Central American (Guatemalan, Honduran, Salvadoran) Minor Refugees
Priority Health Conditions
A list of priority health conditions to consider when caring for or assisting Central American refugees.
Background
Geography, History and Cultural Origins, Ethnic Groups, Language and Literacy, Religious Beliefs, Family and Kinship
Healthcare Access and Conditions in Guatemala, Honduras, and El Salvador
Primary Healthcare, Immunizations, Reproductive Health, Women’s Health Issues, Sexual-and Gender-Based Violence.
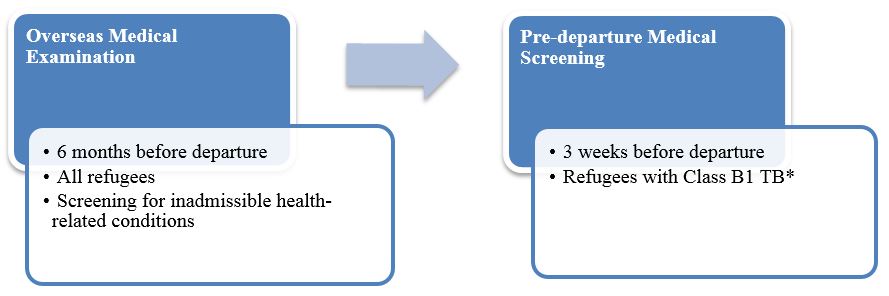
Medical Screening of US-Bound Refugees
Overseas Medical Examination, Pre-Departure Medical Screening, Post-Arrival Medical Screening
Health Information
Infectious and Communicable Diseases, Parasitic Infections, Non-Communicable Diseases, Mental Health, Nutrition
Priority Health Conditions
Healthcare providers should consider the following conditions when caring for refugees from El Salvador, Guatemala, and Honduras:
Background
Geography
El Salvador, Guatemala, and Honduras are three of the northernmost countries of Central America, making up the Northern Triangle, situated just south of Mexico on the isthmus linking North and South America [1]. The Northern Triangle has a population of more than 33.2 million. Guatemala is the most populous country, having a population of approximately 17.4 million [2], while El Salvador and Honduras have populations of roughly 6.5 million and 9.3 million, respectively [3, 4]. Each country is mountainous and has narrow coastal belts along the Pacific Ocean and/or the Caribbean Sea [2-4]. The region is vulnerable to hurricanes, active volcanoes, and earthquakes [1].
Figure 1: Location of El Salvador, Guatemala, and Honduras

Source: Division of Global Migration and Quarantine (DGMQ), CDC
History and Cultural Origins
Like other Mesoamericans, Guatemalans, Hondurans, and Salvadorans share a common pre-Columbian history, originating from the Lenca, Olmec, and Maya civilizations. These ancient indigenous cultures left behind an extensive legacy of art, architecture, and traditions, many of which are still present throughout Central America. Indigenous Central Americans first came into contact with Spanish explorers and colonists in the early 1500s and endured three centuries of colonial rule. In 1821, a united battle for independence led to the establishment of the Federal Republic of Central America. The republic dissolved in 1838, and the countries of El Salvador, Guatemala, and Honduras were formed [1]. However, post-colonial independence brought instability, violence, and war, which persisted throughout the 20th century along with shifting civil and military governance, uneven economic development, and social unrest [1].
Ethnic Groups
El Salvador
Approximately 86.3% of Salvadorans are mestizo (mixed race). Whites account for 12.7%, while Amerindian (including Lenca, Kakawira, and Nahua-Pipil), black, and other ethnicities account for a small minority [3].
Guatemala
Roughly 60% of Guatemalans are of mestizo or European descent. The remaining 40% of the population is K’iche (9.1%), Kaqchikel (8.4%), Mam (7.9%), Q’egchi (6.3%), other Mayan (8.6%), and indigenous non-Mayan (0.2%) [2].
Honduras
Mestizos account for approximately 90% of the population, while Amerindians represent 7% of Hondurans. The remaining 3% of the population is either black or white [4].
Language and Literacy
El Salvador
Spanish is the official and most widely spoken language in El Salvador [3]. Some indigenous Salvadorans speak Nahua, an Amerindian language. However, such speakers are few, as indigenous persons account for less than 1% of El Salvador’s population [3]. Approximately 88% of the Salvadoran population is literate, defined as being at least 15 years old and able to read and write. Among Salvadoran men, 90.4% are literate, while literacy for women is estimated at 86% [3].
Guatemala
Although Spanish is the official language of Guatemala, only 60% of the population communicates primarily in Spanish. Forty percent communicate in one of many Amerindian languages. There are 23 officially recognized Amerindian languages, including Quiche, Cakchiquel, Kekchi, Mam, Garifuna, and Xinca [2]. Approximately 81.5% of the Guatemalan population is literate. Overall, 87.4% of men are literate, and 76.3% of women [2].
Honduras
The official language of Honduras is Spanish, which is widely spoken. Hondurans may also speak Amerindian dialects [4]. Approximately 88.5% of the Honduran population is literate. Rates of literacy among men and women are comparable: 88.4% of male Hondurans and 88.6% of female Hondurans are literate [4].
Religious Beliefs
El Salvador
El Salvador is overwhelmingly Christian. Roman Catholicism is practiced by 57.1% of the population. Protestants account for 21.2% of the population, while small minorities are Jehovah’s Witnesses (1.9%) or Mormon (0.7%). Additionally, 16.8% of the population does not identify as religious, and the remaining 2.3% practice other religions [3].
Guatemala
Roman Catholicism is the predominant religion in Guatemala, with 65%-70% of Guatemalans identifying as Catholic [5]. However, among the indigenous Maya, Catholic practices and traditions are often infused with beliefs of pre-Columbian origin. Evangelical Protestantism has become increasingly popular since the mid-20th century, particularly among lower-income households. As a result, Protestants now account for about 40% of the population [6].
Honduras
Roughly 80% of the Honduran population is Roman Catholic. Growth in Protestant churches has swelled in recent years, making Protestantism the second most popular religion in Honduras [7].
Family and Kinship
Familismo is an integral part of Latin American culture, in which women play a critical role. Women are often responsible for the organization and maintenance of family life and tradition, a role that may afford them significant influence in the home. Many Central American nations are patriarchal, with men often providing the primary income for the family, and women serving as caregivers for the children and family [8].
For additional information regarding minors from Central America, please visit the Cultural Orientation Resource Exchange [PDF – 16 pages].
Population Movements
Drivers of Immigration
Historically, the primary drivers of immigration from El Salvador, Guatemala, and Honduras to the United States have been family reunification and the economy; however, civil war throughout the region in the 1980s also prompted immigration. Recently, extreme poverty and increasing violence have spurred a new wave of immigration [1].
Increased instability and growing gang violence have been particularly unsettling for families and have pushed many children, often unaccompanied by an adult, to flee to the United States. The numbers of unaccompanied minors who arrived in the United States from El Salvador, Guatemala, and Honduras significantly increased from fiscal year (FY) 2009 to 2020 (Figure 2). Furthermore, US Border Patrol reported record numbers of children from Guatemala and Honduras in FY 2019, as well as increases in children from El Salvador and Mexico compared to FY 2018. From October 2020 through February 2021, nearly 30,000 unaccompanied children arrived at the southwest border, 2,942 of whom were 12 years of age and under [9]. In March 2021, 18,890 unaccompanied children apprehended at the Southwest border, a 100% increase from the previous month [10].
Figure 2: Unaccompanied Minors Encountered by US Customs and Border Protection at the Southwest Border, Fiscal Year 2009-2020
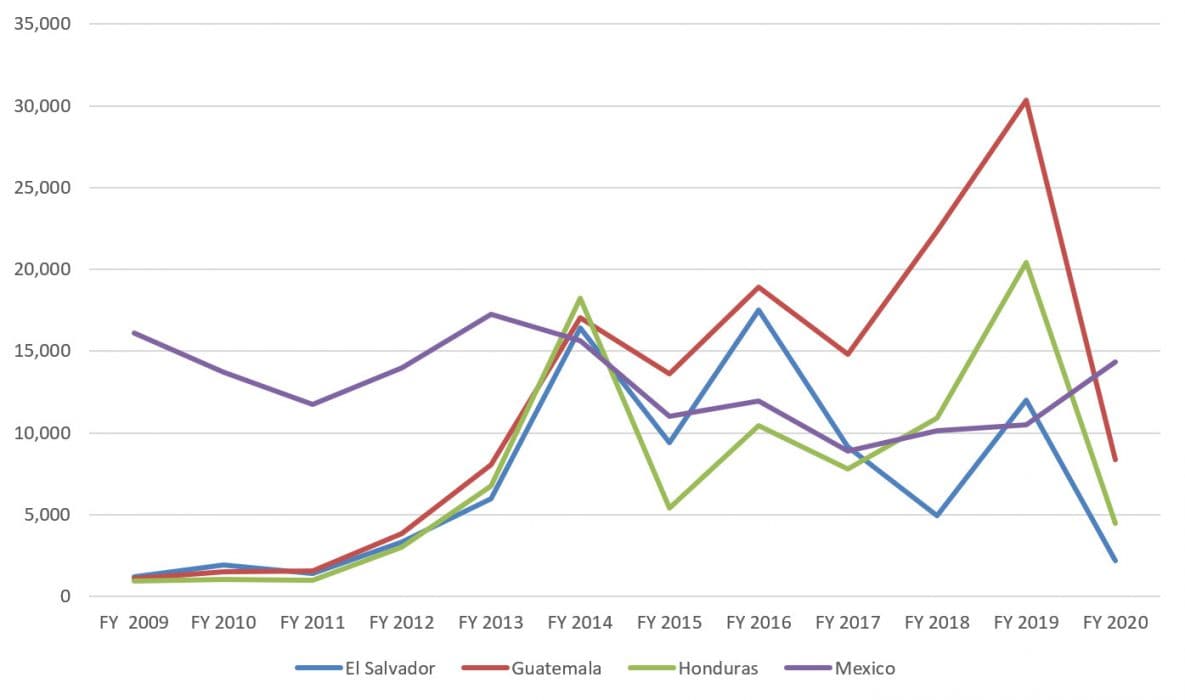
Source: US Customs and Border Protection. https://www.cbp.gov/newsroom/stats/southwest-land-border-encounters/usbp-sw-border-apprehensions
The Department of Homeland Security (DHS) reports that unaccompanied minors presenting at border stations have health issues, often associated with the difficult journey or crowded, unsanitary, and environmental conditions experienced prior to arrival in the United States. The majority of health conditions reported at border stations include scabies, lice, rash illness, diarrhea, and respiratory infections [11].
The Central American Minors Program
Jointly established by the US Department of State Bureau of Population, Refugees, and Migration (PRM) and the Department of Homeland Security (DHS) US Citizenship and Immigration Services (USCIS), from December 2014 until January 2018, the Central American Minors (CAM) Program provided certain minors in El Salvador, Guatemala, and Honduras the opportunity to be considered, while still in their home country, for refugee resettlement in the United States. Those determined ineligible for refugee status were considered for the possibility of admission to the United States under parole. In November 2017, due to a policy change, the Department of State stopped accepting new applications for CAM Program, and USCIS ceased interviewing CAM cases in January 2018.
On March 10, 2021, the US Department of State announced that the United States would restart the CAM Program in a two-phase process to provide lawful pathways for protection in the United States. Phase One began to reopen and process previously closed cases, while Phase Two will accept new applications for processing beginning in summer 2021. During the first iteration of CAM and the first phase of its reopening, to access the program, children and their parents were subject to the following requirements:
A qualifying parent must be:
- A national of El Salvador, Guatemala, or Honduras
- At least 18 years of age
- Lawfully present in the United States (legal permanent resident status; temporary protected status; parole; deferred action; deferred enforced departure; withholding of removal)
A qualifying child must be:
- The child (biological, stepchild, or legally adopted) of the qualifying parent
- Unmarried
- Under 21 years of age
- A Guatemalan, Honduran, or Salvadoran national living in his or her country of nationality
Additional information regarding the CAM program can be found on the PRM and USCIS webpages. Additional information on how children may qualify for humanitarian parole through the CAM program is also available on the USCIS page.
Refugee and Parole Status
The 1951 Convention Relating to the Status of Refugees defined a refugee as a person who, “owing to a well-founded fear of being persecuted for reasons of race, religion, nationality, membership of a particular social group, or political opinion, is outside the country of their nationality, and is unable or, owing to such fear, unwilling to avail himself of the protection of that country” [12]. Additional information on international refugee status can be found here. For the US legal definition of a refugee please refer to Section 101(a)(42) of the Immigration and Nationality Act [PDF – 1 page]. In contrast, parole status allows an individual who may otherwise be inadmissible or ineligible for admission to the United States to enter the United States for a specified period of time [13]. For additional information on parole status, please refer to the USCIS website. If granted refugee status through the CAM program, individuals have access to federal benefits through the Department of Health and Human Services Office of Refugee Resettlement, including health insurance coverage through Refugee Medical Assistance (RMA) or Medicaid. Those who are paroled into the United States are not eligible to receive benefits.
Healthcare Access and Conditions in El Salvador, Guatemala, and Honduras
Even though minors from El Salvador, Guatemala, and Honduras may be designated as refugees, they have not been living in refugee camps (there are no refugee camps in Central America), and usually come from their hometown or village.
Primary Care
Compared to the United States and other high-income nations, physician density in El Salvador, Guatemala, and Honduras is quite low. According to recent data, there are approximately 1.6 physicians per 1,000 population in El Salvador. Physician population density is markedly lower in both Guatemala and Honduras, with 0.93 and 0.37 physicians per 1,000 population, respectively [14]. The World Health Organization estimates that countries with fewer than 23 healthcare workers (including physicians, nurses, and midwives) per 10,000 population will likely fail to achieve adequate coverage rates for primary healthcare, as defined by the Millennium Development goals [15]. Therefore, the number of doctors in El Salvador, Guatemala, and Honduras is likely insufficient to achieve adequate coverage for primary healthcare needs.
Access to basic healthcare in Central America largely depends on socioeconomic status and environment (urban or rural). El Salvador, Guatemala, and Honduras have worked to improve access and quality of care, particularly in rural settings. Despite improvements to health services and systems, rural populations still have difficulty accessing basic health services. In Guatemala, it is estimated that basic health and nutrition services meet only 54% of the needs of the rural population [16]. Similarly, in Honduras, 88.3% of the total population receives care from the Ministry of Health. However, the majority of health services are located in the most developed cities, not easily accessible for rural and indigenous populations [17]. Minors from rural and often underserved regions may also seek care from traditional healers, such as curanderos or folk healers [18]. Curanderismo exists throughout Latin America, and practitioners treat a wide range of ailments including illnesses recognized by modern medicine as well as “folk illness” specific to the local population [18].
Immunizations
Despite challenges in accessing basic primary care services in El Salvador, Guatemala, and Honduras, each country reports high immunization coverage among children. Vaccination coverage in El Salvador varies from 90% to 93%, depending on the vaccine, while vaccination coverage ranges from 93% to 98% and 88% to 93% in Guatemala and Honduras, respectively [19]. El Salvador, Guatemala, and Honduras administer vaccines in accordance with the World Health Organization (WHO) Expanded Program on Immunization.
Women’s Health Issues
Select reproductive health indicators for El Salvador, Guatemala, and Honduras are presented in Table 1. In many cases, access to reproductive healthcare is likely limited for indigenous populations throughout Central America.
Table 1. Reproductive Health Indicators for El Salvador, Guatemala, and Honduras
| Country | Prevalence of contraceptive use (%) | Fertility rate# | Adolescent fertility rate† | Infant mortality rate‡ | Maternal mortality ratio§ | Prevalence of pregnant women receiving prenatal care (%)ǁ | Births attended by skilled birthing attendant (%) |
|---|---|---|---|---|---|---|---|
| El Salvador | 72 | 1.9 | 66 | 14 | 54 | 96 | 98 |
| Guatemala | 54* | 3.2 | 81 | 24 | 88 | 93* | 63 |
| Honduras | 73 | 2.4 | 66 | 17 | 129 | 97 | 83 |
#Total fertility rate represents the average number of children born to a woman during her childbearing years
†Number of births per 1,000 women ages 15-19
‡Number of infant deaths per 1,000 live births
§Number of maternal deaths per 100,000 live births
ǁPercentage of all pregnant women receiving prenatal care at least once during pregnancy by skilled health personnel
Source: World Bank HealthStats Databank [20], unless otherwise cited.
*UNICEF [21]
Sexual- and Gender-Based Violence
Sexual- and gender-based violence has been increasing throughout Central America and Mexico. El Salvador, Guatemala, and Honduras report extremely high rates of femicide, with rates up to five times higher than overall homicide rates in the majority of Northern, Western, and Southern European countries [22]. Gangs and other armed criminal groups often perpetrate violence against women, and domestic violence throughout Central America is widespread [23]. In Honduras, 16,000 allegations of violence against women were registered in 2012, with 74% relating to domestic or interfamily violence, and 20% relating to sex crimes [24].
Medical Screening of US-Bound Refugees
Overseas Medical Examination
An overseas medical examination is mandatory for all refugees identified for resettlement to the United States and must be performed in accordance with CDC Technical Instructions. The overseas medical examination is performed by panel physicians selected by the US Department of State. CDC provides the regulatory and technical oversight and training for all panel physicians. The purpose of the medical examination is to identify applicants with inadmissible health-related conditions.
Central American refugees and parolees admitted through the CAM program receive medical assessments from panel physicians before arrival in the United States (Figure 3). As this program is relatively new, additional components of the medical screening may be added as more individuals are approved for resettlement. Those entering under different mechanisms do not receive medical assessments by panel physicians before entry.
Information collected during the overseas medical examination is reported to the Electronic Disease Notification system (EDN) and is available to state refugee health programs in the states where the refugees are resettled. Refugees are not required to receive any vaccines before they are admitted into the United States.
* Class B1 TB refers to tuberculosis fully treated by directly observed therapy, or abnormal chest x-ray with negative sputum smears and cultures, or extrapulmonary TB.
Pre-departure Medical Screening
If previously diagnosed with Class B1 TB (tuberculosis fully treated using directly observed therapy, or abnormal chest x-ray with negative sputum smears and cultures, or extrapulmonary TB), Central American refugees receive a pre-departure medical screening approximately 3 weeks before leaving for the United States.
Post-arrival Medical Screening
CDC recommends that refugees receive a post-arrival medical screening (domestic medical examination) within 30 days of arrival in the United States. The Department of Health and Human Services Office of Refugee Resettlement (ORR) supports medical screening for those who have been granted refugee status.
The purpose of these comprehensive examinations is to identify conditions for which refugees may not have been screened during their overseas medical examinations and to introduce refugees to the US healthcare system. CDC provides guidelines and recommendations for the domestic medical examination of newly arrived refugees, which state health departments oversee and administer. State refugee health programs determine who conducts the examinations within their jurisdictions; these may be performed by health department personnel, private physicians, or federally qualified health centers (FQHCs). Most state health departments collect data from the screenings.
Health Information
Tension, fear, and uncertainty that can be triggered by chronic violence have lasting effects on physical and psychological health. Chronic distress, mental health conditions, hypertension, and depressed immune system can all stem from exposure to protracted violence [25]. Additionally, fear and concerns regarding crime often deter people from using healthcare and other critical services, which are largely concentrated in urban areas and difficult to access for rural populations [16, 26].
This section describes health conditions, with a focus on infectious diseases, for which children from El Salvador, Guatemala, and Honduras are at significant risk. Where applicable and available, screening or pre-departure interventions are described.
The American Academy of Pediatrics (AAP) Immigrant Toolkit Section on Clinical Care reviews diseases and conditions that are prevalent in immigrant populations. The AAP Immigrant Toolkit also provides medical screening and treatment recommendations for immigrants and refugees from resource-poor areas of developing countries, including countries in Central America [27]. For more information please see AAP.
Infectious and Communicable Diseases
Arboviruses: Dengue, Chikungunya, and Zika Viruses
Dengue, chikungunya, and Zika viruses cause mosquito-borne infections of increasing concern in El Salvador, Guatemala, and Honduras. Dengue fever is endemic throughout much of Central and South America. However, chikungunya first arrived in this region in 2014 after appearing in the Caribbean in 2013. Currently, local chikungunya transmission is occurring in more than 45 countries and territories in the Americas, including El Salvador, Guatemala, and Honduras [28, 29]. Active Zika virus transmission has been reported throughout Central America, including El Salvador, Guatemala, and Honduras [30].
Acute dengue, chikungunya, and Zika infections have similar presentations and may be clinically indistinguishable. Common symptoms include fever, headache, severe myalgia, arthralgia, joint swelling, and rash. Chikungunya is unique in that it may cause persistent joint inflammation for months and sometimes years, even after acute symptoms have resolved. Chikungunya should be considered in those with chronic rheumatologic symptoms from areas of local transmission. Dengue is unique because reinfection with another dengue virus can cause a condition called severe dengue. Severe dengue can be fatal if not properly treated in a timely manner. With good medical management, mortality due to severe dengue can be less than 1%. Severe dengue is more likely when an individual returns to a disease-endemic area and unlikely in a newly arriving refugee. Zika may be associated with conjunctivitis and other symptoms that are generally less severe than dengue and chikungunya. Zika virus infection is frequently asymptomatic. Despite the relatively benign nature of acute infection, Zika has recently been associated with an increased risk of Guillain-Barré syndrome, and birth defects (e.g., microcephaly) when acquired during pregnancy [31, 32]. CDC has posted interim screening guidelines for infants with microcephaly and possible Zika infection. Clinical presentation of these infections during the domestic screening visit is unlikely since the incubation period is generally short, with symptoms often resolving within 10 days of exposure.
Hepatitis B Virus Infection
The prevalence of chronic hepatitis B virus infection in Central American children arriving in the United States is unknown. However, recent data suggest that the general prevalence in El Salvador, Honduras, and Guatemala is low (<2%). In addition, all three countries include a birth dose of hepatitis B vaccine in their national immunization schedules. Therefore, it is reasonable to conduct targeted screening for chronic hepatitis B virus infection in at-risk individuals including:
- Known or suspected IV drug users
- Men who have sex with men
- People with tattoos
- Pregnant women
- Children of mothers with known hepatitis B virus infection
- Household contacts of infected individuals
- Individuals infected with HIV or hepatitis C
- Children who received whole blood products or blood components before immigration
- Children with a history of known or possible sexual exploitation
Children should complete the 3-dose hepatitis B vaccine series if no official documentation of prior completion is available.
For further information, see the domestic hepatitis B screening guidance for refugees.
Sexually Transmitted Infections
HIV screening is not required for refugees before resettlement to the United States. However, HIV screening should be offered to all refugees in accordance with existing domestic refugee screening guidelines for HIV developed by CDC. Although HIV prevalence is relatively low in Central America, minors arriving from El Salvador, Guatemala, and Honduras should be screened, as maternal HIV status is likely unknown and vertical transmission is possible. No data are available regarding the prevalence of syphilis, gonorrhea, and chlamydia. Syphilis and gonorrhea screening is done per current CDC Technical Instructions on all refugees 15 years or older. However, any patient, regardless of age, should be tested for syphilis, gonorrhea, or chlamydia if symptomatic or if there is a history of or concern about possible sexual activity or exploitation. Of note, syphilis during pregnancy is an urgent situation requiring immediate management and treatment to reduce the risk of pregnancy loss or congenital syphilis in infants. Refer to the National Center for HIV, Viral Hepatitis, STD, and TB Prevention for additional information.
Tuberculosis
El Salvador reported 2,206 new and relapsed cases of tuberculosis in 2014 and a prevalence of 49 cases per 100,000 population [33]. Within El Salvador, six new cases of multidrug-resistant (MDR) tuberculosis were confirmed in 2014 [33]. Guatemala and Honduras both reported higher numbers of cases and prevalence rates than El Salvador. Guatemala and Honduras reported 3,163 and 2,820 new and relapsed cases, respectively [34, 35]. Tuberculosis prevalence was 106 per 100,000 population in Guatemala, and 49 per 100,000 population in Honduras in 2014 [34, 35]. Additionally, 79 new cases of MDR TB were reported in Guatemala and 38 new cases of MDR TB were reported in Honduras for 2014 [34, 35].
Refugee children are screened for TB infection. Any child with known latent tuberculosis infection (LTBI) at the time of arrival should be offered LTBI treatment. In addition, those without documentation of LTBI screening should be tested, with treatment offered to those who test positive.
For additional information regarding tuberculosis, see the World Health Organization Tuberculosis Profile.
Parasitic Infections
Chagas Disease
El Salvador, Guatemala, and Honduras are all endemic for Chagas disease. There were 90,222 (El Salvador), 166,667 (Guatemala), and 73,333 (Honduras) cases of Chagas disease reported in 2015 [36]. Chagas disease is caused by the parasite Trypanosoma cruzi and is most commonly transmitted through contact with the feces of an infected triatomine insect (“kissing bug”). Chagas disease can also be transmitted congenitally. Reports of blood transfusion and organ transplantation transmission as well as infection after consumption of contaminated food and drink, although rare, have also been documented.
Chagas disease has an acute and chronic phase. Acute infection may be asymptomatic or may be characterized by nonspecific symptoms such as malaise, fever, and anorexia. Swelling may be observed around the site where the parasite entered the body. If left untreated, infection becomes chronic and is lifelong. Severe complications can develop in 20-30% of patients after years to decades of chronic infection. Severe complications most often include heart manifestations such as rhythm abnormalities, stroke, sudden death, and heart failure. Less common severe complications include dilated esophagus or colon. Chronic Chagas disease is considered to be the most common cause of nonischemic heart disease in Central America and may cause cardiomyopathy years after initial infection [37]. However, the majority of people will be asymptomatic and unaware of infection. Of note, there is a risk for mother-to-child transmission during pregnancy, and it is estimated transmission occurs in up to 5% of pregnant women who are infected. Most infants born with congenital Chagas disease have mild or no signs of illness. Additional information on congenital Chagas disease, refer to the Center for Global Health, Division of Parasitic Diseases and Malaria. Children from El Salvador, Guatemala or Honduras should be tested for Chagas disease (see Recommendations for Screening and Diagnosis of Chagas Disease in the United States).
Giardiasis
Giardiasis is a common infection in all refugee populations. Routine screening of asymptomatic individuals is not recommended, as there is no evidence that screening and treatment are beneficial in these cases. However, giardia infection can be associated with mild symptoms such as abdominal discomfort, loose stools, flatulence, and eructation. In addition, it has been associated with failure to thrive in children. As young children may not verbalize symptoms or express overt signs of the disease, it is reasonable to screen children, particularly those under 5 years old. When screening is performed, stool antigen testing is the preferred method, as it is more sensitive and convenient than stool ova and parasite examination.
Malaria
Although malaria is endemic to Guatemala and Honduras (El Salvador was certified malaria free in February 2021, however, refugees may travel through malaria-endemic areas to reach the United States), the prevalence is not high enough to justify routine screening or presumptive treatment. The malaria species predominantly found in these countries is Plasmodium vivax, also known as relapsing malaria. This form of malaria may become dormant in the liver and reactivate months and even years after exposure, causing clinical disease. As such, clinicians should consider malaria in the differential diagnosis with a patient with symptoms associated with malaria, such as fever, even if exposure to malaria was not recent. Refer to the CDC’s Malaria—Diagnosis & Treatment Guidance for further information.
Soil-transmitted Helminths
People living in extreme poverty, including rural and indigenous populations in El Salvador, Guatemala, and Honduras, are at high risk for neglected tropical diseases, including STH (mainly ascariasis, trichuriasis, and hookworm) [38]. Children from El Salvador, Guatemala, and Honduras require periodic deworming campaigns due to significant STH endemicity, with 1.4 million, 5.0 million, and 2.2 million children treated in El Salvador, Guatemala, and Honduras in 2019, respectively [39]. However, STH surveillance data in Central America is limited [40].
Children from El Salvador, Guatemala, and Honduras do not receive presumptive STH treatment before departure. Upon arrival in the United States, these children should be presumptively treated with albendazole, or tested and then treated. It is necessary to check three ova and parasite stool samples collected 12-24 hours apart in order to identify STH infection and treat appropriately.
Strongyloides stercoralis
Available data on Strongyloides prevalence in Central America are limited. Similarly, no data are available on the prevalence of Strongyloides infections in US immigrants and refugees from Central America [41]. It is prudent to presumptively treat or screen for Strongyloides according to current CDC guidelines.
Taeniasis
Taeniasis in humans, caused by Taenia solium (pork tapeworm) and Taenia saginata (beef tapeworm), is endemic in Central America; however, surveillance data is limited [42, 43]. Infections are spread by ingestion of undercooked beef or pork, or ingestion of cysts directly via oral-fecal contamination. Most infections are asymptomatic; however, some patients may have nausea, anorexia, or epigastric pain. Taenia solium is the cause of cysticercosis and neurocysticercosis [44]. In a 2011 house-to-house survey in rural Honduras, neurocysticercosis was the leading cause of seizures, accounting for 13% of cases [45].
Hymenelopis nana tapeworm infection is endemic in Guatemala and is presumed to be present in other Central American countries [46]. Additionally, Hymenelopis nana is the most common tapeworm infection in children living in poverty worldwide. Although infection is often asymptomatic, it may cause abdominal pain and diarrhea. Hymenelopis nana is spread via oral-fecal contamination, and infection is most common in children [47].
Tapeworm infection is diagnosed using stool ova and parasite testing. Testing three stool samples collected 12-24 hours apart increases sensitivity. Tapeworm is treated with praziquantel, with the type of tapeworm dictating the dosage and duration of treatment [48]. However, if seizures or neurologic deficits of unknown cause are present, neurocysticercosis must be ruled out using neuroimaging before treatment with praziquantel.
All Central American children should have a complete blood count (CBC) with differential to evaluate for eosinophilia (absolute eosinophil count ≥400). The differential diagnosis for an increased eosinophil count is broad and should include parasitic infections for this population. It should be noted that not all parasitic infections cause eosinophilia and not all eosinophilia is cause by parasitic infections. Please refer to CDC guidelines for presumptive treatment options or further evaluation, as clinically indicated.
Neurocysticercosis infection can cause seizures and neurologic deficits. Treatment of a person with neurocysticercosis with albendazole and praziquantel can cause adverse effects such as provoking or worsening seizures. Therefore, any child with a known history of neurologic deficit or seizures should not receive albendazole or praziquantel until neurocysticercosis infection has been ruled out or should be done in consultation with an infectious disease expert.
Non-communicable Diseases
El Salvador, Guatemala, and Honduras do not maintain national non-communicable disease registries. However, over the past 25 years, chronic illnesses such as cardiovascular disease, cancer, type 2 diabetes, and chronic respiratory diseases have replaced communicable diseases as the most common causes of death. Rates of adult obesity, hypertension, and tobacco use are similar in all three countries. Communicable diseases continue to be the primary cause of mortality for children under 5 years old. Neonatal and maternal mortality are high, with elevated teen pregnancy rates and lack of prenatal and perinatal care as likely contributing factors. Deaths related to road traffic accidents and violence have noticeably increased in recent years [49–52].
Anemia
Anemia is common in El Salvador, Guatemala, and Honduras. The prevalence in children under 5 years old is 30%, 47%, and 40%, respectively, in these countries [53–55]. Pregnant women also have been noted to have high prevalence of anemia, particularly in Guatemala, where 22% of pregnant women are anemic [56, 57]. Iron deficiency due to poor nutrition or chronic parasitic infection (which can cause indolent blood loss) is the chief etiology of anemia. However, many other conditions may contribute to anemia, such as lead exposure, untreated chronic disease, and hemoglobinopathies. Arriving children should be screened for anemia with a CBC. Please see the CDC Summary Checklist for the Domestic Medical Examination for Newly Arriving Refugees for further guidance
Dental Caries
It should be presumed that most children have had little, if any, dental care, preventive or otherwise, before arrival in the United States. Preventive fluoride varnish should be applied in all children from first tooth eruption through 5 years of age (up to four applications per year, depending on state guidelines) [58]. Children should be referred for dental care as soon as possible after arrival [59].
Developmental Delays
Access to medical care in Central America is often limited [60], and studies show a lag in diagnosis of developmental delays among non-English speaking children in the United States [61]. It is important that children receive appropriate developmental screening at recommended intervals using screening tools that have been validated in Spanish-speaking populations [62]. If delays are identified, children should be referred for home-based or school-based early intervention services.
All children should have age-appropriate vision (ages 3 years and over) and hearing (ages 4 years and over—and at any age if the child is noted to have speech or developmental delays) screens to rule out deficits that could significantly impact development and learning [63].
El Salvador, Guatemala, and Honduras do not have national newborn screening programs for life-threatening, treatable medical conditions. US providers should follow state-specific guidelines for newborn screening in immigrant and refugee infants [64]. If no state-specific guidelines exist, newborn metabolic screening should be considered for infants <6 months of age. For children between 6 months and 3 years old, thyroid function testing is reasonable.
Lead Exposure
Lead poisoning has been reported among children in Central America as a result of exposure to home remedies, lead-glazed ceramics, and industrial contamination [65]. A study in 337 Honduran school-aged children (median age 7.2 years) evaluated blood lead levels. Of these, 19.6% had elevated blood lead levels (>5 ug/dl) [66]. Additionally, in one El Salvadoran city where lead acid car batteries are manufactured and disposed of, thousands of residents, both children and adults, were chronically exposed to lead [67]. Of note, anemia and malnutrition, both common among children in Central America, increase lead absorption.
All infants and children (6 months to 16 years old), as well as pregnant and lactating women and teens, should be screened for elevated lead levels. Elevated lead in pregnant women increases the risk for spontaneous abortion, low birth weight in infants, and developmental delays in infants with significant exposures in utero [68]. Please see CDC Childhood Lead Poisoning Prevention and Domestic Screening Guidance for Newly Arrived Refugees for guidance pertaining to lead poisoning prevention among newly arrived refugee children and additional information.
Mental Health
It can be assumed that the vast majority of children arriving through the CAM program will have experienced some form of significant trauma. These children come from Central American countries with homicide rates ranking among the top five worldwide, high poverty rates, and widespread gang violence. Violence toward women, often perpetuated by gangs and armed criminal groups, has been widely documented. In a 2013 United Nations study, 400 unaccompanied children from El Salvador, Guatemala, Honduras, and Mexico were interviewed. When asked why they had decided to migrate to the United States alone, nearly half (48%) said they left their home country due to escalating violence. Additionally, 81% cited family or opportunities available, 21% reported abuse in the home, and 16% cited situations of deprivation as factors that contributed to their migration [69].
Access to inpatient and outpatient mental health services is very limited. A report from the Pan American Health Organization (PAHO) found that only 363 Guatemalan patients were able to access national outpatient mental health facilities, 58% of whom were women, and 14% of whom were children or teens. Of those treated, anxiety disorders were the most common diagnoses [70]. Due to limited access to outpatient and inpatient psychiatric treatment in El Salvador, Guatemala, and Honduras, it is difficult to determine the prevalence and types of mental health issues among children and adults.
Once in the United States, these refugee children must adapt to a new physical environment and culture. Leaving behind family and loved ones in their home country and adapting to life in the United States, coupled with the stress associated with being alone and potentially reuniting with unfamiliar or unknown relatives, can have severe consequences. These factors increase the risk for depression, anxiety, PTSD, substance abuse, and homelessness [71]. Therefore, it is important to evaluate these children for mental health issues at initial screening and on an ongoing basis through frequent visits with appropriately trained mental health and primary care providers.
Nutrition: Double Burden of Malnutrition and Obesity
El Salvador, Guatemala, and Honduras have reported high rates of low birth weight in infants (birth weight <2,500g), as well as high rates of malnutrition among infants and children. However, there is an increasing prevalence of overweight and obesity among older children, teens, and adults. This paradox of poor nutrition in early childhood followed by obesity in older children and adults has been described as the “double burden” of malnutrition faced in many developing countries.
Malnutrition
Inequalities and extreme poverty directly affect food security and nutrition, particularly in rural areas of El Salvador. It is estimated that 16.3% of rural Salvadoran families are unable to cover the costs of basic food needs [72]. Additionally, 18.9% of all children under age 5 experience chronic undernutrition, with 25.6% of children living in rural regions experiencing chronic undernutrition [72]. Overall, approximately 21% of Salvadoran children are stunted, while 6% are underweight, and 2% are wasted [53, 73]. It is estimated that malnutrition contributes to more than 30% of all childhood deaths, as chronic undernutrition is known to increase severity of disease [53]. Micronutrient deficiencies, including vitamin A deficiency, are also common in young children [53].
Rural, indigenous populations in Guatemala are often the impacted by food and economic insecurities. Guatemala has the third-highest rate of stunting, or chronic malnutrition, worldwide [54, 74]. Indigenous populations are disproportionately affected and suffer from malnutrition at twice the rate of non-indigenous children [54, 73]. Approximately 49.8% of all Guatemalan children are undernourished, while 69.5% of children in rural, indigenous areas are undernourished [75]. Micronutrient deficiencies are relatively common in Guatemala. A multiyear study revealed that 16% of preschool children are vitamin A deficient [76]. Iodine deficiency has also been observed, and it is reported that less than 50% of families use iodized salt [54].
Poverty is widespread in Honduras, with 75% of the population living in extreme poverty and 12% of households being food-insecure [77, 78]. As in other Central American nations, stunting and malnutrition remain major concerns, particularly for children living in rural areas. Up to 50% of children in some regions are stunted, and children living in rural areas are 2.5 times more at risk for growth faltering than children who live in urban areas [55]. Additionally, children in the poorest households are 8 times more likely to be stunted than children born to wealthy families [55]. Chronic malnutrition can be as high as 48.5% in some rural areas [77]. Micronutrient deficiencies, including vitamin A and iron deficiencies, are common in Honduras and are often observed in young children and pregnant women [55].
All children between 6 months and 59 months old should be prescribed multivitamins with iron. Older children who are malnourished should also take multivitamins for presumed micronutrient deficiency.
Overweight and Obesity
Although stunting and malnutrition affect large numbers of children in El Salvador, Guatemala, and Honduras, overweight and obesity are growing problems. In Latin America, it is estimated that between 42.5 and 51.8 million children aged 0-18 years are overweight or obese [79]. Studies indicate that 5% to 6.5%, 13%, and 7.1% of children under 5 years old are overweight or obese in El Salvador, Guatemala, and Honduras, respectively [80]. To date, few countries have implemented national programs or policies to combat the obesity epidemic in Latin America [79].
Overweight and obesity are also increasing among adults, with up to 60% of adults in some Latin American countries classified as overweight or obese [81]. Furthermore, models predict increases in overweight and obesity in Latin Americans by 2050 [81]. Recent studies indicate that 67% of Guatemalans over 15 years old are overweight, 29% of whom are obese [54, 82]. In Honduras, 46% of all people 15 years and over are either overweight or obese [55, 82], while 49% of adults in El Salvador are either overweight or obese [53, 83]. Overweight and obesity, for both children and adults, are largely due to rapid urbanization, adoption of modern Western diets high in refined carbohydrates, saturated fats, and sugars, and increasingly sedentary lifestyles. Additionally, slow progress in improving community infrastructure and public health systems have contributed to overweight and obesity epidemics [53-55, 84].
Children who are overweight (BMI 85th-95th percentile) or obese (BMI >95 percentile) should be followed closely. Overweight or obese children and their family members should be offered dietary counseling and support [85]. All children, regardless of nutrition status, should have blood pressure checked starting at 3 years old and followed annually [86]. Fact sheets and other health promotional materials for healthy eating and physical activity should be shared with all newly arrived patients and family members, regardless of nutritional status upon arrival.
See CDC nutrition-growth guidelines for further recommendations and guidelines regarding nutritional assessment and management among newly arrived refugee children.
Summary
The information provided in this refugee health profile is intended to help resettlement agencies and healthcare providers gain a better understanding of Central American populations entering the United States, including their cultural backgrounds and population-specific health issues. The following health conditions are considered priorities for screening and evaluation in these groups: mental health, soil-transmitted helminths, Chagas, anemia, lead exposure, and nutritional status (malnutrition or obesity/overweight).