Multistate Outbreak of Human Salmonella Enteritidis Infections Associated with Shell Eggs
Posted August 27, 2010
Click here to go to the Final Update
This outbreak appears to be over. However, Salmonella is an important cause of human illness in the United States. More information about Salmonella, and steps people can take to reduce their risk of infection, can be found on the CDC Salmonella Web Page.
On this Page
Outbreak Highlights
- From May 1 to August 25, 2010, approximately 1,470 reported illnesses were likely to be associated with this outbreak.
- FDA testing identified Salmonella in egg farm environmental samples.
- Don’t eat recalled eggs. Recalled eggs might still be in grocery stores, restaurants, and consumers' homes. Consumers who have recalled eggs should discard them or return them to their retailer for a refund. A searchable database of products affected by the recall is available to consumers.
- Individuals who think they might have become ill from eating recalled eggs should consult their health care providers.
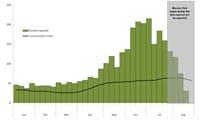
Number of Salmonella Enteritidis cases matching PFGE pattern JEGX01.0004 reported to PulseNet, United States, 2010
CDC is collaborating with public health officials in multiple states, the U.S. Food and Drug Administration (FDA), and the U.S. Department of Agriculture’s Food Safety and Inspection Service to investigate a nationwide increase of Salmonella Enteritidis (SE) infections with an indistinguishable pulsed-field gel electrophoresis (PFGE) pattern JEGX01.0004. This is the most common PFGE pattern for SE in the PulseNet database. Investigators are using DNA analysis of Salmonella bacteria obtained through diagnostic testing to identify cases of illness that may be part of this outbreak. Because the outbreak PFGE pattern (outbreak strain) commonly occurs in the U.S., some of the cases identified with this outbreak strain may not be related to this outbreak.
Investigation of the Outbreak
In early July 2010, CDC identified a nationwide sustained increase in the number of Salmonella Enteritidis isolates with PFGE pattern JEGX01.0004 uploaded to PulseNet, the national subtyping network made up of state and local public health laboratories and federal food regulatory laboratories that performs molecular surveillance of foodborne infections. This increase began in May 2010, and is evident in the epidemic curve, or epi curve. From May 1 to August 25, 2010, a total of 2,403 illnesses were reported. However, some cases from this period have not been reported yet, and some of these cases may not be related to this outbreak. Based on the previous 5 years of reports to PulseNet, we would expect approximately 933 total illnesses during this same period. This means that there are approximately 1,470 reported illnesses that are likely to be associated with this outbreak. Many states have reported increases of this pattern since May. Because of the large number of expected cases during this period, standard methods of molecular subtyping alone are not sufficient to determine which reported cases might be outbreak-associated. CDC is currently conducting testing using advanced molecular methodologies to help distinguish between outbreak-related cases and sporadic (or background) cases.
Illnesses that occurred after July 23, 2010 might not yet be reported due to the time it takes between when a person becomes ill and when the illness is reported. This takes an average of 2 to 3 weeks for Salmonella. For more details, please see the Salmonella Outbreak Investigations: Timeline for Reporting Cases.
Epidemiologic investigations conducted by public health officials in 10 states since April have identified 26 restaurants or event clusters where more than one ill person with the outbreak strain has eaten. Data from these investigations suggest that shell eggs are a likely source of infections in many of these restaurants or event clusters. Preliminary information indicates that Wright County Egg, in Galt, Iowa, was an egg supplier in 15 of these 26 restaurants or event clusters. To date, no new restaurant or event clusters have been reported to CDC. A formal traceback was conducted by state partners in California, Colorado, and Minnesota, in collaboration with FDA and CDC, to find a common source of shell eggs. Wright County Egg in Iowa was found as the common source of the shell eggs associated with three of the clusters. Through traceback and FDA investigational findings, Hillandale Farms of Iowa, Inc. was identified as another potential source of contaminated shell eggs contributing to this outbreak. FDA is currently conducting extensive investigations at both of these firms in Iowa. The investigations involve sampling, records review and looking for potential sources of contamination, such as feed.
Laboratory Testing of Environmental Samples
FDA has collected nearly 600 samples from Wright County Egg and Hillandale Farms of Iowa during this investigation. The majority of these samples are still undergoing laboratory testing and results are pending. To date, FDA's test results of six environmental samples identified Salmonella with PFGE patterns indistinguishable from the outbreak strain. These six positive samples were collected from manure, as well as traffic areas such as walkways, equipment, other surfaces in and around the farm, and from the feed mill at Wright County Egg in Iowa. The feed was provided to pullets (young female chickens or hens) raised at Wright County Egg facilities in Iowa. Pullets are distributed to all premises at Wright County Egg in Iowa and Hillandale Farms in Iowa. These findings indicate that Wright County Egg and Hillandale Farms of Iowa are the likely sources of the contaminated shell eggs. FDA has not found that this feed was distributed to any companies other than Wright County Egg and Hillandale Farms of Iowa.
Recall Information
On August 13, 2010, Wright County Egg of Galt, Iowa, conducted a nationwide voluntary recall of shell eggs. On August 18, 2010, Wright County Egg expanded its recall. On August 20, 2010, Hillandale Farms of Iowa conducted a nationwide voluntary recall of shell eggs.
Clinical Features/Signs and Symptoms
A person infected with Salmonella Enteritidis usually has fever, abdominal cramps, and diarrhea beginning 12 to 72 hours after consuming a contaminated food or beverage. The illness usually lasts 4 to 7 days, and most persons recover without antibiotic treatment. However, the diarrhea can be severe, and hospitalization may be required. The elderly, infants, and those with impaired immune systems may have a more serious illness. In these patients, the infection may spread from the intestines to the blood stream, and then to other body sites and can cause death unless the person is treated promptly with antibiotics. For more information, visit CDC’s Salmonella Enteritidis website.
Advice to Consumers
- Don’t eat recalled eggs. Recalled eggs might still be in grocery stores, restaurants, and consumers' homes. Consumers who have recalled eggs should discard them or return them to their retailer for a refund. A searchable database of products affected by the recall is available to consumers.
- Individuals who think they might have become ill from eating recalled eggs should consult their health care providers.
- Keep eggs refrigerated at ≤ 45° F (≤7° C) at all times.
- Discard cracked or dirty eggs.
- Wash hands and all food contact surface areas (counter tops, utensils, and cutting boards) with soap and water after contact with raw eggs. Then, disinfect the food contact surfaces using a sanitizing agent, such as bleach, following label instructions.
- Eggs should be cooked until both the white and the yolk are firm and eaten promptly after cooking.
- Do not keep eggs warm or at room temperature for more than 2 hours.
- Refrigerate unused or leftover egg- containing foods promptly.
- Avoid eating raw eggs.
- Individuals wishing to further reduce their risk may consider using pasteurized, in-shell eggs.
- Avoid restaurant dishes made with raw or undercooked, unpasteurized eggs. Restaurants should use pasteurized eggs in any recipe (such as Hollandaise sauce or Caesar salad dressing) that calls for raw eggs.
- Consumption of raw or undercooked eggs should be avoided, especially by young children, elderly persons, and persons with weakened immune systems or debilitating illness.
Advice to Egg Producers
- Flock-based SE-control programs that include routine microbiologic testing are mandatory for producers with more than 50,000 hens, as of July 9, 2010, under FDA's egg safety rule.
Advice to Retail and Food Service Establishments and Institutional Settings
- In retail and food service establishments, pasteurized egg products or pasteurized in-shell eggs are recommended in place of pooled eggs or raw or undercooked shell eggs. If used, raw shell eggs should be fully cooked. If shell eggs are served undercooked, a consumer advisory should be posted in accordance with the Food Code.
- In hospitals, nursing homes, adult or childcare facilities, and senior centers, pasteurized egg products or pasteurized in-shell eggs should be used in place of pooled eggs or raw or undercooked eggs.
- Eggs should be purchased or received from a distributor refrigerated and stored refrigerated at ≤ 45° F (≤7° C) at all times.
General Information
- CDC FAQs: Salmonella Enteritidis
- FoodSafety.gov
- Description of the Steps In a Foodborne Outbreak Investigation
- CDC's Role During a Multi-State Foodborne Outbreak Investigation
Additional Resources
- Shell Eggs Recall Product List
- Hillandale Farms of Iowa Conducts Nationwide Voluntary Recall of Shell Eggs Because of Possible Health Risk (August 20, 2010)
- Wright County Egg Expands Nationwide Voluntary Recall of Shell Eggs (August 18, 2010)
- Wright County Egg Conducts Nationwide Voluntary Recall of Shell Eggs Because of Possible Health Risk (August 13, 2010)
- Tips to Reduce Your Risk of Salmonella from Eggs [PODCAST – 4:00 minutes]
CDC's Role in Food Safety
As an agency within the U.S. Department of Health and Human Services (HHS), CDC leads federal efforts to gather data on foodborne illnesses, investigate foodborne illnesses and outbreaks, and monitor the effectiveness of prevention and control efforts. CDC is not a food safety regulatory agency but works closely with the food safety regulatory agencies, in particular with HHS's U.S. Food and Drug Administration (FDA) and the Food Safety and Inspection Service within the U.S. Department of Agriculture (USDA). CDC also plays a key role in building state and local health department epidemiology, laboratory, and environmental health capacity to support foodborne disease surveillance and outbreak response. Notably, CDC data can be used to help document the effectiveness of regulatory interventions.
Previous Updates
Get email updates
To receive email updates about this page, enter your email address:
Contact Us:
- Centers for Disease Control and Prevention
1600 Clifton Rd
Atlanta, GA 30333 - 800-CDC-INFO
(800-232-4636)
TTY: (888) 232-6348 - Contact CDC–INFO
 ShareCompartir
ShareCompartir