
Monthy Case Studies - 1999
Case #17 - August, 1999
A 32-year-old woman from south Georgia developed an acute febrile illness in early July 1999 and was seen at a local hospital. Figures A through E are from Giemsa stained blood smears prepared one week after the first symptoms occurred. She had no history of international travel or of blood transfusion. What is your diagnosis? Based on what criteria?
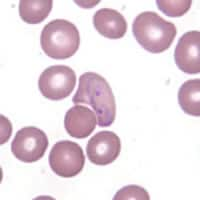
Figure A
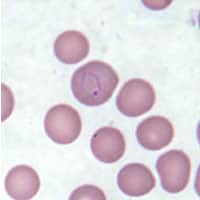
Figure B
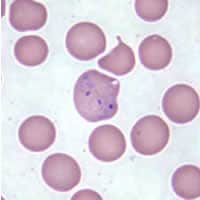
Figure C
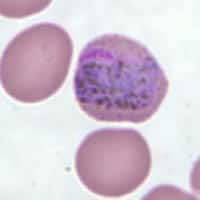
Figure D
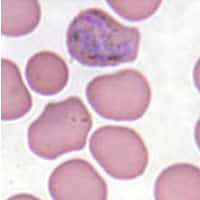
Figure E
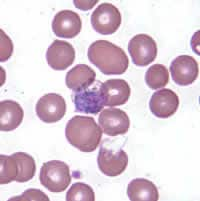
Figure F
Acknowledgement: Case and answer prepared by the Georgia Public Health Laboratory.
Answer to Case #17
This was a case of malaria casused by Plasmodium vivax. All frames in Figure A showed parasites within enlarged erythrocytes. In Figures A, C, and E, the infected erythrocytes had bizarre shapes. Schüffner's dots are visible in Figures B, D, and E. Figure B showed a late ring, and Figures A and C showed trophozoites that are very amoeboid. Figure D showed a gametocyte with numerous pigment granules throughout its cytoplasm and a deep red chromatin dot. The parasite stage in Figure E was more difficult to identify. It is most likely a gametocyte (the parasite nearly filled the erythrocyte and pigment was dispersed all over the parasite), but it might be a mature trophozoite (ameboidicity). Figure F showed a parasite in a ghost erythrocyte. It could be a schizont (chromatin material appearing to be divided into three to six masses, dark staining cytoplasm, and pigment appearing to clump).
The circumstances of the case were interesting because the patient, a native of Georgia, had no history of travel to malaria endemic areas, blood transfusion, organ transplant, or needle sharing, and no history of previous malaria. If the history is accurate, then the patient acquired her P. vivax infection through the bite of an infective mosquito. The latter could have been carried over from an endemic country, in an airplane (airport malaria), but this is unlikely because the patient lived more than 200 miles from the nearest international airport. Alternately, the infective mosquito could be a local mosquito (such as Anopheles quadrimaculatus) that became infected by feeding on a malaria-infected (gametocytemic) individual who happened to be in the area. Local summer weather conditions would have allowed the parasite to complete its sporogonic cycle in the mosquito, resulting in infective sporozoites. An investigation was conducted by the Georgia Division of Public Health and CDC, which among other things found potential breeding sites within a one-mile (1.5 km) radius of the patient's home. An example is shown in Figure A below.
Of note, the gametocytes in the patient's blood (Figure D), if picked up by local susceptible mosquitoes, will further spread the infection! This illustrates the importance of rapid diagnosis and treatment of malaria, not only to cure the patient but also to prevent reintroduction of malaria in the U.S.!

Figure A
More on: Malaria
Images presented in the monthly case studies are from specimens submitted for diagnosis or archiving. On rare occasions, clinical histories given may be partly fictitious.
 ShareCompartir
ShareCompartir


