Division of HIV Prevention (DHP) Strategic Plan 2017 – 2020
The Division of HIV/AIDS Prevention’s (DHAP) Strategic Plan 2017-2020 [PDF – 546 KB] (the Plan) is DHAP’s blueprint for achieving its vision of a future free of HIV. The Plan reflects the Division’s response to new opportunities for HIV prevention created by critical shifts in prevention science as well as in the national, state, and local economic and policy environments. It continues DHAP’s commitment using scalable, cost-effective interventions with demonstrated potential to reduce new infections, in the right populations for high impact prevention. The Plan encompasses the strategic aspects of the Division’s work and will continue to serve as an internal practical guide to ensure DHAP activities and resources are aligned with its priorities.
The Division of HIV/AIDS Prevention (DHAP) is pleased to present its updated Strategic Plan 2017–2020. This Plan is DHAP’s blueprint for achieving its vision of a future free of HIV. The Plan encompasses the strategic aspects of the Division’s work and will continue to serve as a practical guide to inform the work and to ensure DHAP activities and resources are aligned with its priorities.
The Plan was updated to reflect the important advances made in prevention science, including—but not limited to—the discovery of and increased use of pre-exposure prophylaxis (PrEP) as a highly effective tool in HIV prevention; the identification of new interventions as part of the High-Impact HIV prevention approach; the development and implementation of new testing technologies; and focused efforts to improve outcomes along the HIV care continuum. The Plan emphasizes maximizing DHAP’s impact, increasing internal and external coordination and collaboration, and ensuring strategic allocation of resources. In this Plan, the Division also recognizes the need to remain flexible as prevention science continues to evolve.
At the start of the strategic planning process, the Division updated the following high-level prevention goals designed to guide its HIV prevention efforts:
- Prevent new HIV infections
- Improve health outcomes for persons living with HIV
- Reduce HIV-related disparities and health inequities
- Continually improve effectiveness and efficiency of operations
These goals align with national HIV prevention goals. In addition, the Division identified key objectives and strategies to help in focusing its work on strategic efforts needed to advance these goals and to attain a future free of HIV.
In developing these goals, objectives, and strategies, DHAP acknowledges that a range of social, economic, and demographic factors make some Americans more vulnerable to HIV infection and, once infected, to inadequate care. The Plan underscores the important role of partnerships in both reducing HIV incidence and addressing these disparities that persist among populations and within communities.
To chart progress towards reaching these goals, DHAP has developed quantitative indicators that are ambitious, yet feasible. Tracking these indicators will provide the Division with important data to inform its planning and program activities, inspiring action in areas where improvement is needed. The Division will continue to strive, working closely with its partners, to better use the data available at local, state, and national levels to drive its actions, to inform priority setting, and to direct programmatic and scientific endeavors. DHAP looks forward to collaborating with federal, state, and local organizations to achieve the goals in this plan and mark progress towards a future free of HIV.
Vision and Mission
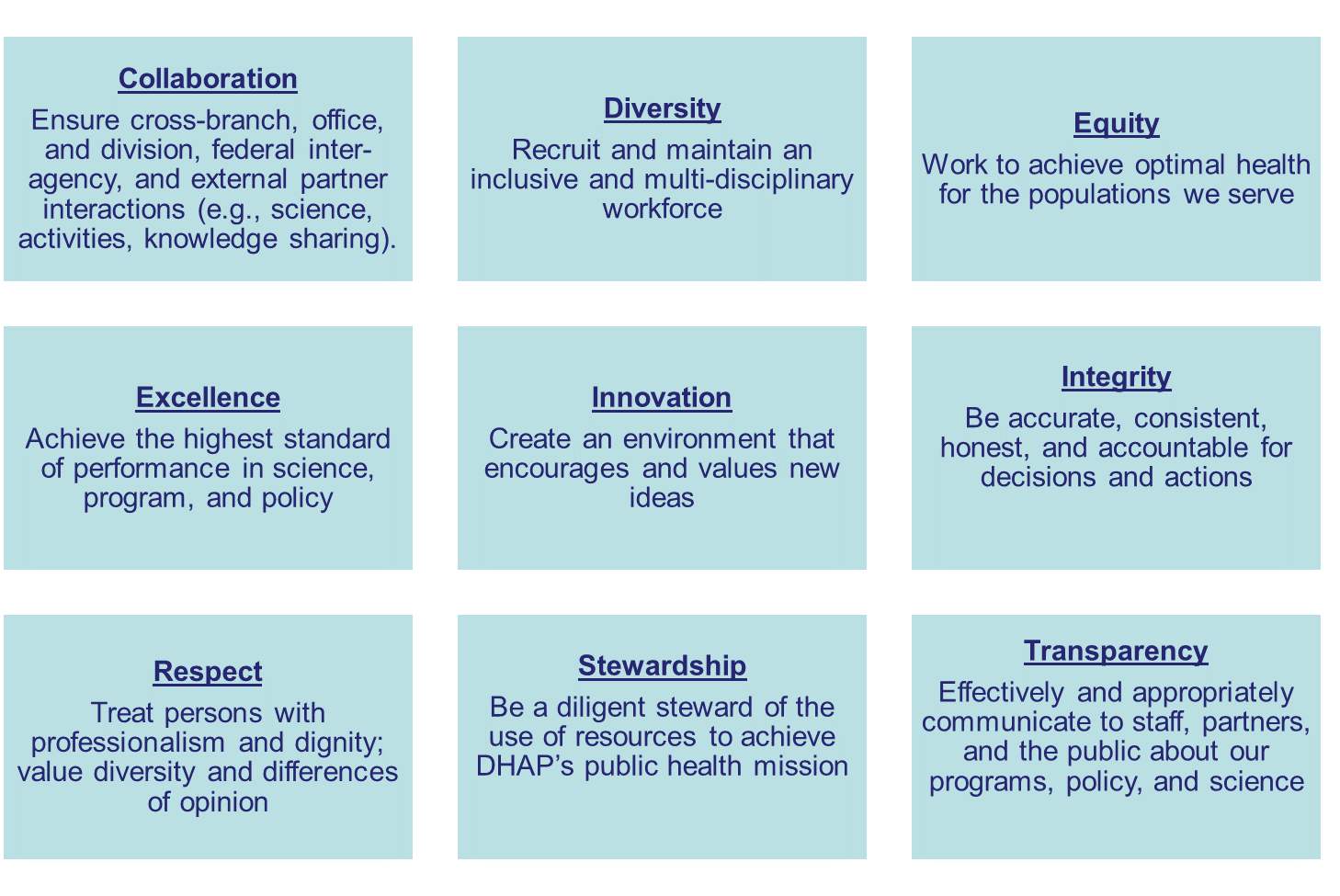
Core Values
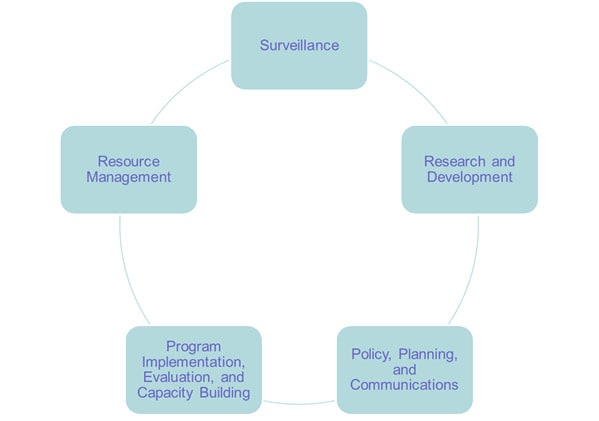
Core Functions
Core functions are essential, foundational activities that DHAP engages in to monitor the trends in HIV; implement and evaluate prevention programs; communicate priorities, information, and guidance to stakeholders and external partners; and support efficiency in the management and operations of the Division. DHAP core functions are as follows:
Over the past 5 years, advances in HIV testing services—such as delivery of couples’ counseling and testing for gay, bisexual, and other men who have sex with men (MSM); increased routine screening in clinical settings; and promotion of repeat testing for persons at ongoing risk for infection—have been associated with increased uptake of testing in the United States (CDC, 2013). From 2008 to 2014, the proportion of persons with undiagnosed HIV infection decreased by an estimated 3.4% per year. In 2014, 15% of persons living with HIV (PLWH) did not know they were infected. CDC will continue to prioritize identifying all PLWH who do not know they are infected and ensuring that persons at high risk of acquiring HIV have the biomedical and behavioral tools they need to protect themselves from acquiring HIV infection.
The estimated annual HIV infections in the United States declined 18% from 2008 to 2014, in large part because of federal HIV prevention and care efforts. CDC will continue this work to increase provision and uptake of comprehensive HIV prevention services, including high-impact behavioral and biomedical interventions, for all Americans and with a particular focus on persons at high risk of acquiring HIV. CDC will also provide resources to health care providers to facilitate access to these critical prevention tools. CDC will continue to develop communication campaigns and partnerships to ensure that everyone knows the facts about acquisition and transmission of HIV, is aware of their HIV status, and has access to tailored information and HIV prevention interventions to protect themselves and their partners. CDC will also continue to conduct research on, and implementation of, highly effective behavioral interventions.
To work towards achieving the goal of preventing new HIV infections, DHAP will prioritize the following primary prevention efforts:
- Diagnosing HIV infections by making HIV testing easy, accessible, and routine, including increasing adherence to 2006 HIV screening recommendations.
- Increasing knowledge of, use of, support for, and adherence to PrEP and nPEP for persons who could benefit from these regimens.
- Working to prevent HIV infections in communities experiencing increased injection drug use and related risk of HIV transmission.
- Ensuring persons have access to condoms and effective behavioral interventions, so they have the tools needed to protect themselves from becoming infected with HIV.
- Increasing awareness of HIV, reducing HIV-related stigma, and promoting HIV testing and proven HIV prevention strategies through key communication campaigns and messaging among populations most affected by HIV.
- Conducting research designed to identify innovative, cost-effective, and high-impact prevention strategies needed to protect persons most at risk of HIV infection.
Goal 1 and its corresponding objectives and strategies will help ensure that all PLWH know their status and that those persons at high risk of acquiring HIV have access to the key risk-reduction tools that they need to stay healthy.
Since 2003, reducing the transmission of HIV and improving health outcomes for PLWH has been a cornerstone of DHAP’s prevention efforts. A growing body of evidence shows that the majority of HIV infections in the United States could be averted by increasing the percentage of PLWH whose infection has been detected and diagnosed and by ensuring they receive early, ongoing care and treatment to become virally suppressed. Specifically, persons who had undiagnosed HIV infection and persons with diagnosed HIV but not retained in medical care were responsible for 91.5% of the estimated 45,000 HIV transmissions in 2009(Skarbinski et al., 2015).
Early linkage to care and treatment, especially when viral suppression is attained and sustained, is positively correlated with better health outcomes, thus helping PLWH live longer, healthier lives and lowering their risk of transmission of HIV to others. In the United States, the percentage of persons with newly diagnosed HIV infection who were linked to medical care within one month of diagnosis increased to 75% in 2015 (up from 70.2% in 2010). Viral suppression rates are improving. In 2014, 57.9% of persons with diagnosed HIV infection were virally suppressed (up from 46.0% in 2010). The viral suppression rates for persons in medical care are higher. The annual rate of deaths per 1,000 persons living with diagnosed HIV infection has decreased from 19.4 in 2010 to 15.2 in 2014.
To work towards achieving the goal of improving health outcomes for PLWH, DHAP will prioritize the following prevention efforts:
- Working with health departments and community-based organizations (CBOs) to improve linkages to care and increase viral suppression rates in communities most affected by HIV.
- Examining new approaches, including studies of clinical, behavioral and structural interventions, to help persons with HIV stay in care and adhere to their medications.
- Developing guidelines and launching educational campaigns to help health care providers better support HIV testing, care, treatment, and prevention.
- Working with states to improve the completeness of their laboratory data and reporting of viral suppression information.
- Advancing efforts to use state and local public health information to identify persons living with HIV who have fallen out of HIV medical care and work to link, engage, re-engage, and retain them in care.
- Expanding Data to Care programs, targeting persons who have fallen out of care or never entered care following an HIV diagnosis, and working to improve viral suppression among those with a diagnosis of HIV infection.
- Expanding experience and developing guidance on investigating and intervening in growing clusters of HIV infection.
- Expanding capacity to collect and analyze molecular data to all jurisdictions.
Goal 2 and its corresponding objectives and strategies will help in assuring that all persons with diagnosed HIV are rapidly linked to, and remain engaged in, care to improve HIV-related health outcomes, to reduce the impact of related comorbidities, and to reduce transmission of HIV to uninfected persons. DHAP will also work closely with partners to ensure public health staff and providers are working together to achieve viral suppression goals and to ensure PLWH are protected from other infectious comorbidities.
Despite intensive prevention efforts, DHAP’s HIV surveillance data show that certain populations and geographical areas in the United States continue to be disproportionately affected by HIV. While there are an expanding number of biomedical options for HIV prevention, certain populations will continue to be at greater risk of HIV infection, because of disparate access to and use of medical care. Because biomedical prevention options are delivered through a medical system that at risk persons may not trust, be able to access, and/or be able to afford, they might not realize the full prevention benefits of these tools. DHAP is committed to achieving health equity for all Americans affected by HIV, by reducing HIV-related disparities and health inequities.
In 2015, despite representing only 2% of the population, MSM accounted for 67% of HIV diagnoses. While annual HIV diagnoses among MSM and black MSM stabilized from 2010–2014, black MSM remain disproportionately affected by HIV compared to MSM of other races/ethnicities and diagnoses of HIV among Hispanic/Latino MSM increased. Although DHAP’s expanded and targeted testing efforts have increased the number of persons who know their HIV status, far too many young people are still unaware of their status. In 2014, the highest percentage of undiagnosed infections (44.4%) was among persons aged 13–24 years. Regarding outcomes for persons living with HIV, 57.9% of persons with diagnosed HIV were virally suppressed in 2014. However, young people (aged 13–24 years) compared to other age groups and blacks compared to other racial and ethnic groups had lower rates of viral suppression. HIV was the 8th leading cause of death for persons aged 25–34 years.
To work towards reducing HIV-related disparities and health inequities, DHAP will prioritize the following prevention efforts:
- Collecting and reporting data on HIV-related disparities;
- Developing interventions, partnerships, and communication efforts that increase capacity to effectively deliver critical services to disproportionately affected key populations.
- Addressing the social and structural factors that can influence health outcomes.
DHAP will target efforts to address HIV-related health disparities to the following populations: MSM, especially young black and Hispanic MSM; persons who inject drugs; transgender persons; and persons living in the southern United States.
Goal 3 and its corresponding objectives and strategies are designed to help DHAP in achieving its health equity goals. Success in this area is contingent upon building key partnerships with government partners, educational institutes, employment agencies, harm reduction organizations, mental health services and substance use disorder treatment, and other social service agencies that are primarily charged with addressing social and structural factors that lead to health inequities and disparities.
DHAP recognizes that ensuring the efficiency and effectiveness of its programs is more than just allocating resources and is committed to continually improving the systems and performance management practices, and to strengthening the workforce and infrastructure needed for continued success in reducing HIV infection in the United States.
To achieve the goal of continually improving effectiveness and efficiency of operations, DHAP will prioritize the following efforts:
- Maximizing the efficiency and effectiveness of its processes.
- Creating a work environment that ensures a skilled and motivated workforce.
- Promoting employee satisfaction, growth, and retention.
- Continuing to implement strategies to effectively recruit, employ, and promote qualified members of the workforce for DHAP positions that reflect the populations most affected by HIV.
Goal 4 and its corresponding objectives and strategies are designed to make sure that the DHAP workforce is trained and empowered to best address urgent threats to the public’s health and to ensure DHAP administrative and management processes maximize the effectiveness and impact of the Division.
Appendix 1: Key Indicators
| Goal | Objective | Indicator |
|---|---|---|
| Prevent New Infections |
|
|
| Improve Health Outcomes for Persons Living with HIV |
|
|
| Reduce HIV-related Disparities and Health Inequities |
|
|
| Continually Improve Effectiveness and Efficiency of Operations |
|
|
Appendix 2: Definitions
- Vision: A short statement of DHAP’s aspirations for the future.
- Mission: A succinct description of the fundamental purpose of the organization.
- Goals: Broadly defined outcomes.
- Objectives: The specific, measurable, achievable, and realistic results to be achieved within 5 years.
- Strategies: Plans or methods to achieve the objectives.
- Guiding Principles: Factors that guide senior leadership decision making.
- Core Functions: Key areas that represent DHAP’s essential body of work funded by the federal government to carry out its public health mission. These include the following 5 areas: Surveillance; Resource Management; Program Implementation, Evaluation, and Capacity Building; Policy, Planning, and Communications; and Research and Development.
- Core Values: Principles that guide how an organization thinks and works together, and how they serve their communities.
- Indicators: Ambitious, feasible, and measurable targets that chart progress towards successful implementation of the strategic plan and the impact of strategic plan efforts.
- Core Activities: Routine, foundational efforts necessary to maintain steady progress towards realizing DHAP’s vision.
- Strategic Activities: Prioritized, targeted efforts that are essential to accelerate progress towards achieving the specific objectives and goals laid out in the DHAP strategic plan.