Tuberculosis Technical Instructions for Panel Physicians
At a Glance
The medical screening for tuberculosis among persons overseas applying for U.S. immigration status and nonimmigrants who are required to have an overseas medical examination, hereafter referred to as applicants, is an essential component of the immigration medical examination. One of the goals of the immigration medical examination is to diagnose and treat certain infectious diseases, and thus the primary focus of these instructions is infectious tuberculosis disease.
Background
The Centers for Disease Control and Prevention (CDC) Division of Global Migration Health (DGMH) developed these instructions in consultation with U.S. tuberculosis subject matter experts and U.S. panel physicians. These instructions define the specific responsibilities of panel physicians in terms of testing for and treatment of infectious tuberculosis disease among applicants overseas. For the purposes of these instructions, the term infectious tuberculosis disease refers to tuberculosis disease of the lung parenchyma, pleura, larynx, or intrathoracic lymph nodes. Other forms of extrapulmonary tuberculosis and latent tuberculosis infection (LTBI) are not included in the definition of infectious tuberculosis disease and are defined separately.
These instructions are specific to the immigration medical examination and should not be used as guidance to test for or treat tuberculosis disease in other settings or as a clinical manual that defines detailed laboratory procedures or specific treatment regimen details. Treatment of applicants for drug-susceptible tuberculosis disease must be consistent with current CDC guidance: Treatment for TB Disease.
The instructions in this document supersede all previous Tuberculosis Technical Instructions, Updates to the Technical Instructions and communications to panel physicians and international refugee resettlement organizations. These instructions must be followed for tuberculosis disease screening and treatment of all applicants. The molecular testing requirement, interferon-gamma release assay (IGRA) testing for adults and changes to drug susceptibility testing (DST) defined in these instructions go into effect no later than October 1, 2024; all other components of these instructions go into effect January 24, 2024.
Applicants in all countries who are ≥15 years old must have a chest x-ray.
Applicants 2 years of age and older examined in countries with a World Health Organization (WHO)-estimated tuberculosis incidence rate of ≥20 cases per 100,000 population must have an interferon-gamma release assay (IGRA).
Human immunodeficiency virus (HIV) testing is not a part of the U.S. medical screening process; however, panel physicians may advise applicants for whom testing is clinically indicated about HIV testing.
Infectious tuberculosis disease screening requirements vary based on age of applicant and the WHO-estimated tuberculosis disease incidence rate in the country where the exam occurs. A complete screening medical examination for tuberculosis disease consists of a medical history, physical examination, then the following items when required by these instructions: IGRA; chest x-ray; sputum samples for molecular testing on the first sputum sample, smears for acid-fast bacilli (AFB), solid and liquid culture testing for mycobacteria with confirmation of the Mycobacterium species at least to the M. tuberculosis complex level; and drug susceptibility testing (DST) for positive cultures.
HIV testing is not a part of the U.S. medical screening process; however, panel physicians may advise applicants for whom testing is clinically indicated about HIV testing. Such applicants may include those with signs or symptoms suggestive of HIV infection or those with tuberculosis disease. For such applicants, the consent for HIV testing should include the following:
- Applicants understand they do not have to be tested for HIV.
- Applicants understand that if they would like to be tested for HIV, they do not have to be tested for HIV by a panel physician.
- Applicants understand that panel physicians must include the test results on the paperwork they complete.
If applicants who would benefit from HIV testing provide consent, panel physicians should perform HIV testing consistent with the standards of testing in their countries.
People with HIV infection are less likely to have an abnormal chest x-ray or positive IGRA during infectious tuberculosis disease; and negative IGRA results do not rule out infectious tuberculosis disease; thus, all applicants with known HIV infection must provide three sputum specimens for smears and culture plus molecular testing of the first sample, regardless of IGRA or chest x-ray results, to rule out infectious tuberculosis disease.
Additionally, applicants diagnosed with extrapulmonary tuberculosis only (of sites other than the larynx, pleura, intrathoracic lymph nodes, or lung parenchyma) must have a chest x-ray and must provide three sputum specimens for smears and culture plus molecular testing of the first sample, regardless of IGRA or chest x-ray results, in order to rule out infectious tuberculosis disease.
Tuberculosis Screening Protocols by Country Incidence
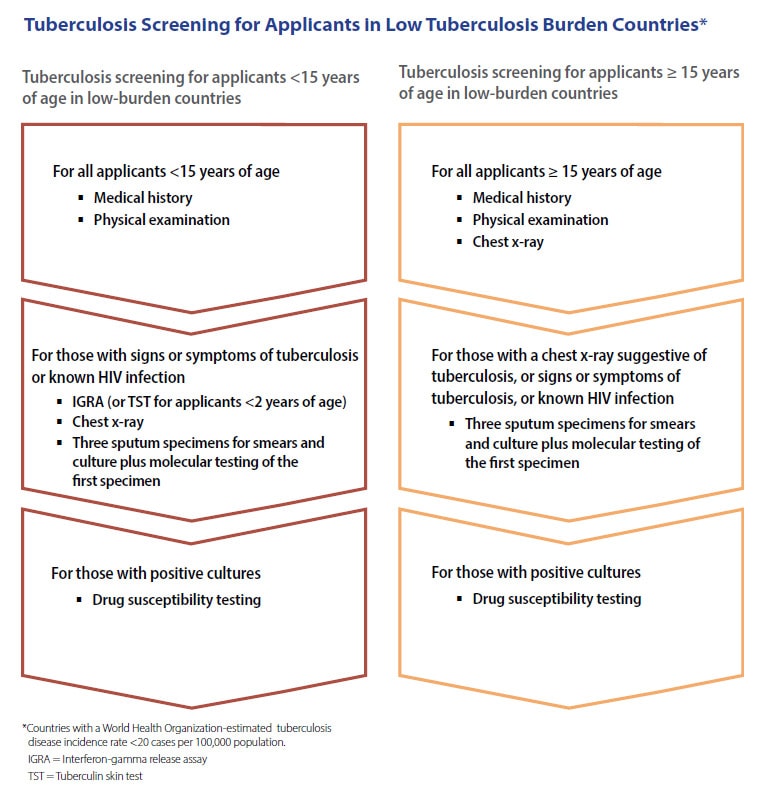
Tuberculosis screening for applicants in countries with a WHO-estimated tuberculosis disease incidence rate of <20 cases per 100,000 population
All applicants <15 years of age examined in low tuberculosis burden countries, defined as countries with a WHO-estimated tuberculosis disease incidence rate of <20 cases per 100,000 population, must have a physical examination and history provided by a parent or responsible adult who knows the child best. Those applicants who have signs or symptoms suggestive of infectious tuberculosis disease or have known HIV infection must have an IGRA (tuberculin skin test [TST] may be used for those < 2 years of age) and a chest x-ray (anteroposterior or posteroanterior view and a lateral view for applicants <10 years of age; posteroanterior view for applicants ≥10 years of age). Those applicants must also provide three sputum specimens for smears and culture plus molecular testing of the first sample.
Applicants ≥15 years of age examined in these countries must have a medical history, physical examination, and chest x-ray (posteroanterior view). Those applicants who have signs or symptoms suggestive of infectious tuberculosis disease, chest x-ray findings suggestive of infectious tuberculosis disease, or known HIV infection must provide three sputum specimens for smears and culture plus molecular testing of the first sample.
Tuberculosis Screening for Applicants in Low Tuberculosis Burden Countries
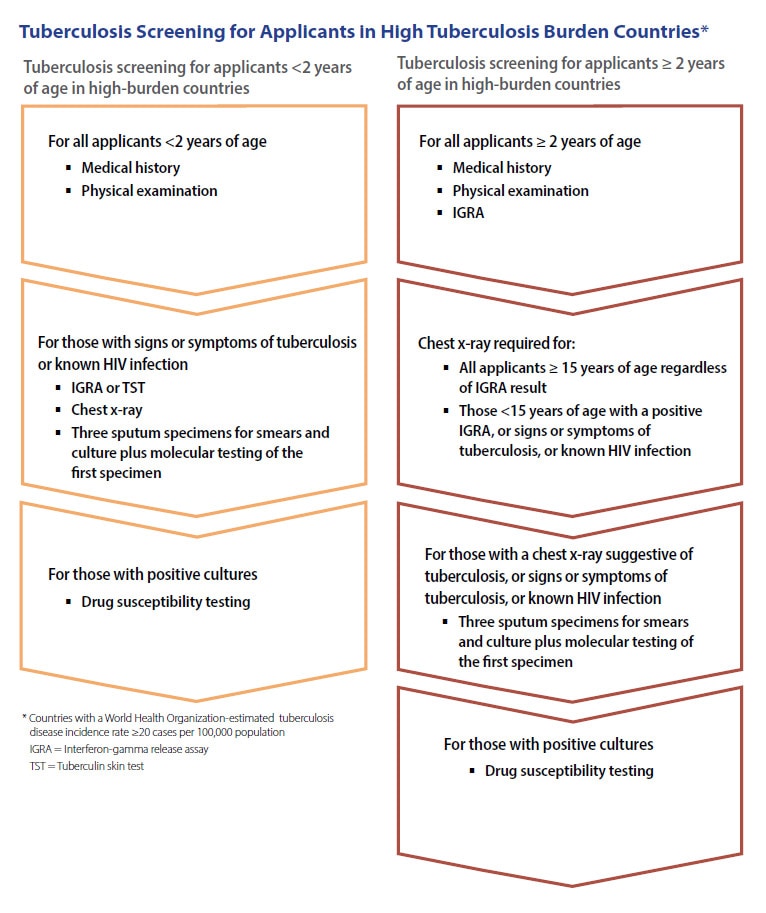
Tuberculosis screening for applicants in countries with a WHO-estimated tuberculosis disease incidence rate of ≥20 cases per 100,000 population
All applicants <2 years of age examined in countries with a WHO-estimated tuberculosis disease incidence rate of ≥20 cases per 100,000 population, must have a physical examination and history provided by a parent or responsible adult who knows the child best. Applicants who have signs or symptoms suggestive of infectious tuberculosis disease or have known HIV infection must have an IGRA or tuberculin skin test (TST) and a chest x-ray (anteroposterior or posteroanterior view and a lateral view) and must provide three sputum specimens for smears and culture plus molecular testing of the first sample.
IGRA testing is required for all applicants ≥2 years of age who are examined in countries with a WHO-estimated tuberculosis disease incidence rate of ≥20 cases per 100,000 population. IGRA must be performed for these applicants if a U.S. Food and Drug Administration (FDA)-approved or WHO-approved IGRA test is licensed for use in the country in which the panel physician is practicing. If an FDA-approved or WHO-approved IGRA is not available for use in the country, the panel physician must contact DGMH by emailing cdcqap@cdc.gov for further guidance. IGRA testing in these countries for applicants ≥15 years must be implemented by October 1, 2024.
For children 2 through 14 years old, if the IGRA is positive or if the applicant has signs or symptoms of infectious tuberculosis disease or has known HIV infection, a chest x-ray (anteroposterior or posteroanterior view and a lateral view for applicants <10 years of age; posteroanterior view for applicants ≥10 years of age) must be performed. Applicants who have a chest x-ray with findings suggestive of infectious tuberculosis disease, signs or symptoms of tuberculosis disease, or known HIV infection must provide three sputum specimens for smears and culture plus molecular testing of the first sample.
Applicants ≥15 years of age who are examined in high-tuberculosis-burden countries must have a chest x-ray regardless of IGRA result. Applicants who have a chest x-ray with findings suggestive of infectious tuberculosis disease, signs or symptoms of tuberculosis disease, or known HIV infection must provide three sputum specimens for smears and culture plus molecular testing of the first sample.
Each aspect of the examination for tuberculosis is detailed below.
Tuberculosis Screening for Applicants in High Tuberculosis Burden Countries
Initial Evaluation
Medical History
- The medical history should focus on risk factors for infectious tuberculosis disease, including previous history of tuberculosis disease; illness suggestive of tuberculosis disease (such as cough of ≥3 weeks’ duration, dyspnea, weight loss, fever, or hemoptysis); prior treatment suggestive of tuberculosis disease treatment; and prior diagnostic evaluation suggestive of tuberculosis disease. The clinical expression of infectious tuberculosis disease may be different in children than in adults, and for children may only include generalized findings such as fever, night sweats, growth delay, and weight loss. Children are also more prone to extrapulmonary tuberculosis, such as meningitis, and disease of the middle ear and mastoid, lymph nodes, bones, joints, and skin.
- The medical history should also include inquiries regarding family or household contact with a person who has or had tuberculosis disease, or an illness, treatment, or diagnostic evaluation suggestive of tuberculosis disease.
Physical Exam
Pertinent elements of the physical examination for infectious tuberculosis disease include general characteristics such as height, weight, temperature, heart rate, respiratory rate, and blood pressure; a thorough pulmonary examination; inspection and palpation of lymph nodes; and inspection for scars of scrofula or prior chest surgery.
Immune Response to M. tuberculosis Antigens
Applicants ≥2 years of age examined in high tuberculosis burden countries must have an IGRA test to determine immune response to M. tuberculosis antigens.
Exceptions include applicants with written documentation from a physician of a previous positive IGRA. For past positive IGRA results, the written documentation must include date of the test, type of IGRA performed, test results in standard units of measurement, the test interpretation (i.e., positive), and the testing physician’s name, signature, and office information. Applicants ≥2 years of age examined in high-tuberculosis-burden countries who provide documentation of a previous positive TST must still have an IGRA performed; if the IGRA is negative, the applicant is considered to have a negative immune response to M. tuberculosis antigens in this examination.
- IGRA – CDC will allow use of IGRA tests approved by the FDA or WHO. If the panel physician does not have access to an approved IGRA test, the panel physician must contact DGMH by emailing cdcqap@cdc.gov for further guidance. Panel physicians must follow the manufacturers’ written instructions for collecting samples, performing tests, and interpreting test results. IGRA results must be available within 72 hours of sample collection. For these Technical Instructions only, an indeterminate test result must be documented as indeterminate and not result in repeat testing by the panel physician, chest x-ray, nor B2 classification. However, for applicants with an indeterminate test result, a repeat IGRA after arrival in the U.S. is recommended for their health, but not required.
- TST – TST may only be used in children under 2 years of age when indicated, or when IGRA is not available and use of TST is approved by DGMH. Tuberculin purified protein derivative (PPD) must be administered intradermally by the Mantoux method. Ideally, preparations used should be equivalent to 5TU PPD-S. However, in countries where such preparations are limited or impossible to import, panel physicians must use PPD preparations that are approved for use by their ministries of health. The type of PPD used must be documented. A TST is considered positive if it results in induration ≥10 mm (≥5 mm if applicant is HIV-positive or a known recent contact to a person with tuberculosis disease).
Chest Radiography
When performed, chest radiography (chest x-ray) must consist of a standard posteroanterior view for all applicants ≥10 years of age. Applicants <10 years of age who receive a chest x-ray must have a standard anteroposterior or standard posteroanterior view and must also have a lateral view. The chest x-ray must be labeled “PA” or “AP” for the benefit of the radiologist’s review. Additional views can be taken if clinically appropriate.
Chest x-rays must be interpreted by a radiologist and reviewed by the panel physician. The radiologist who interprets the image must complete and sign the radiology portion of the U.S. Department of State (DS) form or U.S. eMedical application. Interpreting radiologists must be licensed to practice medicine and board certified in radiology either in the U.S. or by equivalent regional/national credentialing entities. Chest x-ray results should be available same day but must be available no later than 3 days from the time they were performed. An applicant’s chest x-ray must be retaken if the initial chest x-ray is suboptimal because of factors such as motion artifact or low lung volumes. Chest x-ray interpretations should include comparisons with prior chest x-rays, if available.
Applicants with clinical and radiographic findings suggestive of common bacterial infections of the respiratory tract may be treated with a course of antibiotics. However, fluoroquinolones should not be used for empiric treatment of respiratory infections because they are a mainstay of first- and second-line therapy for tuberculosis disease, and their use could both result in mistreatment of tuberculosis disease and lead to drug resistance. The chest x-ray for medical screening should not be performed until at least 8 weeks after treatment for respiratory tract infections unless the applicant’s clinical status warrants further evaluation earlier than 8 weeks after therapy.
Applicants who are pregnant may postpone the required immigration chest x-ray (and immigration medical examination) until after pregnancy but are required to have a chest x-ray to immigrate. Pregnant applicants should discuss this matter with the Department of State (DOS) consular officer to determine if the delay will affect their immigration status. If panel physicians choose to obtain consent from pregnant women for the chest x-ray, they should develop their own consent form. Lead shielding practices for applicants should follow applicable local laws and regulations; however, lead shielding is no longer recommended or required for the immigration medical examination for any applicants, including those who are pregnant.
The panel sites must use digital radiography (computed radiography (CR) or direct digital radiography (DDR)) to obtain plain chest x-rays for applicants. Digitized analog images are not digital images and are not acceptable.
Digital radiography equipment systems and interpretations must meet the following requirements:
- Images must be interpreted by a radiologist on a high-resolution screen. The screens used by radiologists must be medical-grade monitors that are at least 3 megapixels (MP) in “display resolution” AND that are advertised as being appropriate for primary image interpretation (not for image review). The screens used by the panel physicians to review the images are not required to meet this standard.
- Images may not be interpreted from laser-printed films, as the quality of printing varies greatly, and film format cannot be optimized.
- Images must be DICOM compatible and sized within 3.5-5MB to be uploaded into eMedical.
Sputum Testing
Sputum Collection and Transport
- Laboratory examination for infectious tuberculosis disease must consist of at least three sputum specimens. Each specimen must undergo microscopy for AFB (sputum smear) as well as culture for mycobacteria, confirmation of the Mycobacterium species at least to the M. tuberculosis complex level, and DST for cultures positive for M. tuberculosis complex. A molecular test must be performed on the first sputum specimen for all applicants from whom sputum is collected.
- Once the panel physician notifies the applicant that sputum specimens are required, the applicant must report for testing as soon as possible. If testing is delayed longer than 2 weeks, the panel physician should strongly consider testing the applicant for the presence of medications used to treat tuberculosis disease.
- The sputum specimen must be an early morning fasting specimen, and collection must be directly observed by a healthcare provider. Applicants should be instructed not to brush their teeth, use mouth wash, or eat anything prior to sputum collection. Three specimens consisting of 5–10 mL each must be collected at least 24 hours apart, preferably on consecutive working days. Applicants must rinse their mouths with purified or distilled water before providing a sputum specimen. Do not use water from plastic water dispensers, water coolers or sinks, even if filtered.
- Salivary specimens are unacceptable. The collection of a good-quality sputum specimen is of critical importance to rule out infectious tuberculosis disease, and the person collecting sputum must ensure it is not a salivary specimen before sending it to the laboratory.
- For applicants who have difficulty producing sputum, there are several methods of obtaining a specimen. Inhalation of an aerosol of sterile hypertonic saline (3%–5%), usually produced by an ultrasonic nebulizer, can be used to stimulate the production of sputum (sputum induction). Sputum induction can be used for children as young as 3 years of age. Even though aerosol-induced specimens may appear thin and watery, they should be processed. The specimen must be labeled clearly as “induced sputum” so it will not be discarded by the laboratory as an inadequate (salivary) specimen.
- Although sputum testing is best, for the small number of applicants unable to produce sputum specimens even with induction (such as young children or people with advanced dementia) alternative methods of specimen collection and testing must be performed. These methods include molecular testing of stool, early morning gastric aspirates and flexible bronchoscopy.
- For the small number of people unable to produce sputum even with induction, a molecular test performed on three stool specimens is an acceptable first alternative. A molecular stool test can be performed if the panel-designated laboratory has completed an internal validation of the test for that purpose and testing has been approved for use in the country in which the panel physician practices. Three specimens must be collected, preferably on consecutive days. If an applicant has a positive stool test, three gastric aspirates must be collected to attempt to culture the organism and allow DST.
- If neither sputum nor stool testing is possible a gastric aspirate specimen can be used for any aged applicant and may be especially helpful for young children. Three specimens must be collected, preferably on consecutive days. Detailed gastric aspirate guidance is published by the Curry International Tuberculosis Center.
- If an adult is unable to provide sputum and stool testing or gastric aspirates are not available, flexible bronchoscopy is acceptable for obtaining a specimen, but is the most invasive of the three alternative methods. Contact DGMH for approval by emailing cdcqap@cdc.gov if planning to use this procedure. If bronchoscopy is used, only one procedure is required. During the bronchoscopy, two specimens must be obtained from different areas of the lung. These specimens must then be sent to the laboratory for AFB smears and cultures. If the panel-designated laboratory has completed an internal validation of molecular testing of bronchoscopy specimens and testing has been approved for use in the country in which the panel physician practices, both specimens should also be sent for molecular testing.
- Specimens must be transported to the laboratory promptly within 24 hours after collection. If not transported within 1 hour, specimens must be refrigerated (but not frozen). Specimens received in the laboratory must be kept refrigerated and processed within 24 hours of receipt.
Sputum Smears
Sputum specimens must undergo centrifugation before smears are performed. Applicants who have sputum smears that are positive for AFB by microscopy should be started on treatment for infectious tuberculosis disease. If molecular testing on smear-positive specimens is negative, panel physicians may wait to start treatment until culture results are reported if, in their clinical judgment, the applicant might not have infectious tuberculosis disease. If treatment is started and the applicant’s cultures are subsequently negative, panel physicians should use their clinical judgment to determine whether continued treatment for infectious tuberculosis disease is warranted. If the decision is made that the applicant does not have infectious tuberculosis disease, treatment may be stopped and the applicant may be given a Class B1 TB, Pulmonary classification and allowed to travel.
Molecular Testing
A molecular test must be performed on the first sputum specimen from all applicants from whom sputum is collected for initial diagnosis. Panel physicians can only use tests that have regulatory approval in the country in which they will be used, and only use the tests for the purposes for which they have been approved. This molecular test must be a diagnostic nucleic acid amplification test (NAAT), but otherwise the panel physician can choose the test they use, and a specific manufacturer or product is not required. Panels can use tests that detect drug resistance, which can be helpful but is not required.
If the molecular test is positive, the panel physician can begin treatment for the applicant based on these results. However, a negative molecular test cannot be used to rule out infectious tuberculosis disease, and the applicant must wait for culture results (limited exceptions defined below). If the molecular test is negative, and at least one culture is positive, the applicant must be diagnosed with Class A, infectious tuberculosis disease. If the molecular test is positive and all cultures are negative, the physician should use their clinical judgement in diagnosing the patient.
Molecular tests are only required to be performed on the first diagnostic sputum specimen and are not recommended or required for follow-up testing.
Culture and Drug Susceptibility Testing
All sputum specimens must be cultured for mycobacteria and confirmation of the Mycobacterium species, at least to the M. tuberculosis complex level.
All positive cultures must undergo DST for isoniazid, rifampin, ethambutol, pyrazinamide and a fluoroquinolone (e.g., ofloxacin, levofloxacin, moxifloxacin).
All sputum specimens must be cultured for mycobacteria and confirmation of the Mycobacterium species, at least to the M. tuberculosis complex level. A total of 3 cultures must be performed for each of the three sputum samples, which must include two (2) solid cultures and one (1) liquid culture (for a total of 9 cultures). Löwenstein–Jensen (LJ) media must be used for solid cultures and mycobacterial growth indicator tube (MGIT) media must be used for the liquid cultures. Specimens must be incubated for a minimum of 6 weeks for liquid cultures and 8 weeks for solid cultures, before a final negative report can be issued. Positive cultures must be reported as soon as the results are known.
- Positive M. tuberculosis cultures must undergo DST for isoniazid, rifampin, ethambutol, pyrazinamide and a fluoroquinolone (e.g., ofloxacin, levofloxacin, moxifloxacin). Panel physicians must have access to DST results within 10 weeks of sputum collection.
- Positive M. tuberculosis cultures that are resistant to rifampin (either rifampin mono-resistant or with isoniazid resistance) must undergo drug susceptibility testing for second-line anti-tuberculosis medications. At a minimum, second-line DST must include testing for the classes of drugs to be used for the infectious tuberculosis disease treatment regimen.
- Applicants who have negative sputum smears and cultures but have one of the cultures reported as “contaminated” may still be cleared for travel. When applicants have 2 or more contaminated cultures, panel sites and their designated laboratories should review their procedures and collect three additional sputum specimens from the applicant for AFB smear and culture.
In addition to these requirements provided, panel physicians should use their clinical judgment in the evaluation and diagnosis of infectious tuberculosis disease.
Any applicant diagnosed with infectious tuberculosis disease who needs treatment must receive a classification of Class A TB and is not cleared for travel until successful treatment completion, regardless of the diagnostic criteria.
Applicants must be assigned one or more tuberculosis classifications on the DS forms or in eMedical.
The tuberculosis classifications and travel clearance times are listed below.
No TB Classification
Applicants without current clinical findings of infectious tuberculosis disease or extrapulmonary tuberculosis, without known HIV infection, and, for those applicants who require additional screening, with a normal chest x-ray and a negative IGRA for those who require it. Travel clearance for these applicants is valid for 6 months from the time the evaluation is complete.
All applicants who are diagnosed with infectious tuberculosis disease. All applicants with 1 or more cultures positive for M. tuberculosis complex must be diagnosed with infectious tuberculosis disease regardless of other test results or clinical findings. Infectious tuberculosis can also be diagnosed clinically based on signs and symptoms. This classification also applies to applicants with extrapulmonary tuberculosis who have a chest x-ray suggestive of infectious tuberculosis disease, regardless of sputum smear and culture results. These applicants are not cleared for travel until completion of treatment unless a waiver is granted.
Class B0 TB, Pulmonary
Applicants who were diagnosed with infectious tuberculosis disease by the panel physician or presented to the panel physician while on tuberculosis treatment and successfully completed DGMH-defined DOT under the supervision of a panel physician prior to immigration. Travel clearance is valid for 3 months from the date final (end of treatment) cultures are reported as negative.
Class B1 TB, Pulmonary
Applicants who have signs or symptoms, physical exam, or chest x-ray findings suggestive of infectious tuberculosis disease, or have known HIV infection, but have negative cultures and are not diagnosed with infectious tuberculosis disease. The IGRA result can be either positive or negative and does not affect the B1 classification. This classification also includes applicants who were diagnosed with infectious tuberculosis disease by the panel physician, refused DGMH-defined DOT treatment, and are returning after treatment and completion of a minimum 1-year wait. Travel clearance is valid for 3 months from the date final cultures are reported as negative.
Applicants diagnosed with extrapulmonary tuberculosis with a normal chest x-ray and negative sputum cultures. Travel clearance is valid for 3 months from the date final cultures are reported as negative.
Applicants who have a positive IGRA or TST but otherwise have a negative evaluation for tuberculosis disease. The IGRA result or size of the TST reaction, the applicant’s status with respect to LTBI treatment, and the medication(s) used must be documented. For applicants who had more than one IGRA or TST, all dates and results and whether the applicant’s IGRA or TST converted must be documented. Known contacts as defined below with a positive IGRA or TST ≥5 mm must receive this classification in addition to a Class B3, Contact Evaluation classification (if they are not already Class B0 TB, Pulmonary; B1 TB, Pulmonary; B1 TB, Extrapulmonary; or Class A TB). Travel clearance is valid for 6 months from the time the evaluation is complete.
Class B3 TB, Contact Evaluation
Applicants who are a recent contact of a person with known infectious tuberculosis disease, regardless of IGRA or TST results. The IGRA result or the size of the applicant’s TST reaction must be documented. Applicants can be both Class B3 and Class B1 (a contact who required sputum testing with negative cultures), or Class B3 and Class B2 (a contact with LTBI). However, other combinations of tuberculosis classifications are not permitted.
Information about the source case, name, alien number (if applicable), relationship to contact, and drug resistance of tuberculosis disease must also be documented. Additional information can be found in the Contacts of Tuberculosis Cases section. Travel clearance for Class B3 and B3/B2 is valid for 6 months from the time the evaluation is complete. Travel clearance for Class B1/B3 is valid for 3 months from the date final cultures are reported as negative.
TB Classification Pending
Applicants with signs or symptoms suggestive of infectious tuberculosis disease, a chest x-ray suggestive of infectious tuberculosis disease, known HIV infection, or extrapulmonary tuberculosis only, must provide three sputum specimens for molecular testing (of the first sample), AFB smears and culture. Any laboratory or additional studies deemed necessary, either as a result of the physical examination or pertinent information elicited from the applicant’s medical history, must be performed to reach a conclusion about the presence or absence of infectious tuberculosis disease. While results are pending, applicants will have this classification.
Additional Information about TB Classifications and Travel Clearance
Applicants who have been diagnosed with infectious tuberculosis disease by panel physicians and who do not receive DGMH-defined DOT are not cleared for travel. These applicants will need to repeat their medical screening examination at least 1 year after treatment is completed. If the tuberculosis disease examination is negative at that time, the applicant can be cleared for travel. The applicant must receive a Class B1 TB, Pulmonary classification. See the “Tuberculosis Treatment” section of this document for additional information.
Limited Exception to allow children to travel while cultures are pending
Applicants 10 years of age or younger who require sputum cultures, regardless of HIV infection status, may travel to the United States immediately after sputum smear analysis and molecular test results are reported as negative (while culture results are pending) if none of the following three conditions exist:
- Chest radiograph findings include either one or more cavities or extensive disease (e.g., particularly if involving both upper lobes)
- Respiratory symptoms include a forceful and productive cough
- Known contact with a person with multidrug-resistant tuberculosis disease (MDR TB) who was infectious at the time of contact
This can only occur for applicants who are traveling immediately and can be seen by a U.S. healthcare provider within days of arrival, such as international adoptees. For applicants 10 years of age or younger who travel to the United States while results of cultures are pending, the panel physicians must:
- Give the applicant a Class B1 TB, Pulmonary classification.
- Document that culture results are pending.
- Email culture results to DGMH at cdcQAP@cdc.gov so that DGMH can send the culture results to the receiving U.S. health departments.
If the child will not travel until after culture results are reported, panel physicians must wait to complete the DS forms or the eMedical documentation until results are available. If the child will travel while results of cultures are pending, the panel physician must enter “pending” in the “Date specimen reported” field while cultures are pending.
People with a past history of a Tuberculosis Condition
It is possible to have infectious tuberculosis disease more than once, and it is possible to develop infectious tuberculosis after appropriate treatment for LTBI. Thus, people with these histories must be screened and have specific considerations:
- People with a history of LTBI treatment with documentation of the treatment still need a chest x-ray. If the chest x-ray is negative, and they have no signs or symptoms of tuberculosis and no known HIV, they can receive a classification of “No TB Classification”.
- Children and adults with a history of tuberculosis disease must have a chest x-ray regardless of IGRA results and country of exam.
- Applicants with a well-documented remote history of having completed treatment for tuberculosis disease (1 or more years ago) who have a normal chest x-ray, no current signs or symptoms of infectious tuberculosis disease, and no known HIV infection should be assigned “No TB Classification” regardless of IGRA results. This includes applicants who were treated by the panel physician or other sites. If the history is not well-documented, and the IGRA is positive, the applicant must receive a B2 classification.
- People with a history of treated infectious tuberculosis disease may have residual DNA from dead Mycobacterium tuberculosis organisms, that can cause a false positive result on molecular tests. The panel physician should take this into consideration and use clinical judgment when interpreting results for these applicants to determine if this represents new or past infection.
Conditions that do not prevent travel
Latent Tuberculosis Infection (LTBI)
LTBI will typically present in a person without HIV as a positive IGRA with a negative chest x-ray and no signs or symptoms of infectious tuberculosis disease. LTBI is not an infectious condition and therefore treatment is not required for the purposes of immigration. Applicants diagnosed with LTBI must receive information about their diagnosis and treatment options and informed about how to find their local health department in the U.S. This information can be found here: why and where to seek LTBI treatment. Further information about applicants who have LTBI and are contacts of a person with known infectious tuberculosis disease can be found in the contacts section.
Nontuberculous Mycobacteria
If AFB smears are positive and the culture results are negative or demonstrate nontuberculous mycobacteria (NTM), panel physicians should use their clinical judgment in determining whether to continue treatment for infectious tuberculosis disease. NTM in smears or in culture can represent contamination or actual NTM disease, and the differentiation is outside the scope of these instructions. If applicants have NTM contamination of their laboratory results or NTM disease and the panel physician’s clinical judgement is that further treatment for infectious tuberculosis disease is not warranted, those applicants may be cleared for travel. NTM contamination or disease is not the same as infectious tuberculosis disease as defined in these Technical Instructions and is not a Class A condition.
An applicant may have a positive sputum smear but a negative molecular test because NTM organisms can cause positive AFB smears. In that scenario, panel physicians must use their clinical judgment to determine whether to start treatment for infectious tuberculosis disease while awaiting culture results.
The presence of NTM in culture results must be documented. If an applicant has culture results that are positive for NTM, but negative for M. tuberculosis complex, and the panel has no clinical suspicion for infectious tuberculosis disease, the applicant must receive a TB classification of either a Class B1 TB, Pulmonary classification if the NTM were found in the initial set of sputum cultures, or a Class B0 TB, Pulmonary if the NTM were found in the end of treatment cultures for someone who successfully completed infectious tuberculosis disease treatment with the panel physician.
Extrapulmonary Tuberculosis
Applicants diagnosed with extrapulmonary tuberculosis only must have a chest x-ray and must provide three sputum specimens for molecular testing (of the first sample), AFB smears and culture, regardless of chest x-ray results.
If the chest x-ray is suggestive of infectious tuberculosis disease, these applicants are Class A TB and must complete directly observed therapy (DOT) as defined by DGMH in these Technical Instructions even if sputum smears, molecular test and cultures are negative.
If the chest x-ray is normal, and the sputum smears, molecular test and cultures are negative, these applicants can be cleared for travel and assigned a Class B1 TB, Extrapulmonary tuberculosis classification.
Applicants with extrapulmonary tuberculosis only, normal chest x-ray, and negative sputum smears and cultures should be considered for extrapulmonary tuberculosis treatment if departure is not planned within 3 months or if withholding therapy would be harmful. These applicants should receive DGMH-defined DOT and be instructed on the importance of completing therapy after their arrival in the U.S. If started on treatment, they must be given a 30-day supply of medication at departure.
Tuberculosis Treatment and Monitoring
Tuberculosis Treatment
Treatment of tuberculosis disease must be administered following directly observed therapy (DOT). DOT as defined by DGMH is an adherence-enhancing strategy in which a health-care worker watches a patient swallow each dose of medication in person and documents each dose. DOT is the standard of care for all applicants with tuberculosis disease. Doses that are self-administered over weekends or holidays are not counted as directly observed doses.
Panel physicians must provide DOT to applicants or identify in-country treatment programs that follow the DOT standards defined in these Technical Instructions by DGMH. Treatment provided outside the panel physician clinic must be evaluated in advance and closely supervised by the panel physician to ensure compliance with the Technical Instructions.
Virtual or electronic DOT, the practice of observing a patient take medication over a phone or other electronic device rather than in person, is not approved in these Technical Instructions. Self-administered doses do not count towards treatment completion.
Medication regimens for drug-susceptible tuberculosis must be consistent with the current guidance: Treatment for TB Disease.
Use only quality-assured drugs. Consult the WHO Global Drug Facility (GDF) for first-line drugs and the International Dispensary Association (IDA, Amsterdam) or WHO Green Light Committee for second-line drugs.
The TB Centers of Excellence for Training, Education, and Medical Consultation (TB COEs), in partnership with DGMH’s Quality Assessment Program and supported by CDC’s Division of Tuberculosis Elimination (DTBE), provide an online Medical Consultation Service for U.S. panel physicians. This service is intended to be used by panel physicians who need expert consultations on unique or difficult clinical situations encountered while treating applicants for U.S. immigration who have tuberculosis disease. To request a consultation, please complete and submit the online Consultation Request Form.
Important Note – This service is exclusive to U.S. panel physicians and their direct staff. If you are not a panel physician and have a TB-related question, please send your inquiry to cdcinfo@cdc.gov.
The panel physician has an ethical obligation to make good-faith efforts to treat patients. Applicants diagnosed with infectious tuberculosis disease, regardless of laboratory and clinical criteria for the diagnosis, who do not want to receive DGMH-defined DOT, may not travel to the U.S. Panel physicians must notify the Consulate of any Class A applicants refusing DGMH-defined DOT for infectious tuberculosis disease. Panel physicians must notify the appropriate public health officials in their jurisdiction when they diagnose applicants with infectious tuberculosis disease and if efforts to treat them fail.
Identification of an applicant with rifampin resistance (mono-resistance, multidrug-resistant tuberculosis disease [MDR], or extensively drug-resistant [XDR] TB) must be reported to DGMH (cdcQAP@cdc.gov) within 1 week of receipt of the DST report.
Treatment of rifampin-resistant disease must be done in close consultation with experts in the management of such cases. If panel physicians are unable to determine if the treatment regimen is adequate for immigration they should request a consultation from the Tuberculosis Centers of Excellence (COEs) and ask if the proposed treatment regimen is consistent with U.S. standards. If treatment is managed by a national program, the panel physician is required to follow the treatment course, and alert DGMH if the treatment is not consistent with U.S. requirements according to the COE consult.
Additional guidance on treatment of drug-resistant tuberculosis disease can be found in Drug-Resistant Tuberculosis: A Survival Guide for Clinicians, 3rd edition, by the Curry International Tuberculosis Center and California Department of Public Health.
Applicants who are on treatment for infectious tuberculosis disease at the time of the examination must be transferred into a DGMH-defined DOT program provided by, or closely monitored by, the panel physician for the remainder of treatment, and have the following performed:
- Chest radiograph
- Three sputum specimens for smears and culture plus molecular testing of the first sample
- DST on positive cultures
When applicants on treatment for infectious tuberculosis disease at the time of examination had negative smears and cultures at the time of diagnosis, and remain culture-negative, panel physicians should use their clinical judgment to determine whether continued tuberculosis disease treatment is warranted. If it is the panel physician’s clinical judgement that further treatment is not clinically warranted, these applicants must be given a Class B1 TB, Pulmonary classification.
The panel physicians must provide DGMH-defined DOT at their clinics to applicants or refer the applicant to a program that will provide DGMH-defined DOT consistent with these Technical Instructions. When applicants are sent for treatment at national or other in-country programs for DOT, panel physicians must first ensure that the programs provide DGMH-defined DOT, and treatment regimens are consistent with CDC guidance, for example, as described here for drug-susceptible tuberculosis disease: Treatment for TB Disease and here for drug-resistant tuberculosis disease: Drug-Resistant TB. The panel physician must then collaborate with these designated treatment programs to ensure adequate completion of therapy for the applicants by reviewing treatment and testing records once a month at a minimum, and any additional measures deemed appropriate.
It is the panel physician’s responsibility to ensure that all applicants have an option to receive DGMH-defined DOT if they are diagnosed with infectious tuberculosis disease. Panel physicians must work with their national programs and colleagues to identify DGMH-defined DOT options in multiple regions of the country to accommodate applicants when possible. The panel physician must also explain to the applicants at the time of diagnosis that if they refuse to be treated at a site that provides DGMH-defined DOT treatment consistent with the Technical Instructions for the full duration of therapy, the applicant will be required to wait 1 year after treatment completion before they can be allowed to repeat the medical screening. For example, an applicant prescribed a 6-month treatment course would need to wait 1 year and 6 months before medical screening could be completed. Applicants refusing DGMH-defined DOT must sign a form stating that they refuse to be treated by DOT, and acknowledging that they are aware of the DOT treatment option, understand that documentation of treatment is required, and understand the required wait time.
All applicants who refuse DGMH-defined DOT must provide detailed documentation of their treatment to demonstrate having completed treatment for infectious tuberculosis disease. A letter from a physician stating they were treated is not sufficient. Documentation of treatment must include―
- Medication names
- Medication dosages
- Dates of delivery of each medication
- All sputum smear, molecular test, culture, and DST results performed by the treatment center
- Reports of all chest x-rays performed by the treatment center
The applicant’s treatment location, including physician name and clinic city and state, must be documented on the DS Forms or in eMedical. The applicant must provide this detailed report to the panel physician for review and the report must be attached to the travel documents of the applicant. Without this documentation, the applicant will not be considered further for immigration to the U.S. Please note that applicants who completed treatment for tuberculosis disease before their first immigration medical examination are not subject to this wait time.
Tuberculosis Treatment Monitoring
The frequency of laboratory testing required during treatment is based on drug-susceptibility testing results.
Children <10 years of age with drug-susceptible or culture-negative tuberculosis disease who cannot provide sputum specimens will not need to provide induced sputum or gastric aspirate specimens during treatment, unless their clinical course warrants further evaluation.
When signs of clinical worsening or failure to improve occur during therapy, such as persistent weight loss, fever, cough, or worsening chest x-ray, repeat smears, cultures, and DST are indicated.
Molecular testing is required for the first sputum specimen when diagnosing infectious tuberculosis disease, not for treatment monitoring.
This guidance for treatment monitoring differs from recommendations in the ATS/CDC/IDSA guidelines and Drug-Resistant Tuberculosis: A Survival Guide for Clinicians, 3rd edition, by the Curry International Tuberculosis Center and California Department of Public Health.
- Culture-positive and rifampin-sensitive: two sputum specimens must be collected and submitted for smears and culture once a month during therapy until cultures are negative for 2 consecutive months. Two sputum specimens must be collected and submitted for smears and culture at the end of therapy. See the sputum collection section for additional information about sputum collection.
- Culture-positive and rifampin-resistant: two sputum specimens must be collected and submitted for smears and culture once a month during therapy. Two sputum specimens must be collected and submitted for smears and culture at the end of therapy.
- No drug susceptibility testing results (culture-negative or contamination on DST specimen): one sputum specimen must be collected and submitted for smear and culture once a month during therapy. Two sputum specimens must be collected and submitted for smears and culture at the end of therapy.
Contacts of persons with infectious tuberculosis disease should be removed from exposure to the person with infectious tuberculosis disease if possible.
All contacts must receive an IGRA within 2 weeks of diagnosis of the potential source case.
Contacts who have clinical or chest x-ray findings suggestive of tuberculosis disease or known HIV infection must provide three sputum specimens for smears and culture plus molecular testing of the first sample.
If an applicant leaves for the United States and you later learn that they are a contact of someone with a positive culture, please notify DGMH (cdcQAP@cdc.gov), who will then notify the receiving health department.
A contact is a person who has shared the same enclosed air space in a household or other enclosed environment for a prolonged period (days or weeks, not minutes or hours) with a person with smear-positive or culture-positive tuberculosis disease. Contacts are at increased risk of infection with M. tuberculosis. The end of contact occurs when the person with infectious tuberculosis disease is isolated from others or the person’s sputum smears are negative after at least 2 weeks of treatment.
Applicants for U.S. immigration who are contacts must be evaluated for infectious tuberculosis disease by the panel physician. All such contacts must receive an IGRA.
If the IGRA is negative, negative chest x-ray (if required), no signs or symptoms of infectious tuberculosis disease, and no known HIV infection, the contact may be cleared for travel immediately. These applicants must be assigned a Class B3 TB, Contact Evaluation classification if traveling <8 weeks after contact ends. If the IGRA is negative, and the contact is not placed on prophylaxis and does not choose to travel immediately, and exposure continues, follow-up is recommended but not required, as follows: a repeat IGRA every 3 months until departure or until 8 weeks after contact ends, or the IGRA becomes positive. Contacts who travel ≥8 weeks after contact ends and have an IGRA that is negative done ≥8 weeks after the end of contact, should not receive a Class B3 TB, Contact Evaluation classification.
If the IGRA is positive, the contact must be further evaluated with medical history, physical examination, and chest x-ray. Contacts with clinical findings or chest x-ray suggestive of infectious tuberculosis disease, or known HIV infection, must provide three sputum specimens for smears and culture plus molecular testing of the first sample. Contacts diagnosed with tuberculosis disease must receive a Class A TB classification and must complete treatment for infectious tuberculosis disease before U.S. immigration.
If the IGRA is positive, but the chest x-ray is negative, there are no signs or symptoms of infectious tuberculosis disease, and no known HIV infection, the applicant must receive a classification of Class B2, LTBI evaluation and B3, Contact Evaluation and can be immediately cleared to travel. Although LTBI treatment is not required prior to travel, these applicants may be offered LTBI treatment (see below). If the applicant chooses not to travel immediately, and is not started on LTBI treatment, repeat evaluation including medical history, physical examination, and chest x-ray is recommended, but not required, every 3 months until departure. The classification for contacts with a positive IGRA result and no findings of infectious tuberculosis disease will remain Class B2, LTBI evaluation and B3, Contact Evaluation.
Contacts, regardless of IGRA results, who had clinical findings or chest x-ray suggestive of infectious tuberculosis disease or known HIV infection, had negative sputum cultures and are not being treated for infectious tuberculosis disease, must be classified as both Class B1 TB, Pulmonary, and Class B3 TB, Contact Evaluation if traveling less than 8 weeks after contact has ended.
All applicants who are identified as contacts with LTBI (both Class B2 and B3) should be encouraged to be treated for LTBI. Panel physicians may provide voluntary LTBI treatment if the panel physician is able to do so.
Special situations in which LTBI treatment (also called preventive therapy) should be initiated overseas include certain pediatric contacts (see information below) and contacts with impaired immunity (e.g., HIV infection).
- Children <4 years of age and applicants with impaired immunity (e.g., HIV infection) who are contacts of a person with known infectious tuberculosis disease, regardless of how that person was diagnosed, and who have a negative evaluation for tuberculosis disease (infectious or extrapulmonary), should begin directly observed preventive therapy (DOPT) regardless of IGRA results. Isoniazid may be used except in known exposures to a tuberculosis disease case with MDR TB or isoniazid resistance. Rifamycins may be used except in known exposures to a tuberculosis disease case with MDR TB or rifampin resistance. Advice on other preventive regimens based on drug resistance patterns of the tuberculosis disease case should be sought from experts at a COE.
- Children and applicants with impaired immunity (e.g., HIV infection) receiving preventive therapy should have an IGRA 8 weeks after exposure to the infectious case ends if the initial IGRA was negative. Preventive therapy may be discontinued if the IGRA is negative 8 weeks after exposure to the infectious case ends.
- Children and applicants with impaired immunity may be cleared for travel while on preventive therapy and should be assigned a tuberculosis classification (Class B3 TB, Contact Evaluation). If the applicant does not complete preventive therapy before departure, a 30-day supply of medication and instructions on how to take it should be given to the applicant or the parent or responsible adult traveling with the applicant.
Panel physicians do not need to wait on culture results from the person suspected of having infectious tuberculosis disease to classify applicants as contacts.
Applicants undergoing infectious tuberculosis disease treatment may petition for a Class A waiver.
In exceptional situations, applicants undergoing treatment for infectious tuberculosis disease can petition for a Class A waiver. Forms must be completed by the applicants, Form I-601 for immigrants, and Form I-602 for refugees. The U.S. Department of Homeland Security (DHS) reviews these petitions and considers them in situations with extenuating circumstances. DGMH reviews each petition and provides an opinion regarding the case to the requesting entity (U.S. Department of State or DHS). DHS then has the final authority to approve or deny the waiver request.
Applicants must obtain written approvals from both the US-based physician accepting responsibility for the applicant’s continued care and treatment and the U.S. local and state health departments with jurisdiction to accompany the request for waiver submitted to DHS.
As soon as the panel physician is aware that an applicant has applied for a Class A waiver, the panel physician must provide the following to CDC so that CDC can make a recommendation to DHS when the other components of the application are complete:
- Summary of case
- Completed DS forms
- All available pertinent laboratory results
- All chest x-ray images (in a DICOM format)
All medical documentation, including original laboratory reports, must be included with the required DS forms or in eMedical.
All required paper medical documentation must be sent by courier or other secure means to the U.S. Embassy for all Class A and Class B1 conditions. All Class A and Class B1 tuberculosis conditions must be reported to the U.S. Embassy upon detection.
If using paper forms, Department of State forms DS-2054, DS-3025, DS-3026, and DS-3030, and DICOM images of chest radiographs must be completed in their entirety and included in the applicant’s travel packet. This includes assigning a tuberculosis classification on the DS-2054 and DS-3030. Incomplete documentation may result in refusal to grant a visa or in designation of medical hold status at arrival to ports of entry.
For applicants requiring tuberculosis disease treatment before U.S. immigration, the panel physician is required to document the following:
- Chest radiograph findings and images before, during, and after treatment.
- Interferon gamma release assay results must include type of IGRA used (e.g.., QuantiFERON®, T-SPOT®, etc.), expiration date, and test result including units of measurement. If TST is used in a child under 2 or when granted permission by DGMH, TST documentation must include date of TST reading, name of product, expiration date, the type of product used (e.g., 5TU PPD-S), and results in millimeters of induration.
- Sputum smear results obtained before, during, and after treatment.
- Molecular test result from first sputum sample.
- Culture results obtained before, during, and after treatment, including for cultures that were contaminated.
- DST results performed on any positive cultures.
- DOT regimen received (including doses of all medications), start date, completion date, and any periods of interruption. Daily DOT record must also be included.
- Clinical course, such as clinical improvement or lack of improvement during and after treatment, including resolution of symptoms and signs and weight stability or gain.
Tuberculosis Indicators
DGMH is responsible for monitoring the effectiveness of these Technical Instructions in diagnosing applicants with tuberculosis. To assist with this monitoring, panel physicians must submit Tuberculosis Indicator reports to CDC/DGMH annually. The reports are to be submitted electronically via REDCap, and submission instructions are e-mailed to panel physicians at the beginning of each calendar year. Reports are due in April. Panel physicians who do not receive the reporting form by January of each year, or are new to the data submission process, should contact cdcQAP@cdc.gov for assistance.
Glossary of Abbreviations
| Acronym | Full Phrase |
|---|---|
| ATS | American Thoracic Society |
| CDC | U.S. Centers for Disease Control and Prevention |
| Chest x-ray | Chest radiograph |
| COE | Tuberculosis Centers of Excellence |
| DGMH | Division of Global Migration Health (CDC) |
| DOPT | Directly observed preventive therapy |
| DOT | Directly observed therapy |
| DST | Drug-susceptibility testing |
| DTBE | Division of Tuberculosis Elimination |
| FDA | U.S. Food and Drug Administration |
| GDF | WHO Global Drug Facility |
| HIV | Human immunodeficiency virus |
| IDA | International Dispensary Association |
| IDSA | Infectious Diseases Society of America |
| IGRA | Interferon gamma release assay |
| LTBI | Latent tuberculosis infection |
| MDR TB | Multidrug-resistant tuberculosis disease |
| PPD | Purified protein derivative |
| TST | Tuberculin skin test |
| WHO | World Health Organization |
| XDR TB | Extensively drug-resistant tuberculosis disease |
Definitions of Selected Terms as Used in these Technical Instructions
Contact – a person who has shared the same enclosed air space (i.e., exposed) in a household or other enclosed environment for a prolonged period (days or weeks, not minutes or hours) with a person with smear- or culture-positive pulmonary tuberculosis disease. Contacts exposed in this fashion to persons with smear- or culture-positive pulmonary tuberculosis disease are at increased risk of infection with M. tuberculosis.
Directly observed therapy (DOT) – adherence-enhancing strategy in which a health-care worker watches a patient swallow each dose of medication in person and documents the dose. Health-care workers providing DOT can include pharmacists, trained community health workers, etc., but cannot include the applicant’s friends or relatives. DOT is the standard of care for all applicants with tuberculosis disease. Panel physicians must provide DOT treatment to applicants or identify in-country treatment programs that follow this definition of DOT. Treatment provided outside the panel physician clinic must be evaluated in advance and closely supervised by the panel physician to ensure compliance with this definition.
Drug susceptibility test (DST) – a laboratory determination to assess whether an M. tuberculosis complex isolate is susceptible or resistant to antituberculosis drugs. The results predict whether a specific drug is likely to be effective in treating tuberculosis disease caused by that isolate.
Extensively drug-resistant tuberculosis disease (XDR TB) – is a type of multidrug-resistant tuberculosis (MDR TB) that is resistant to isoniazid, rifampin, a fluoroquinolone, and a second-line injectable (amikacin, capreomycin, and kanamycin) OR isoniazid, rifampin, a fluoroquinolone, and bedaquiline or linezolid.
Extrapulmonary tuberculosis – tuberculosis disease in any part of the body other than the lung parenchyma, pleura, intrathoracic lymph nodes or larynx. The presence of extrapulmonary disease does not exclude pulmonary tuberculosis disease.
Infectious tuberculosis disease –tuberculosis disease of the lung parenchyma, pleura, intrathoracic lymph nodes or larynx. Latent tuberculosis infection and extra-pulmonary tuberculosis are not included in this definition of infectious tuberculosis disease.
Interferon gamma release assay (IGRA) – test that measures a component of cell-mediated immunity reactivity to M. tuberculosis in fresh whole blood.
Latent tuberculosis infection (LTBI) – the presence of M. tuberculosis in the body without signs or symptoms, or radiographic or bacteriologic evidence of tuberculosis disease or extrapulmonary tuberculosis.
Laryngeal tuberculosis – tuberculosis of the larynx (voice box), a rare form of tuberculosis which is highly infectious.
Multidrug-resistant TB (MDR TB) – tuberculosis disease caused by M. tuberculosis organisms that are resistant to at least isoniazid and rifampin.
M. tuberculosis complex – includes M. tuberculosis, M. bovis, M. africanum, M. microti, M. canetti, M. caprae, M. pinnipedii, and M. orygis.
M. tuberculosis culture – a laboratory test in which the organism is grown from a submitted specimen (e.g., sputum) to determine the presence of M. tuberculosis. In the absence of cross contamination, a positive culture confirms the diagnosis of tuberculosis disease.
Pleural tuberculosis – tuberculosis disease of the membranes lining the lung, often involving fluid accumulation in the pleural space. Pleural tuberculosis is included in the definition of infectious tuberculosis disease, and is not considered extrapulmonary, because parenchymal disease is also often present and may not be apparent on chest radiograph because of compression of affected lung tissue by pleural fluid.
Pre-immigration medical screening – the medical evaluation required for all applicants.
Pulmonary tuberculosis – tuberculosis disease that involves the lung parenchyma and is often infectious (i.e., contagious [determined by sputum smear examination for acid-fast bacilli (AFB) and mycobacterial culture]).
Successfully completed tuberculosis disease therapy – directly observed therapy for tuberculosis disease taken for the full duration of therapy, including the total number of recommended doses within the time specified in CDC guidance (for example, for drug-susceptible disease see Treatment for TB Disease), with negative sputum smears and cultures at completion.
Tuberculosis disease – disease caused by infection with a member of the M. tuberculosis complex that has progressed to causing clinical (manifesting symptoms or signs) or subclinical (early stage in which signs or symptoms are not present, but other indications of disease activity are present) illness.