Polysubstance Use During Pregnancy
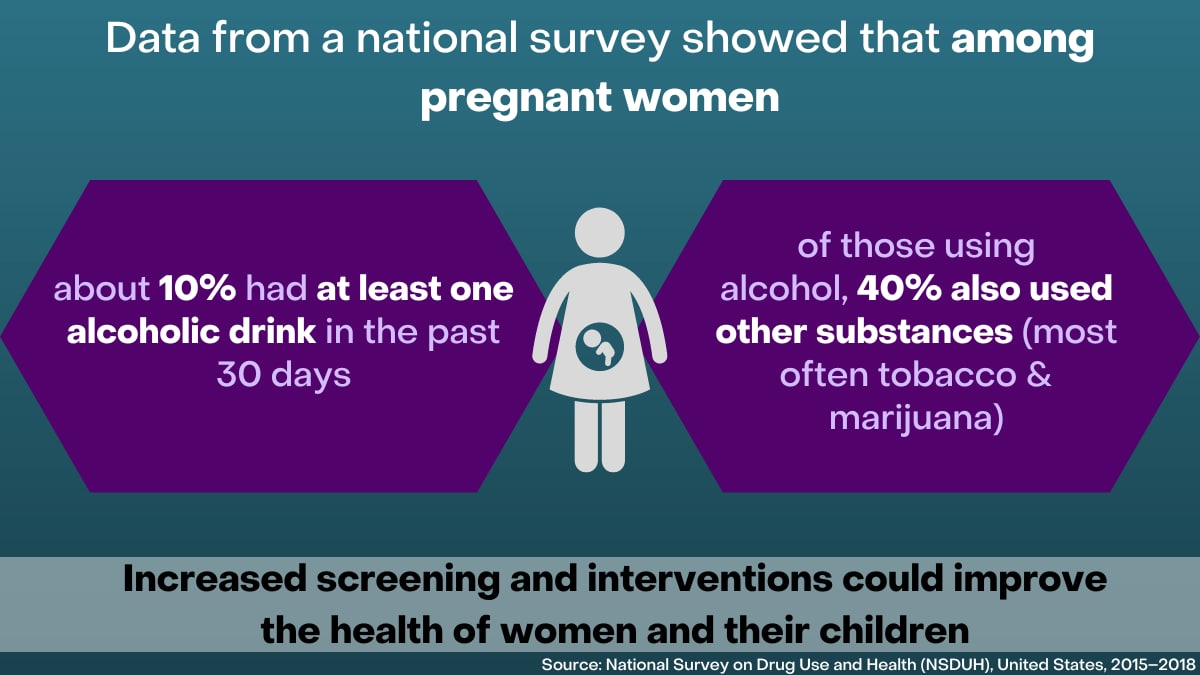
Research suggests that the use of more than one substance, also known as polysubstance use, during pregnancy is common. More research is needed to understand the possible effects from exposure to multiple substances compared to one substance during pregnancy. Increased evidence-based practices, such as screening and follow-up as appropriate, can help reduce substance exposure during pregnancy and improve the health of people who are pregnant and their children.
Substance use during pregnancy can have health effects on a pregnant person and baby

- Alcohol use during pregnancy can cause miscarriage, stillbirth, and a range of lifelong birth defects and developmental disabilities. These disabilities are known as fetal alcohol spectrum disorders (FASDs).
- Opioid use during pregnancy has been linked to poor fetal growth, preterm birth, stillbirth, specific birth defects, and neonatal abstinence syndrome (NAS) or neonatal opioid withdrawal syndrome (NOWS).
- Cigarette smoking during pregnancy increases the risk of health problems for developing babies, such as preterm birth, low birth weight, and birth defects of the mouth and lip. Smoking during and after pregnancy also increases the risk of sudden infant death syndrome (SIDS). In addition, tobacco products containing nicotine (the addictive drug found in tobacco) and e-cigarettes are not safe to use during pregnancy.
- Some research shows that marijuana use during pregnancy is linked to low birth weight. It may also increase the chances for developmental problems for a child, such as problems with attention and learning. Further research is needed to better understand how marijuana may affect pregnant people and developing babies.
- Nonmedical use of prescription medications can lead to an increased risk of adverse health outcomes and overdose. Combining substances, such as opioids with benzodiazepines or opioids with alcohol, can also increase the risk of drug overdose.
If you need help for substance use, talk with your healthcare provider. Visit FindTreatment.gov to find local resources.
Polysubstance use is common during pregnancy
Many people may use more than one substance during pregnancy. For example,
- A 2020 study found that about 10% of pregnant women reported current alcohol use, and among them, use of other substances was common—about 40% reported current use of one or more other substances.1
- A study published in 2020 found that among women who continued marijuana use before and during pregnancy, 74% also smoked cigarettes during their pregnancy.2
- A 2017 study found that more than half of pregnant women who used opioids for nonmedical reasons reported drinking more than five drinks with alcohol per day during a 1-month period of time.3
- A 2015 study found that pregnant women prescribed opioid pain medication were more likely to smoke tobacco compared to those who did not use opioids.4
Impacts of polysubstance use on infants are not well known
The effects of polysubstance use during pregnancy are not well known. Limitations to data collection can include the following:
- Data sources are often limited to self-reported information, which might be underreported because of stigma and legal implications.
- The timing of substance use during pregnancy can be difficult to determine. For example, some surveys ask about use in the past 12 months or past 30 days, so patterns across individual pregnancies are not known.
- Some respondents may not know they are pregnant at the time of a survey, which could lead to an underestimation of substance use during pregnancy.
- Studies often examine use of a single substance, but polysubstance use is not always accounted for in analyses.
More research is needed to better understand the effects of polysubstance use on people who are pregnant and their babies. This information could help explain the effects of prenatal polysubstance use compared to the effects of each individual substance.

The U.S. Preventive Services Task Force (USPSTF) makes recommendations about the effectiveness of specific clinical preventive services. These recommendations are based on the evidence of both the benefits and harms of the service. For substance use among adults, including pregnant persons, the USPSTF currently provides the following recommendations:
- Unhealthy Drug Use: Screening (2020)
- “The USPSTF recommends screening by asking questions about unhealthy drug use in adults age 18 years or older. Screening should be implemented when services for accurate diagnosis, effective treatment, and appropriate care can be offered or referred.” (Grade B)
- Applies to adults 18 years or older, including people who are pregnant or postpartum, and adolescents aged 12–17 years in primary care settings
- Unhealthy Alcohol Use: Screening and Behavioral Counseling Interventions (2018)
- “The USPSTF recommends screening for unhealthy alcohol use in primary care settings in adults 18 years or older, including pregnant women, and providing persons engaged in risky or hazardous drinking with brief behavioral counseling interventions to reduce unhealthy alcohol use.” (Grade B)
- Applies to adults 18 years or older, including people who are pregnant
- Tobacco Smoking Cessation in Adults, Including Pregnant Persons (2015)
- “The USPSTF recommends that clinicians ask all pregnant persons about tobacco use, advise them to stop using tobacco, and provide behavioral interventions for cessation to pregnant persons who use tobacco.” (Grade A)
- Applies to adults aged 18 years or older, including people who are pregnant
Healthcare provider?
Our Work
CDC’s National Center on Birth Defects and Developmental Disabilities (NCBDDD) works to address substance use during pregnancy. NCBDDD also works to improve care for affected individuals and their families. CDC does this work through the following activities:
- Collecting and analyzing data on substance exposure during pregnancy, the impact of evidence-based programs, and the occurrence of negative infant outcomes
- Implementing programs to inform policies for practice and systems change
- Working with partners to develop and implement evidence-based interventions and clinical guidelines for the care of mothers and babies
- Conducting communication activities to increase awareness and sharing new findings in a timely manner
Related Articles
Polysubstance Use in Pregnancy: Surveillance, Interventions, and Next Steps
Journal of Women’s Health 2023; DOI: 10.1089/jwh.2023.0341
Park Y, Dang EP, Board A, Gilboa SM, Ondersma SJ, Smid MC, Shakib JH, Mitchell KT, England LJ, Broussard CS, Meaney-Delman D, Iskander J, Kim SY.
[Read Summary]
Polysubstance Use During Pregnancy: The Importance of Screening, Patient Education, and Integrating a Harm Reduction Perspective
Drug and Alcohol Dependence 2023;247:109872. DOI: 10.1016/j.drugalcdep.2023.109872
Board A, D’Angelo DV, Salvesen von Essen B, Denny CH, Miele K, Dunkley J, Baillieu R, Kim SY.
[Read Article]
Systematic Review: Polysubstance Prevalence Estimates Reported during Pregnancy, US, 2009–2020
Maternal Child and Health Journal 2023; DOI: 10.1007/s10995-023-03592-w
Tran EL, England LJ, Park Y, Denny CH, Kim SY.
[Read Article]
Alcohol Use and Co-use of Other Substances Among Pregnant Females Aged 12–44 Years – United States, 2015–2018
Morbidity and Mortality Weekly Report; August 7, 2020; 69(31): 1009-1014
England LJ, Bennett C, Denny CH, Honein MA, Gilboa SM, Kim SY, Guy GP, Tran EL, Rose CE, Bohm MK, Boyle CA.
[Read Article]
More Information
- AAP: Fetal Alcohol Spectrum Disorders Program
- AAP: Substance Use and Prevention
- ACOG: Fetal Alcohol Spectrum Disorders Prevention
- ACOG: Marijuana Use During Pregnancy and Lactation
- ACOG: Opioid Use Disorder and Pregnancy
- ACOG: Tobacco and Pregnancy
- Academy of Perinatal Harm Reduction
- CDC: Alcohol Screening and Brief Intervention
- CDC: Fetal Alcohol Spectrum Disorders
- CDC: MAT-LINK
- CDC: Opioid Use During Pregnancy
- CDC: Smoking During Pregnancy
- CDC: Substance Use During Pregnancy
- CDC: What You Need to Know About Marijuana Use and Pregnancy
- March of Dimes: Beyond Labels – Substance Use and Pregnancy
- FASD United
- SAMHSA: Marijuana and Pregnancy
- SAMHSA: Opioid Use Disorder and Pregnancy
1England LJ, Bennett C, Denny CH, et al. Alcohol use and co-use of other substances among pregnant females aged 12–44 years – United States, 2015–2018. MMWR Morb Mortal Wkly Rep 2020; 69(31): 1009-1014.
2Ko JY, Coy KC, Haight SC, et al. Characteristics of marijuana use during pregnancy – eight states, Pregnancy Risk Assessment Monitoring System, 2017. MMWR Morb Mortal Wkly Rep 2020; 69(32): 1058-1063.
3Jarlenski M, Barry CL, Gollust S, et al. Polysubstance use among US women of reproductive age who use opioids for nonmedical reasons. Am J Public Health 2017; 107(8):1308–1310.
4Patrick SW, Dudley J, Martin PR, et al. Prescription opioid epidemic and infant outcomes. Pediatrics 2015;135(5):842–850.