Developing a Framework for Assessing and Managing Individual-Level Risk of Coronavirus Disease 2019 (COVID-19) Exposure in Mobile Populations
Updated October 29, 2021
Purpose
To provide a framework of considerations for ministries of health and their partners to use while designing and implementing travel-related intervention strategies. The recommendations are based on individual-level risk assessment of potential infection of arriving travelers to mitigate the geographic spread of coronavirus disease 2019 (COVID-19). This framework focuses on public health measures to mitigate risks of COVID-19 spread among those crossing international borders and for communities through which they travel; it serves as a discussion guide to begin country-specific conversations for assessing risk of exposure and categorizing levels of monitoring and movement to establish approaches commensurate with resources and policies. This document is not intended for risk assessment and management of persons traveling into and within the United States.
Background
When outbreaks occur in areas with highly mobile populations and porous borders, the risk of further spread within an outbreak area or to other locations with a connection to an outbreak area (e.g., neighboring country, countries with flight connections) is high. The complex movement patterns in border communities and among mobile populations present challenges for identifying infected or exposed travelers and facilitating appropriate public health management strategies. Additionally, limitations in public health surveillance at points of entry contribute further challenges.1
Recognizing that neighboring countries may be in different phases of the COVID-19 pandemic and have different strategies for preparedness and response, it is important that the comprehensive border health measures countries implement have “full respect for the dignity, human rights, and fundamental freedoms of persons” [International Health Regulations, Article 3]2 while mitigating further international spread.
Objectives
The objectives of this framework are to:
- Describe methods to assess the individual-level risk of COVID-19 exposure and potential infection among mobile populations based on symptoms, travel, exposure, and diagnosis history
- Describe appropriate risk-mitigation strategies for mobile populations that are suitable for country resources
- Provide approaches to reduce risk of COVID-19 spread consistent with identified individual-level risk assessment results and associated risk-mitigation intervention levels
Methodology
This framework contains two parts. Part 1 addresses the first two objectives and Part 2 addresses the third objective. Before initiating discussions related to Parts 1 and 2, ministries of health and their partners should gather information about the country’s legal framework, including legal authorities for isolation* and quarantine** of nationals and non-nationals, regional guidance and legal frameworks for border control measures, and available resources for public health interventions and communications.
Part 1
This framework describes methods to assign a risk-mitigation intervention level, e.g., none, minimal, intermediate, or high, based on an individual-level risk assessment. Topics in this part include applying information about existing symptoms consistent with COVID-19, travel history of being in an outbreak area with ongoing community transmission, exposure history to suspected or confirmed cases, and diagnosis history including test results.
Part 2
This framework features approaches to respond to the assigned risk-mitigation intervention level, considering country-level resources. Approaches are ordered in scale of least to most restrictive and include a range of approaches, including no intervention, self-monitoring, monitoring by the health authority, movement restrictions (including voluntary or mandatory quarantine at a residence or a government approved-location) for asymptomatic persons with known or potential exposure, to isolation (at a residence or in a healthcare facility) for symptomatic persons with suspected or confirmed infection. The selection of appropriate approaches in the framework should be guided by public health system capabilities and infrastructure and current outbreak status. Approaches outlined in this section may be incorporated into existing national-level guidance on contact tracing and monitoring of individuals who may have been exposed to COVID-19.
Limitations
Countries may not have established policies or regulatory authority to impose mandatory quarantine or isolation, and may have varying levels of resources to devote to monitoring or restricting movement of infected or exposed individuals across preparedness and response phases. This document does not recommend the same approaches for all countries and serves as a discussion guide to begin country-specific conversations. Ministry of health discussions will inform refinements to the approaches used for monitoring and movement restrictions of exposed persons and persons with suspected or confirmed infection throughout the pandemic.
*Isolation is the separation of people known or suspected to be infected with a communicable disease and potentially infectious from those who are uninfected to prevent spread of the disease.
**Quarantine is the separation of those known or suspected to be exposed to a communicable disease from those who are not exposed for the purpose of monitoring and to facilitate rapid isolation if they are identified as being infected.
Part 1: Assigning risk level based on individual-level risk assessment
Application: Public health leadership can use the information below as a guide for developing procedures for applying information about individual-level risk, based on travel or exposure history, presence of symptoms, and results of any medical evaluation or diagnostic testing, to identify the appropriate risk-mitigation intervention level. Risk levels described below refer to the previous 14 days.* After developing context-specific procedures, public health leadership can use Part 2 to guide considerations for mitigation strategy approaches.
- Lower risk
- History of being in an area with no ongoing community transmission
- Negative molecular (RT-PCR) or antigen test for SARS-CoV-2 (the virus that causes COVID-19) within a timeframe before departure defined by the receiving country or upon arrival3 and individual meets no other criteria in other risk categories
- Intermediate risk
- History of being in an area with ongoing community transmission**
- History of attending a mass gathering or large social gathering such as a wedding
- Consideration: Individual level risk level may vary if the individual and other participants fully practiced personal protective measures (e.g., social distancing; use of facemasks; handwashing)
- Higher risk
- A close contact7 of a person with confirmed COVID-19,
- Risk level can be further assessed by investigating whether the infected person and close contact consistently wore face masks or took other recommended precautions during exposure period
- Additional factors to consider when defining close contact include proximity (closer distance likely increases exposure risk), duration of exposure (longer exposure time likely increases exposure risk), whether the infected individual was symptomatic (the period of onset of symptoms is associated with the highest level of viral shedding), if the infected person was likely to generate respirator aerosols (e.g. through coughing, singing, shouting), and other environmental factors (e.g. crowding, adequacy of ventilation, indoor or outdoor exposure)
- Suspected or confirmed cases
- A close contact7 of a person with confirmed COVID-19,
* Definitions of lower and higher risk activities in this document differ from CDC guidance for U.S. settings.10
**WHO defines community transmission as: Countries/territories/areas experiencing large outbreaks of local transmission defined through an assessment of factors including, but not limited to: Large numbers of cases not linkable to transmission chains. Large number of cases from sentinel lab surveillance or increasing positive cases through sentinel samples, multiple unrelated clusters in several areas of the country/territory/area.11 Refer to WHO (https://who.sprinklr.com/) or national data for latest outbreak information and affected areas.
Part 2: Tailoring a risk mitigation strategy to assigned risk levels
Instructions for use: Using the results from Part 1 and the information provided in Part 2, identify monitoring and movement approaches to mitigate risk of COVID-19 spread among and by mobile populations. This Part provides considerations for designing approaches that include no specific monitoring or movement actions, self-monitoring, monitoring by a health authority, and movement restrictions, including isolation and quarantine. The approaches are considerations, and should be adapted based on the country’s resources, public health system, legal framework, and other contextual factors. Public health leadership should review and consider the design of selected approaches throughout the stages of COVID-19 preparedness and response. Regardless of travel or exposure history, if an individual becomes symptomatic, he or she should isolate and seek a medical consult.
Information in Part 2 applies to a general population. Please refer to Annex 1 for considerations unique to critical infrastructure workers who cross borders during the course of their duties, including truckers who transport goods across international borders.
Considerations: The risk mitigation strategies outlined in Table 1 may require the following critical capacities to allow for effective implementation:
Surveillance
- Ability to detect and confirm cases of COVID-19 through public health surveillance in communities, health care facilities, and points of entry and the capacity to diagnosis disease
Contact Tracing
- Ability to identify and locate close contacts of an infected person in a timely manner to notify them of exposure, assess them for signs and symptoms of illness, and take other measures as needed to prevent further spread of disease
Monitoring
- Ability to monitor potentially exposed individuals for the duration of the incubation period to determine if they become symptomatic
Legal framework
- A legal framework that allows for public health actions listed in the risk mitigation strategy, including monitoring of exposed people and movement restrictions such as preventing travel by exposed or symptomatic people, isolation of symptomatic people, and quarantine of exposed people
Travel restrictions
- A system to prevent further travel if indicated, including a mechanism to remove travel restrictions when the restrictions are no longer needed
Quarantine
- Capacity to keep persons who might have been exposed to the virus away from others. Capacity to quarantine persons known or suspected to have been exposed including ensuring access to food and lodging and, if severe disease develops, to safely move ill persons to a medical facility for isolation
Isolation
- Capacity to keep persons who are infected with the virus away from others, whether or not they have symptoms. Capacity to isolate or to monitor self-isolation including ensuring access to food, and if severe disease develops, to safely move those in self-isolation to a medical facility
Coordination with healthcare facilities
- Ability to communicate rapidly with health care facilities to ensure they are prepared to receive ill persons and quickly obtain diagnoses
In addition to the above critical capacities, existence of the following additional capacities will ensure a more robust and coordinated monitoring and movement system is implemented.
Lab testing
- Ability to rapidly collect and transfer specimens, including specimens collected at points of entry and along travel routes, to a diagnostic facility and quickly obtain diagnoses12
Coordination with neighboring countries and regional partners
- Ability to communicate rapidly with neighboring countries and regional partners to share the developed intervention framework and positive test results of cross-border travelers13,14
Collaboration
- Ability to work in collaboration with neighboring countries to carry out cross-border contact tracing
- Engagement of other non-health ministries (e.g., Ministry of Interior or Foreign Affairs) to support implementation of interventions
- Engagement with non-government organizations to support compliance with interventions, e.g., not allowing employees to work while sick15
Understanding that countries and multinational regions may have varying agreements on or capacity for the requirements, it is important each country adapt the approaches to its own context. For example, a country may not have a legal framework in place for mandatory quarantine, but health authorities can still encourage adherence with recommendations of self-quarantine or monitoring. Further, having discussions with exposed people regarding their needs may help build trust in implementing the movement and monitoring approaches described below.
Monitoring Approaches
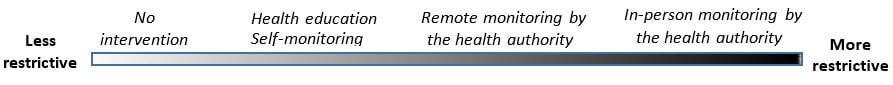
Risk mitigation level (moving from lower-level intervention on the left to higher-level intervention on the right)
Table 1. Potential approaches to use of monitoring across risk-mitigation levels
Risk-mitigation level:
No intervention
Risk-mitigation level:
No intervention
Risk-mitigation level:
Lower intervention
Risk-mitigation level:
Lower intervention
Risk-mitigation level:
Intermediate intervention
Risk-mitigation level:
Intermediate intervention
Risk-mitigation level:
Higher intervention
Risk-mitigation level:
Higher intervention
- No recommendation or requirement for monitoring
- No recommendation or requirement for monitoring
- Providing health information at points of entry, including symptoms of COVID-19 and what to do if they begin to experience any symptoms of COVID-19 (i.e., contact the health authority, health care facility, or partner organization [as directed by the health authority] for further guidance)
- Recommendation that travelers self-monitor for symptoms of COVID-19 for a specified period of time
- Providing health information at points of entry, including symptoms of COVID-19 and what to do if they begin to experience any symptoms of COVID-19 (i.e., contact the health authority, health care facility, or partner organization [as directed by the health authority] for further guidance)
- Recommendation that travelers self-monitor for symptoms of COVID-19 for a specified period of time
- Requirement for remote monitoring in countries that meet the critical capacities listed in Part 2
- Remote monitoring may be accomplished through regularly scheduled follow-ups via phone call, text message/WhatsApp, mobile apps, or other methods of communication to assess for the presence of COVID-19 symptoms
- Requirement for remote monitoring in countries that meet the critical capacities listed in Part 2
- Remote monitoring may be accomplished through regularly scheduled follow-ups via phone call, text message/WhatsApp, mobile apps, or other methods of communication to assess for the presence of COVID-19 symptoms
- Requirement for in-person monitoring in countries that meet the critical capacities listed in Part 2
- In-person monitoring may take place at the individual’s lodging if self-isolating or quarantining at the lodging, or at designated locations, such as a mandatory quarantine site, health department, or way stations, along predetermined travel routes. If in-person monitoring is planned, procedures must be in place to protect health workers conducting the monitoring from exposure
- Requirement for in-person monitoring in countries that meet the critical capacities listed in Part 2
- In-person monitoring may take place at the individual’s lodging if self-isolating or quarantining at the lodging, or at designated locations, such as a mandatory quarantine site, health department, or way stations, along predetermined travel routes. If in-person monitoring is planned, procedures must be in place to protect health workers conducting the monitoring from exposure
Movement Restriction Approaches
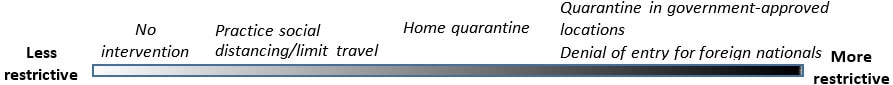
Risk mitigation level (moving from lower-level intervention on the left to higher-level intervention on the right)
Table 2. Potential approaches to use of movement restrictions across risk-mitigation levels
Risk-mitigation level:
No intervention
Risk-mitigation level:
No intervention
Risk-mitigation level:
Lower intervention
Risk-mitigation level:
Lower intervention
Risk-mitigation level:
Intermediate intervention
Risk-mitigation level:
Intermediate intervention
Risk-mitigation level:
Higher intervention
Risk-mitigation level:
Higher intervention
- No recommendation or requirements to restrict movement
- No recommendation or requirements to restrict movement
- Recommendation for social distancing, or limiting time spent in public places or traveling. For example, recommendation to only leave lodging to gather essentials or seek medical care for the duration of the potential incubation period or time in country
- Recommendation for social distancing, or limiting time spent in public places or traveling. For example, recommendation to only leave lodging to gather essentials or seek medical care for the duration of the potential incubation period or time in country
- Requirement for home quarantine or exclusion from public places (e.g., markets), congregate gatherings (e.g., stadiums), workplaces, or from local public conveyances (e.g., buses, taxis transporting other passengers, etc.) for the duration of the potential incubation period or time in country.
- Requirement for home quarantine or exclusion from public places (e.g., markets), congregate gatherings (e.g., stadiums), workplaces, or from local public conveyances (e.g., buses, taxis transporting other passengers, etc.) for the duration of the potential incubation period or time in country.
- Requirement for mandatory quarantine in government-approved locations.
- If mandatory quarantine is instituted, governments must identify mechanisms to ensure quarantined individuals have access to food, water, and sanitation and hygiene products and services
- For foreign nationals, denial of entry as long as denial does not put others at risk, e.g. requiring the individual to depart the country by plane
- Requirement for mandatory quarantine in government-approved locations.
- If mandatory quarantine is instituted, governments must identify mechanisms to ensure quarantined individuals have access to food, water, and sanitation and hygiene products and services
- For foreign nationals, denial of entry as long as denial does not put others at risk, e.g. requiring the individual to depart the country by plane
Annex 1. Considerations for critical infrastructure workers whose work involves travel
Among mobile populations is a sub-population of critical infrastructure workers who cross international borders to complete their job responsibilities. They are members of key industries whose continued operations are necessary to allow for continuity of services and movement of essential goods.16 To ensure these industries can continue functioning during the COVID-19 pandemic, it is important that workers within these industries who must cross borders for work be allowed to do so without undue burden. The critical infrastructure workforce may include, but is not limited to, transport, health, public health, and food and agriculture workers; it is the responsibility of the government to define which sectors are critical and the types of workers within each sector who are deemed essential.
To facilitate the continued movement of the critical infrastructure workforce, the country’s approach to monitoring and use of movement restrictions may need to be adapted for these workers. Examples of some strategies are provided below.
- Monitoring
- Link workers with public health authorities for remote monitoring via a phone application or SMS system for daily reporting while in country
- Conduct in-person monitoring at interval sites along approved routes, e.g., at truck weigh stations or designated trucker lodgings
- Require a negative RT-PCR or antigen test for SARS-CoV-2 before allowing entry to the country
- Establish multi-country regional surveillance systems for critical infrastructure workers who cross borders to allow for rapid notification of positive test results and facilitate contact tracing
- Movement
- Identify specific routes, stops along the route, and lodgings that workers are allowed to use
- For those staying within the border region, allow entrance to the country only for the hours of work and travel only to/from the worksite
- Offload trucks from other countries at the POE then load contents onto a local truck for transport into the country (this approach may not be suitable for all types of cargo)
Engagement of critical infrastructure partners by the government is an additional key step in order to facilitate communications and provide guidance on employer and employee responsibilities. Establishing clear expectations for these partners, as well as reliable mechanisms to receive notifications from employers (e.g., if a worker who has crossed the border tests positive or is identified as exposed), allows the government to focus on other important areas of the response.
Annex Table 1: Responsibilities of critical infrastructure employers and employees during the COVID-19 pandemic
Employer
Employer
Employee
Employee
Preparedness
Preparedness
- Develop and implement COVID-19 plans, policies, and procedures
- Train employees on policies and procedures
- Develop and implement COVID-19 plans, policies, and procedures
- Train employees on policies and procedures
- Attend trainings as directed by employer
- Attend trainings as directed by employer
Worker safety/surveillance
Worker safety/surveillance
- Develop, update and implement occupational health and safety guidance
- Develop protocols for a risk-based approach for testing of employees
- Maintain contact with staff to ensure they are monitoring their health
- Establish mechanisms to receive notifications from staff who become sick or are exposed to a person with COVID-19
- Develop and implement procedures for managing staff who become sick while working
- Screen staff for symptoms of COVID-19 before they begin work, as possible
- Ensure ill staff do not report to work until they meet public health criteria in the country for discontinuing isolation
- Develop, update and implement occupational health and safety guidance
- Develop protocols for a risk-based approach for testing of employees
- Maintain contact with staff to ensure they are monitoring their health
- Establish mechanisms to receive notifications from staff who become sick or are exposed to a person with COVID-19
- Develop and implement procedures for managing staff who become sick while working
- Screen staff for symptoms of COVID-19 before they begin work, as possible
- Ensure ill staff do not report to work until they meet public health criteria in the country for discontinuing isolation
- Follow company guidance and procedures
- Adhere to company protocols for testing
- Self-monitor for symptoms of COVID-19
- Do not report to work and notify employer if you:
- Wash hands often and wear face masks in public
- Maintain a distance of at least 2 meters from others to the extent possible
- Minimize contact with others, e.g., at POE, during stops (e.g., food, sleep, way stations) during loading and unloading
- Follow company guidance and procedures
- Adhere to company protocols for testing
- Self-monitor for symptoms of COVID-19
- Do not report to work and notify employer if you:
- Wash hands often and wear face masks in public
- Maintain a distance of at least 2 meters from others to the extent possible
- Minimize contact with others, e.g., at POE, during stops (e.g., food, sleep, way stations) during loading and unloading
Cleaning and disinfection
Cleaning and disinfection
- Clean and disinfect conveyances and other equipment or surfaces regularly
- Provide cleaning supplies and recommended personal protective equipment (e.g., gloves) for staff to clean and disinfect conveyances, surfaces, and equipment as needed
- Train staff on safe procedures to clean and disinfect conveyances and other equipment and surfaces
- Clean and disinfect conveyances and other equipment or surfaces regularly
- Provide cleaning supplies and recommended personal protective equipment (e.g., gloves) for staff to clean and disinfect conveyances, surfaces, and equipment as needed
- Train staff on safe procedures to clean and disinfect conveyances and other equipment and surfaces
- Clean and disinfect conveyances and other equipment or surfaces regularly
- Clean and disinfect conveyances and other equipment or surfaces regularly
Risk communication
Risk communication
- Communicate company policies to employees
- Educate staff on COVID-19 and how to minimize risk of getting sick
- Communicate company policies to employees
- Educate staff on COVID-19 and how to minimize risk of getting sick
The following may be useful to ministries of health and their partners in further developing their frameworks to implement intervention levels and risk mitigation approaches introduced in this document.
- Centers for Disease Control and Prevention Considerations for health screening for COVID-19 at points of entry
- World Health Organization International Health Regulations (2005) third edition
- Centers for Disease Control and Prevention (under development) Testing for SARS-CoV-2 infection at points of entry to limit international spread of COVID-19: utility and potential alternatives
- Centers for Disease Control and Prevention If you are sick or caring for someone
- Centers for Disease Control and Prevention How to protect yourself and others
- World Health Organization Coronavirus disease (COVID-19) advice for the public
- Centers for Disease Control and Prevention Contact tracing for COVID-19
- Centers for Disease Control and Prevention Discontinuation of transmission-based precautions and disposition of patients with COVID-19 in healthcare settings (interim guidance)
- Centers for Disease Control and Prevention Discontinuation of isolation for persons with COVID-19 not in healthcare settings
- Centers for Disease Control and Prevention International Travel to and from the United States
- World Health Organization Public health surveillance for COVID-19: interim guidance
- World Health Organization Regional Office for Africa Harmonized strategy for POE surveillance, laboratory testing, and transnational response to COVID-19 for cross border truck drivers [1 MB, 12 pages]
- World Health Organization Regional Office for Africa Framework on COVID-19 information sharing within East and Southern Africa (ESA) [664 KB, 5 pages]
- World Health Organization Handbook for public health capacity-building at ground crossings and cross-border collaboration
- World Health Organization Regional Office for Africa Harmonized sub-regional essential prevention and control services (IPC) at points of entry and within-country IPC interventions for transnational truck drivers within East and Southern Africa [426 KB, 8 pages]
- Department of Homeland Security Guidance on the essential critical infrastructure workforce: ensuring community and national resilience on COVID-19 response [809 KB, 19 pages]
- Centers for Disease Control and Prevention Symptoms of Coronavirus
- World Health Organization Coronavirus