Multistate Outbreak of Salmonella Saintpaul Infections Linked to Raw Produce
Posted August 22, 2008
Click here to go to the Final Update
This outbreak appears to be over. However, Salmonella is an important cause of human illness in the United States. More information about Salmonella, and steps people can take to reduce their risk of infection, can be found on the CDC Salmonella Web Page.
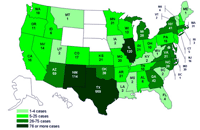
Cases infected with the outbreak strain of Salmonella Saintpaul, United States, by state
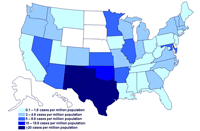
Incidence of cases of infection with the outbreak strain of Salmonella Saintpaul, United States, by state
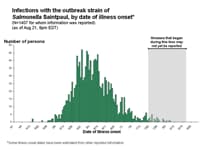
Interpretation of Epidemic Curves During an Active Outbreak
CDC is collaborating with public health officials in many states, the Indian Health Service, and the U.S. Food and Drug Administration (FDA) to investigate an ongoing multi-state outbreak of human Salmonella serotype Saintpaul infections. An initial epidemiologic investigation in New Mexico and Texas comparing foods eaten by persons who were ill in May to foods eaten by well persons identified consumption of raw tomatoes as strongly linked to illness.
A similar but much larger, nationwide study comparing persons who were ill in June to well persons found that ill persons were more likely to have recently consumed raw tomatoes, raw jalapeño peppers, and raw cilantro. These items were commonly, though not always, consumed together, so that study could not determine which item(s) caused the illnesses.
After the first case-control study was conducted, clusters of infection were detected that were associated with specific restaurants. Most clusters involve fewer than 5 ill persons. In two clusters, illnesses were linked to an item containing raw jalapeño peppers and no other of the suspect items. Detailed investigations of three other clusters indicate that jalapeño peppers do not explain all illnesses. In two of these investigations, illnesses were linked to an item containing raw serrano peppers and raw tomatoes, but not jalapeño peppers. In the third, illnesses were linked to an item that contained raw jalapeños and tomatoes.
These epidemiological studies indicate that more than one food vehicle is involved in this outbreak. No one food item can explain the entire outbreak. Although rare, there have been outbreaks in the past in which more than one food source has been implicated.
At present, information indicates that jalapeño and serrano peppers grown, harvested, or packed in Mexico are the cause of some clusters and are major food vehicles for the outbreak. The outbreak strain Salmonella Saintpaul has been isolated twice from jalapeño peppers and once from serrano peppers. These foods were sampled as the result of traceback investigations based on the epidemiologic investigations of clusters. An FDA laboratory detected the outbreak strain Salmonella Saintpaul in a sample of a jalapeño pepper obtained from a distribution center in McAllen, Texas. The distributor worked with FDA to recall the contaminated product in the United States. The peppers were grown in Mexico.
An FDA laboratory detected the outbreak strain Salmonella Saintpaul in a sample of a serrano pepper and an agricultural water sample collected on a farm in Mexico that supplied peppers to the distribution center in McAllen, Texas. Results from the FDA laboratory therefore confirm that this outbreak was caused by at least two produce items, raw jalapeño and raw serrano peppers. In addition, the Laboratory Services Division of the Colorado Department of Public Health and Environment detected the outbreak strain of Salmonella Saintpaul in a jalapeño pepper provided by an ill individual.
Since April, 1438 persons infected with Salmonella Saintpaul with the same genetic fingerprint have been identified in 43 states, the District of Columbia, and Canada. These were identified because clinical laboratories in all states send Salmonella strains from ill persons to their State public health laboratory for characterization.The number of ill persons identified in each state is as follows:Alabama (6 persons), Arkansas (21), Arizona (59), California (16), Colorado (17), Connecticut (5), Florida (4), Georgia (42), Idaho (6), Illinois (120), Indiana (21), Iowa (2), Kansas (21), Kentucky (2), Louisiana (3), Maine (1), Maryland (39), Massachusetts (31), Michigan (28), Minnesota (31), Mississippi (2), Missouri (20), Montana (1), New Hampshire (6), Nevada (14), New Jersey (16), New Mexico (114), New York (41), North Carolina (28), Ohio (10), Oklahoma (38), Oregon (11), Pennsylvania (15), Rhode Island (3), South Carolina (2), Tennessee (10), Texas (559), Utah (2), Virginia (31), Vermont (2), Washington (18), West Virginia (1), Wisconsin (13), and the District of Columbia (1). Five ill persons are reported from Canada. Four appear to have been infected while traveling in the United States; the travel status of the fifth ill person is unknown.
Among the 1407 persons with information available, illnesses began between April 16 and August 8, 2008, including 115 who became ill on July 1 or later. These numbers include those with estimated onset dates as well as those with reported onset dates. The latest reported onset date is August 8. The latest estimated onset date is August 7.
Patients range in age from < 1 to 99 years; 50% are female. The rate of illness is highest among persons 20 to 29 years old; the rate of illness is lowest in children 10 to 19 years old and in persons 80 or more years old. At least 282 persons were hospitalized. A man in his eighties who died in Texas from cardiopulmonary failure had an infection with the outbreak strain at the time of his death; the infection may have contributed to his death. A man in his sixties who died in Texas from cancer had an infection with the outbreak strain of at the time of his death; the infection may have contributed to his death.
The outbreak can be visually described with a chart showing the number of persons who became ill each day. This chart is called an epidemic curve or epi curve. Please see Interpretation of Epidemic Curves During an Active Outbreak. It shows that the number of persons who became ill peaked during May and decreased in June. The average number of persons who became ill in recent weeks continues to decrease, indicating that the outbreak is ending. See the Salmonella Outbreak Investigations: Timeline for Reporting Cases.
Only 18 persons infected with this strain of Salmonella Saintpaul were identified in the country during April through August of 2007. The previous rarity of this strain and the distribution of illnesses in all U.S. regions suggest that the implicated food is distributed throughout much of the country. Because many persons with Salmonella illness do not have a stool specimen tested, it is likely that many more illnesses have occurred than those reported. Some of these unreported illnesses may be in states that are not on today's map.
Clinical features of Salmonella Infection
Most persons infected with Salmonella develop diarrhea, fever, and abdominal cramps 12-72 hours after infection. Infection is usually diagnosed by culture of a stool sample. The illness usually lasts 4-7 days. Although most people recover without treatment, severe infections may occur. Infants, elderly persons, and those with impaired immune systems are more likely than others to develop severe illness. When severe infection occurs, Salmonella may spread from the intestines to the bloodstream and then to other body sites, and can cause death. In these severe cases, antibiotic treatment may be necessary.
Advice to consumers
FDA is advising consumers that they should avoid raw jalapeño peppers and raw serrano peppers and foods that contain them, if they were grown, harvested, or packed in Mexico. Jalapeño and serrano peppers grown in the United States are not connected with this outbreak. Commercially canned, pickled, and cooked jalapeño peppers are also not connected with the outbreak.
Consumers everywhere are advised to follow the general food safety guidelines below:
- Refrigerate within 2 hours or discard cut, peeled, or cooked produce items
- Avoid purchasing bruised or damaged produce items, and discard any that appear spoiled.
- Thoroughly wash all produce items under running water.
- Keep produce items that will be consumed raw separate from raw meats, raw seafood, and raw produce items.
- Wash cutting boards, dishes, utensils, and counter tops with hot water and soap when switching between types of food products.
Consumers are reminded that vegetables are an important part of a healthy diet and that cooking vegetables kills bacteria, including Salmonella.
FDA information on this investigation.
More information about Salmonella and this investigation can be found at:
- Salmonella FAQ
- Timeline for Reporting of Cases
- New Mexico Department of Health [PDF – 191 KB]
- Kansas Identifies 3 Cases Linked to Multi-State Salmonella Outbreak
- Kentucky Cabinet for Health and Family Services Press Release
- Indiana State Department of Health Media Update on Salmonella Outbreak
- New Jersey Department of Health and Human Services: NJ Reports Four Salmonella Cases Linked to Multi-State Outbreak
- Utah Department of Health: Health News
- Information on the safe handling of produce [PDF - 2 pages]
Previous Updates on this Outbreak
- August 20, 2008
- August 15, 2008
- August 12, 2008
- August 8, 2008
- August 6, 2008
- August 4, 2008
- August 1, 2008
- July 30, 2008
- July 29, 2008
- July 28, 2008
- July 25, 2008
- July 24, 2008
- July 23, 2008
- July 22, 2008
- July 21, 2008
- July 18, 2008
- July 17, 2008
- July 16, 2008
- July 15, 2008
- July 14, 2008
- July 11, 2008
- July 10, 2008
Get email updates
To receive email updates about this page, enter your email address:
Contact Us:
- Centers for Disease Control and Prevention
1600 Clifton Rd
Atlanta, GA 30333 - 800-CDC-INFO
(800-232-4636)
TTY: (888) 232-6348 - Contact CDC–INFO
 ShareCompartir
ShareCompartir