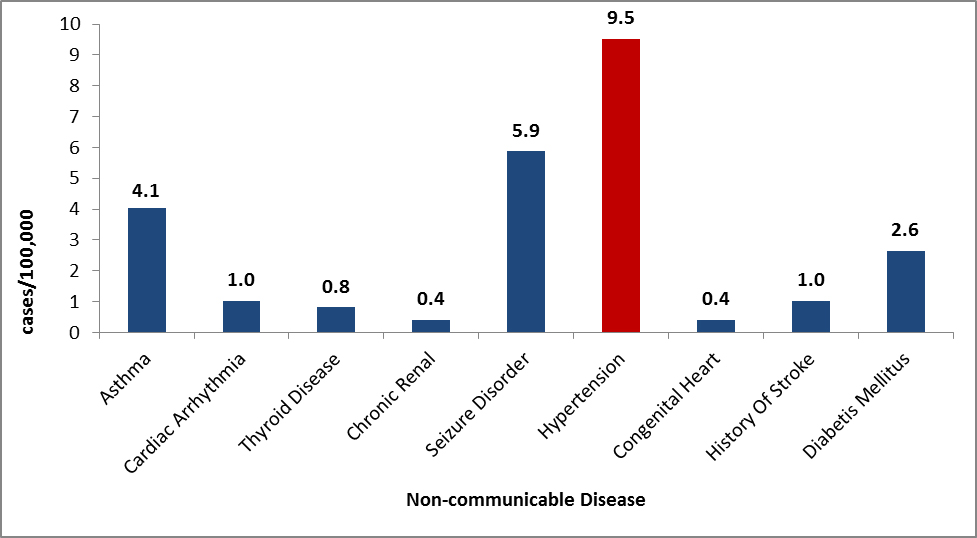
Hypertension, dyslipidemia, and diabetes are disproportionately represented in persons of African descent. Data from Congolese patients indicate that this population follows these trends and has high rates of these disorders (Figure 13) 24, 25.
Figure 13: Non-communicable diseases as reported by Congolese refugees during overseas medical examinations at panel physician sites, 2008–2012 (N=4,938)
Mental Health
Mental health conditions in refugee populations can develop or become exacerbated due to issues related to acculturation and limited coping mechanisms upon resettlement. Among the 3,577 Congolese refugees examined by IOM physicians in the overseas medical screening exam from 2010–2012, 1% were found to have a mental health condition. Data in Table 2 demonstrate the most common mental health conditions found among Congolese refugees. These were mental retardation (0.39%); adjustment disorders (0.34%); schizophrenia (0.11%); mental disorder, not otherwise specified (0.08%); depression (0.06%); and specific developmental disorder of motor function (0.6%). Mental retardation includes cases ranging from mild to moderate and unspecified mental retardation. Depression includes mild, moderate, and severe episodes of depression without psychotic symptoms. The mental health component of the overseas medical screening exam is subject to limitations in the refugee setting including lack of medical history, language limitations, cultural barriers, and a lack of mental health specialists.
Table 2: Top disease conditions (ICD-10) under mental health disease group among Congolese refugees (n=3,577) screened in Burundi, Rwanda, Uganda, and Kenya, 2010–2012
| ICD-10 disease condition under mental health disease group | No. of People | Prevalence (%) |
|---|---|---|
| Mental retardation | 13 | 0.39% |
| Reaction to severe stress and adjustment disorders | 11 | 0.34% |
| Schizophrenia | 4 | 0.11% |
| Mental disorder, not otherwise specified | 3 | 0.8% |
| Depression | 2 | 0.6% |
| Specific developmental disorder of motor function | 2 | 0.6% |
| Total | 35 | 1.03% |
Source: IOM
Although IOM data indicated low rates for some mental health disorders, other assessments have shown high rates of post-traumatic stress disorder (PTSD) among this population. The high rates of PTSD are due to the severe and widespread nature of personal violence and trauma Congolese refugees are reported to have witnessed and experienced, including Sexual Gender Based Violence. A population-based study conducted in the eastern DRC identified 41% of the adult population that met the symptom criteria for major depressive disorder (MDD), and 50% for PTSD. After extrapolation to the sampling frame population of the DRC, it is estimated that 3.25 million adults meet criteria for PTSD, 2.63 million meet criteria for MDD, and approximately 1.04 million have attempted suicide 9.
A recent report surveying 43 local resettlement agencies serving Congolese refugees after their arrival in the United States suggested a high degree of mental health issues, including depression, anxiety disorder, substance abuse, and domestic violence 11. This report also identified at least 2 challenges in terms of increasing access to mental health services in the US for Congolese: (a) interpretation needs and (b) client’s refusal of services. However, in a controlled trial of psychotherapy among Congolese survivors of sexual violence randomly assigned to either group therapy or individual support, group psychotherapy was found to be more effective at reducing PTSD symptoms, combined depression and anxiety symptoms, and improving functioning 27. This suggests that while mental health is a sensitive subject for Congolese, in settings where trust has been built between patient and caregiver, open discussion of mental health problems may be more readily achieved.