
Monthy Case Studies - 2002
Case #92 - September, 2002
A patient received 9 separate units of packed red blood cells (3 times in March, 3 times in late May, and 3 times in late June). The patient developed flu-like symptoms 5 days after the last transfusion. The patient had no history of travel outside the continental United States. Thick and thin blood smears of the patient's blood were stained with Giemsa and examined. The following images show the objects seen in the blood smears. What is your diagnosis? Based on what criteria?
During the follow-up investigation, a total of 9 different blood donors were identified. Blood smears were prepared from the donated blood, stained and examined for parasites. All 9 smears were negative (no parasites found). What additional diagnostic tests would you recommend to identify the infected donor and why?
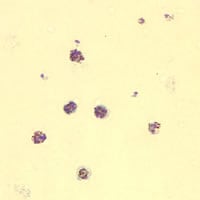
Figure A
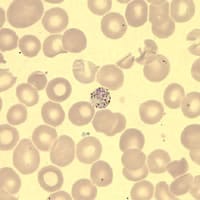
Figure B
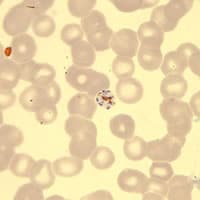
Figure C
Answer to Case #92
This was a case of transfusion-acquired malaria caused by Plasmodium malariae. Diagnostic features observed included:
- small, rounded gametocytes in less-than-normal sized red blood cells (Figures A and B).
- small, compact trophozoites with large chromatin dot (Figure A).
- ring-form trophozoites with large chromatin dots (Figure B).
- schizonts with less than 12 nuclei (merozoites) and centralized, coarse pigment (Figures A and C). Some schizonts in a rosette pattern.
Serologic tests should be performed to identify the infected donor(s). In this case, specimens from 8 of the 9 donated blood units were submitted for serologic testing. Eight units had negative serologic results for malaria; the remaining unit had antibodies to malaria. The antibody titers to all four human malaria parasites are shown below:
- P. falciparum 1:1024
- P. vivax 1:256
- P. ovale 1:256
- P. malariae >1:16384
Serological tests do not distinguish active from past infections, but they can be useful to help identify Plasmodium infected blood donors. Serology to detect the infected donor is helpful only in nonendemic areas. Cross-reactions with species other than the infecting one are not uncommon in malaria, particularly in persons who emigrated from malaria endemic areas. PCR was negative in this case. However, a negative PCR result does not alter the interpretation that this donor was infected at the time of donation.
More on: Malaria
Images presented in the monthly case studies are from specimens submitted for diagnosis or archiving. On rare occasions, clinical histories given may be partly fictitious.
 ShareCompartir
ShareCompartir


