

|

|

Volume
7: No. 1, January 2010
SPECIAL TOPIC
Simulating and Evaluating Local Interventions to Improve Cardiovascular Health
Jack Homer, PhD; Bobby Milstein, PhD, MPH; Kristina Wile, MS; Justin Trogdon, PhD; Philip Huang, MD, MPH; Darwin Labarthe, MD, MPH, PhD; Diane Orenstein, PhD
Suggested citation for this article: Homer J, Milstein B, Wile K, Trogdon J, Huang P, Labarthe D, et al. Simulating and evaluating local interventions to improve cardiovascular health. Prev Chronic Dis 2010;7(1):A18.
http://www.cdc.gov/pcd/issues/2010/
jan/08_0231.htm. Accessed [date].
PEER REVIEWED
Abstract
Numerous local interventions for cardiovascular disease are available, but resources to deliver them are limited. Identifying the most effective interventions is challenging because cardiovascular risks develop through causal pathways and gradual accumulations that defy simple calculation.
We created a simulation model for evaluating multiple approaches to preventing and managing cardiovascular risks. The model incorporates data from many sources to represent all US adults who have never had a cardiovascular event. It simulates trajectories for the leading direct and indirect risk factors from 1990 to 2040 and evaluates 19 interventions. The main outcomes are first-time cardiovascular events and consequent deaths, as well as total consequence costs, which combine medical
expenditures and productivity costs associated with cardiovascular events and risk factors. We used sensitivity analyses to examine the significance of uncertain parameters.
A base case scenario shows that population turnover and aging strongly influence the future trajectories of several risk factors. At least 15 of 19 interventions are potentially cost saving and could reduce deaths from first cardiovascular events by approximately 20% and total consequence costs by 26%. Some interventions act quickly to reduce deaths, while others more gradually reduce costs related to risk factors. Although the model is still evolving, the simulated experiments reported here can inform policy and spending decisions.
Back to top
Introduction
Conditions in particular neighborhoods or cities can profoundly enhance or impede people’s prospects for a healthy life
(1). This dependence on local context is especially evident in cardiovascular health, for which behavioral, social, and environmental factors combine to affect the likelihood of developing disease or dying prematurely
(2). Heart disease and stroke are largely preventable, but they remain the first and third leading causes of death in the United States, partly because we
have yet to establish living conditions that minimize such modifiable risks as smoking, obesity, stress, air pollution, poor diet, and physical inactivity. The importance of intervening to limit these risks is highlighted in A Public Health Action Plan to Prevent Heart Disease and Stroke (3).
The notion that cardiovascular disease (CVD) can be prevented through local actions raises practical questions that can be examined through systems modeling and simulation. Working closely with colleagues in Austin/Travis County, Texas, and subject matter experts at the Centers for Disease Control and Prevention and the National Institutes of Health, we developed a system dynamics simulation model to answer the following questions:
- How does local context affect the major risk factors for CVD and, in turn, population health status and costs?
- How might local interventions affect CVD risk, health status, and costs over time?
- How might local health leaders better balance their policy efforts given limited resources?
Back to top
Methods
System dynamics models improve our ability to anticipate the likely effects of interventions in dynamically complex situations, where the pathways from interventions to outcomes may be indirect, delayed, and possibly affected by nonlinearities or feedback loops
(4). System dynamics has been used effectively since the 1970s to model many areas of public health and social policy, including CVD
(5).
Model structure
We previously described a framework for understanding cardiovascular health in a local context
(6). That framework has been refined and quantified by using additional literature and input from veteran health planners and analysts. The resulting simulation model (Figure 1) focuses on primary prevention; it does not address people who have experienced a CVD event. Causal influences move down and to the right, ending with 2 outcomes: 1) first-time cardiovascular events and consequent
deaths and 2) costs associated with these events and with the identified risk factors.
[View
enlarged image
and descriptive text.]
Figure 1. Simulation model for cardiovascular disease (CVD)
outcomes. This diagram depicts major health conditions related to CVD and their causes. Boxes identify risk factor prevalence
rates modeled as dynamic stocks. The population flows associated with these stocks — including people entering the adult population, entering the next age category, immigration, risk factor incidence, recovery, cardiovascular event survival, and death — are not shown.
Key:
Blue solid arrows: causal linkages affecting risk factors and cardiovascular
events and deaths.
Brown dashed arrows: influences on costs.
Purple italics: factors amenable to direct intervention.
Black italics (population aging, cardiovascular event fatality): other specified trends.
Black nonitalics: all other variables, affected by italicized variables and by each other.
The model starts with conditions in the United States in 1990 and simulates them continuously through 2040. The
population without CVD and risk factor prevalence rates are represented as dynamic stock or state variables, subdivided by sex and age group (18-29 y, 30-64 y, and ≥65 y). Smoking and obesity are viewed as reversible conditions, whereas diabetes, high blood pressure, and high cholesterol are viewed as chronic
conditions that are not reversible but that can be controlled, with the help
of good-quality primary health care, to reduce CVD risk.
The incidence of first-time CVD events in the model is driven by the effect of several direct risk factors, based on a widely used risk calculator from the Framingham
Heart Study (7). We modified that calculator in several ways for this study, most fundamentally by estimating annual risks at a population level on the basis of risk factor prevalence
rates, rather than at the level of an individual. (A detailed description of the modified calculator is available at
http://sustainer.org/cvd/documents/SELI_App1.pdf). We also recognized the direct effect on CVD events, especially myocardial infarctions, from secondhand smoke and small particulate matter (PM 2.5) air pollution
(8-11). Furthermore, because deaths from CVD have declined partly because of improvements in emergency and acute care, we incorporated a downward trend in the CVD case-fatality rate for 1990 through 2003
(12).
Obesity contributes to CVD, largely through diabetes, high blood pressure, and high cholesterol levels
(13). Other indirect influences in the model are physical inactivity, poor diet, psychosocial stress, and smoking as it affects diabetes and obesity (14-21).
Both the direct and indirect influences in the model may be modified by 19 interventions
(Table 1). These 19 interventions could be implemented at a city, county, or state level rather than requiring changes nationwide. In functional terms, the interventions are of a few basic types: those that provide broader access to health-promoting services, those that promote desirable behaviors, and those that tax or regulate to deter undesirable behaviors.
Cost calculation
We used a common metric — constant 2005 dollars — to track medical and productivity costs (for morbidity and mortality) that might be affected by the 19 interventions. We measured the societal value of morbidity (sick days) and premature mortality (years of life lost) using a human capital approach, which estimates the market value of lost productivity at work and at home
(22). (A detailed description of cost calculations is available at
http://sustainer.org/cvd/documents/SELI_App2.pdf.) This summary of medical and productivity costs can determine whether any intervention, or package of interventions, is justified by its likely aggregate consequences, or “total consequence costs.” We did not estimate the costs of interventions. However, the total consequence costs can inform spending decisions. For example, suppose that for a given intervention the model calculates a total consequence cost savings of $50 per capita. Planners
may then conclude that up to $50 per capita could be justifiably spent to implement that intervention and still create positive net benefits to society.
The model tracks 3 types of intervention consequences:
- Medical and productivity costs attributable to fatal and nonfatal CVD events.
- Medical and productivity costs attributable to noncardiovascular complications of smoking (eg, lung cancer), diabetes (eg, blindness), high blood pressure (eg, kidney failure), and obesity (eg, colorectal cancer). We have thus far been able to quantify these costs, but not yet
the costs related to noncardiovascular complications of stress (eg, depression), physical inactivity (eg, back pain), or poor diet (eg, colorectal cancer).
- Costs of services and products to manage risk factors. These include medications and visits for managing chronic disorders, mental health services, weight-loss services, and smoking cessation services and products.
Model calibration
Although the model is meant to investigate interventions in localities such as Austin/Travis County, we began by calibrating it to represent the entire United States. This approach enabled more precise estimation, given that certain data were either unreliable or unavailable at the local level. The results are generally reported as per capita estimates to facilitate interpretation at a local level.
Table 2 lists the major information sources on which the model is based (23-32).
The model specifies initial (1990) incidence rates for smoking, obesity, diabetes, high blood pressure, and high cholesterol, as well as cessation rates for smoking and obesity. These parameters have been set so that the model accurately simulates the observed changes in prevalence
rates in the National Health and Nutrition Examination Survey from 1988-1994 to 1999-2004.
The model also contains 56 causal links requiring the estimation of relative risks, effect sizes, or initial values. Many of these parameters were estimated through the use of published studies, meta-analyses, and in some instances, ad hoc surveys of veteran practitioners
(33). Because most of these parameter estimates have some level of uncertainty, we also identified lower and upper bounds to be used for sensitivity analysis.
Model testing
Having calibrated the model to accurately reproduce observed trends in risk factor prevalence
rates as well as CVD events and deaths, we then explored plausible futures. A base case scenario assumed no changes after 2004 in many of the local determinants of risk in the adult population, including healthiness of diet, extent of physical activity, stress, use of quality primary care, air pollution, and the prevalence
rates of smoking and obesity among incoming 18-year-olds. This base case should not be
taken as a statement about what is most likely to happen in the absence of intervention, but rather serves as a straightforward and easily understood benchmark against which to compare intervention scenarios.
We tested interventions singly and in groups of similar interventions. For all interventions, we assumed a 1-year ramp-up during 2009, followed by full implementation from 2010 through 2040. The significance of full implementation depends on the intervention, but in all cases is based on effect sizes that the research literature or veteran practitioners indicate should be possible:
- For the 7 marketing interventions and for taxes on tobacco or junk food: doing the maximum that has been demonstrated or seriously proposed somewhere in the United States.
- For the 6 access interventions: raising access to 100%.
- For smoking restriction: reducing secondhand exposures in workplaces and public places to zero.
- For air pollution: reducing small particulate matter by 50% from its 2001-2003 value.
- For sources of chronic stress: a 50% reduction.
- For the quality of primary care (ie, adherence to guidelines): improvement from a national average of 54% (27) to 75%.
For each intervention scenario, we conducted separate simulations using the midpoint, lower-end, and upper-end values for all uncertain parameters. This method yielded a range of plausible outcomes for each intervention scenario.
Back to top
Discussion
Base case results
The base case projects that even after 2004, when we assume no further
changes to the model’s inputs, historical trends in the model’s risk factor
prevalence rates will continue through 2040, although with diminishing slopes. In
particular, the model projects further declines in smoking (and, thus,
secondhand smoke exposure) and high cholesterol, and at the same time further
growth in high blood pressure and diabetes. The projected continuation of past
trends reflects the eventual death of older cohorts and their replacement by
younger cohorts with different habits and characteristics. For instance, the
continued decline of smoking prevalence reflects the lower rate of smoking among
teens and young adults today than in previous decades. Such demographic turnover
also helps explain the continued growth of high blood pressure and diabetes,
which occurs in the model as a legacy of the increase in obesity — a leading
risk factor for both disorders — from 1980 to 2004. The projected continuation
of trends also reflects the future aging of the population; the over-65
population will increase from 2010 through 2030. This aging effect contributes
to the projected decline in smoking because smoking is much less common among
the elderly. It also contributes to the projected increase in high blood
pressure and diabetes because the prevalence of these disorders is higher with
increasing age.
Deaths from first-time CVD events, which declined by 35% from 1990 to 2004,
are projected in the base case to rebound by 33% from 2004 to 2040. Much of the
past decline is attributable to a 28% reduction in the event fatality rate, from
improvements in emergency and acute care. But it also reflects an 11% decline in
the rate of CVD events that occurred, despite increases in high blood pressure
and diabetes, because of decreases in smoking, secondhand smoke, PM 2.5 air
pollution, and uncontrolled high cholesterol.
The potential future rebound in deaths anticipated by our model reflects a
17% increase in fatality from CVD events per capita and a 15% increase in the
rate of CVD events because of the aging of the population. Although the base
case projects no future increase in CVD events or deaths within each age group,
the aging of the population will lead to an increase in the overall rate of CVD
events and deaths.
Per capita total consequence costs, which the model calculates to have
declined by 25% from 1990 to 2004, are projected in the base case to decline by
another 5% from 2004 to 2040. Total consequence costs encompass not only CVD
events (which account for 44% of the total costs in 2004) but also
noncardiovascular complications of risk factors (also 44%) and
management of risk factors (12%). Although per capita CVD event costs are
projected to increase by 12% from 2004 to 2040 (reflecting the increase in the frequency
of the events themselves) and per capita risk management costs are projected to
increase by 8% (reflecting the growing demand for blood pressure and diabetes
treatment), these increases are more than offset by a 25% decrease in noncardiovascular complications. This decrease is due to the projected decline
of smoking, which in 2004 was responsible for more than 400,000 noncardiovascular deaths, primarily from lung cancer and chronic obstructive
pulmonary disease. These premature non-CVD deaths from smoking account for a
large fraction (about 28% in 2004) of the total consequence costs calculated in
the model.
Intervention scenario results
Individual tests of the 19 interventions suggest that each can reduce deaths
from first-time CVD events, and most can reduce total consequence costs. Four of
the interventions, however, raise total consequence costs, meaning that they
increase risk factor management costs more than they decrease the costs of
medical events and complications. These 4 interventions include the 2 that
encourage use of mental health services and the 2 that encourage use of weight-loss services. However, because of limitations in the model, planners
should not dismiss these interventions in the real world. In the case of mental
health services, we have not yet estimated the noncardiovascular costs of
depression. In the case of weight-loss services for obese people, our estimates
of cost and benefit are based on conventional dieting and exercise programs,
rather than on bariatric surgery, which, although more costly, also appears to
be more effective (34).
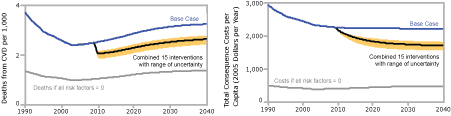
We present simulation results for only the 15 interventions that in
the model do not increase total consequence costs (Figure 2). Such a multipronged approach may be challenging to implement, given resource limitations,
but it is useful to look at what could be achieved.
[View
enlarged image
and descriptive text.]
Figure 2. Estimated impacts of a 15-component
intervention, with ranges based on sensitivity testing, simulation model for
cardiovascular disease (CVD) outcomes. The 15 interventions are listed in
Table 1 under the topical clusters of Care, Air, and Lifestyle.
Key:
Blue line = base case results.
Black line = expected reduction in death rate or costs from the 15-component
intervention when the uncertain parameters are all set to their baseline values.
Orange shaded area around the black line = envelope of plausible outcomes in the
15-component intervention outcomes based on sensitivity testing. Upper edge
(least impact) results when all uncertain impact parameters are set to
their lowest values, while lower edge (most impact) results when all
uncertain impact parameters are set to their greatest values.
Gray line = the model’s calculation of what the death rate or costs would be if
all of the risk factors in the model — smoking, small particulate matter (PM 2.5) air pollution, high blood
pressure, high cholesterol, diabetes, obesity, poor nutrition, inactivity, and
stress — were reduced to zero.
The model suggests that if all risk factors in the model were eliminated, the
death rate could be reduced by approximately 60% below the base case, which
falls between the 50% to 75% rate that other authors have suggested (35). This model
dichotomizes blood pressure, cholesterol, and diabetes as “high” or “not high”
and does not further subdivide the “not high” into normal and borderline.
Reducing borderline conditions (prehypertension, borderline cholesterol,
prediabetes) to normal could further reduce CVD, but we cannot explore this
possibility with this model. (A static analysis of the potential benefits
of reducing both high and borderline conditions is available at http://sustainer.org/cvd/documents/SELI_App3.pdf.)
The model projects that a 15-component intervention could reduce the
first-time CVD event death rate relative to the base case by 20% (range based on
sensitivity analysis, 15%-26%) in 2015 and by 19% (range, 14%-25%) in 2040.
Thus, the interventions that could reduce CVD deaths have a relatively
rapid effect.
The effect of the interventions is more gradual with regard to total
consequence costs than it is with regard to CVD deaths; nearly 40% of the
eventual effect on costs occurs after 2015 (Figure 2). If all risk factors in
the model were eliminated, consequence costs could be reduced by approximately
80% below the base case. Relative to the base run, the 15-component intervention
reduces consequence costs by 16% (range, 12%-23%) in 2015, eventually reaching
26% (range, 19%-33%) in 2040. The reduction in consequence costs is $348 per
capita (range, $254-$514) in 2015 and $565 per capita (range, $416-$722) in
2040.
The 15-component intervention may be better understood by examining the
incremental contributions of its components grouped by topical cluster (Figure
3). We used the same base case graph as in Figure 2 and then incrementally added
the following topical clusters:
1) The 3 interventions that improve the use and quality of primary care
(Care).
2) The 6 interventions related to air quality and smoking (Air).
3) The 5 interventions related to improved nutrition and physical activity
and the 1 intervention that would reduce sources of stress (Lifestyle).
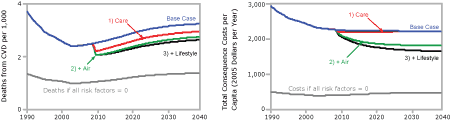
[View
enlarged image
and descriptive text.]
Figure 3. Projected changes in the death rate from
first-time cardiovascular disease (CVD) events and in total consequence costs per capita when 15
interventions are combined, expressed in terms of clusters of interventions,
simulation model for cardiovascular health outcomes.
Key:
Blue line = base case results.
Gray line = outcomes if all risk factors were reduced to zero.
Red line = implement the 3 interventions that improve the use and quality of
primary care (Care).
Green line = add the 6 interventions related to air quality and smoking (Air).
Black line = add the 5 interventions related to improved nutrition and physical
activity and the 1 intervention that would reduce sources of stress
(Lifestyle). This scenario includes all 15 interventions and is identical to
the black line in Figure 2.
The relative effects of the clusters are different for CVD deaths than they
are for total consequence costs. Of the 3 topical clusters, the largest
contributor to projected reductions in CVD deaths, both in 2015 and 2040, is
Care, followed by Air and then a smaller (though growing) contribution from
Lifestyle. In contrast, the largest contributor to projected cost reductions,
both in 2015 and 2040, is Air, followed by Lifestyle and then a smaller (and
ultimately negligible) contribution from Care. The contributions to per capita
cost reduction in 2015 are $235 from Air, $71 from Lifestyle, and $42 from
Care. The contributions in 2040 are $393 from Air, $165 from Lifestyle,
and $7 from Care.
Back to top
Conclusions
The major factors that affect cardiovascular health at a population level interact through causal pathways and develop through gradual accumulations that defy simple calculation. This dynamic complexity — and not
just gaps in data — is a challenge for local leaders who want to intervene most effectively given limited resources. Our simulation model helps
meet this challenge by integrating what is known about the various risk factors in a single testable framework for
prospective policy analysis.
The simulations reported here point to several conclusions that local leaders and national allies may find valuable.
1) The CVD death rate has declined in recent years, not only because of improvements in emergency and acute care but also because of reductions in the CVD event rate itself, due to reductions in smoking, secondhand smoke, particulate air pollution, and uncontrolled high cholesterol. If this progress does not continue at a similar pace in the future, however, the CVD death
rate will likely rebound strongly as the population ages.
2) Medical and productivity costs associated with CVD risk factors have declined
because of declines in first-time CVD events and consequent deaths,
and because of reductions in non-CVD deaths (especially lung cancer and chronic obstructive pulmonary disease) associated with smoking. Population aging will likely keep smoking prevalence on a path of decline into the future, so that even if CVD deaths rebound, the total consequence costs
need not rebound.
3) Of 19 interventions that local planners may consider for lowering CVD risk, at least 15 could reduce CVD deaths without increasing total consequence costs.
4) Interventions aimed at reducing smoking and improving indoor and outdoor air quality can save lives relatively quickly and can justify intervention spending equivalent to as much as $300 per capita per year for 30 years (in 2005 constant dollars, without time discounting) to achieve the full implementation
targets. Most local health leaders are already aware of the need for tobacco control and smoking bans, but many may not be aware of the contribution of particulate air pollution to CVD risk, even in areas like Austin/Travis County
without heavy pollution.
5) Interventions aimed at improving the use and quality of primary care to diagnose and control high blood pressure, high cholesterol, and diabetes can save lives quickly but should not be expected to save much on total costs,
primarily because of the high cost of medications. Consequently, the intervention spending to achieve and maintain such improvement should not exceed the equivalent of $25 per capita per year for 30 years. Other researchers have similarly found that good preventive care for chronic conditions may be cost-effective but is not necessarily cost-saving (36,37).
6) Interventions to improve nutrition and physical activity and to reduce sources of stress take more time to affect CVD deaths, as
they gradually reduce obesity and other chronic disorders. Nonetheless, their contribution grows over time and may justify intervention spending equivalent to as much as $100 per capita per year for 30 years.
The ability of particular localities to achieve full implementation within these cost limits may vary depending on context and implementation factors. Potential extensions and improvements to the model include the following:
- Modeling medical and personal costs for the post-CVD
event population and targeted interventions for secondary prevention to reduce the rate of recurrent CVD events.
- Modeling the prevalence rates of borderline conditions (prehypertension, borderline cholesterol, prediabetes) and incorporating them in the CVD risk calculations.
- Modeling the prevalence of former smokers and incorporating their differential risks in the CVD event and cost calculations.
- Incorporating the non-CVD consequences of stress, physical inactivity, and poor diet.
- Estimating intervention implementation costs to better inform intervention priorities.
- Incorporating additional independent risk factors for CVD (eg, excess sodium intake, excess trans fat intake, vitamin D deficiency, periodontal disease).
The model described here was created through a close collaboration with health planners in Austin/Travis County, who are now using a locally calibrated version of the model to support local strategy design and leadership development. We plan to pursue similar engagements with colleagues elsewhere. With more widespread use, this tool may help health planners across the country transform local contexts to most effectively improve cardiovascular health.
Back to top
Acknowledgments
We acknowledge the contributions of Terry Pechacek, Dave Buchner, Roseanne Farris, Parakash Pratibhu, Deb Galuska, Adolfo Valadez, Karina Loyo, Rick Schwertfeger, Cindy Batcher, Ella Pugo, Jessie Patton-Levine, Josh Vest, Patty Mabry, John Robitscher, Alyssa Easton, Nancy Williams, and Larry Fine.
Back to top
Author Information
Corresponding Author: Jack Homer, PhD, Homer Consulting, 4016 Hermitage Dr, Voorhees, NJ 08043. Telephone: 856-810-7673. E-mail:
jhomer@comcast.net.
Author Affiliations: Bobby Milstein, Darwin Labarthe, Diane Orenstein, Centers for Disease Control and Prevention, Atlanta, Georgia; Kristina Wile, Sustainability Institute, Stow, Massachusetts; Justin Trogdon, RTI International, Research Triangle Park, North Carolina; Philip Huang, Austin/Travis County Health and Human Services Department, Austin, Texas.
Back to top
References
- Bell J, Rubin V. Why place matters: building a movement for healthy communities. Oakland (CA): PolicyLink; 2007.
- Labarthe D. Epidemiology and prevention of cardiovascular diseases: a global challenge. Gaithersburg (MD): Aspen Publishers; 1998.
- A public health action plan to prevent heart disease and stroke. Centers for Disease Control and Prevention; 2003. http://www.cdc.gov/dhdsp/library/action_plan/. Accessed August 14, 2009.
- Sterman JD. Business dynamics: systems thinking and modeling for a complex world. Boston (MA): Irwin McGraw-Hill; 2000.
- Homer JB, Hirsch GB.
System dynamics modeling for public health: background and opportunities. Am J Public Health 2006;96(3):452-8.
- Homer J, Milstein B, Wile K, Pratibhu P, Farris R, Orenstein D. Modeling the local dynamics of cardiovascular health: risk factors, context, and capacity. Prev Chronic Dis 2008;5(2).
http://www.cdc.gov/pcd/issues/2008/apr/07_0230.htm. Accessed August 14, 2009.
- Anderson KM, Odell PM, Wilson PW, Kannel WB.
Cardiovascular disease risk profiles. Am Heart J 1991;121(1 Pt 2):293-8.
- Pope CA 3rd, Burnett RT, Thurston GD, Thun MJ, Calle EE, Krewski D, et al.
Cardiovascular mortality and long-term exposure to particulate air pollution: epidemiological evidence of general pathophysiological pathways of disease. Circulation 2004;109(1):71-7.
- Dominici F, Peng RD, Zeger SL, White RH, Samet JM.
Particulate air pollution and mortality in the United States: did the risks change from 1987 to 2000? Am J Epidemiol 2007;166(8):880-8.
- Mowery PD, Babb S, Bishop EE, Pechacek TF. Comparison of two methods for estimating prevalence of exposure to secondhand smoke in the US population. Paper presented at Towards a Smokefree Society Conference; September 9-12, 2007; Edinburgh, Scotland.
- The health consequences of involuntary exposure to tobacco smoke: a report of the Surgeon General. US Department of Health and Human Services, Public Health Service; 2006. http://www.surgeongeneral.gov/library/secondhandsmoke/. Accessed August 14, 2009.
- Morbidity and mortality: chart book on cardiovascular, lung, and blood diseases. National Heart, Lung, and Blood Institute; 2007. http://www.nhlbi.nih.gov/resources/docs/cht-book.htm. Accessed August 14, 2009.
- Thompson D, Edelsberg J, Colditz GA, Bird AP, Oster G.
Lifetime health and economic consequences of obesity. Arch Intern Med 1999;159(18):2177-83.
- Katzmarzyk PT, Gledhill N, Shephard RJ.
The economic burden of physical inactivity in Canada. CMAJ 2000;163(11):1435-40.
- Fleshner M.
Physical activity and stress resistance: sympathetic nervous system adaptations prevent stress-induced immunosuppression. Exerc Sport Sci Rev 2005;33(3):120-6.
- Elmer PJ, Obarzanek E, Vollmer WM, Simons-Morton D, Stevens VJ, Young DR, et al.
Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. Ann Intern Med 2006;144(7):485-95.
- Rozanski A, Blumenthal JA, Kaplan J.
Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation 1999;99(16):2192-217.
- Björntorp P.
Do stress reactions cause abdominal obesity and comorbidities? Obes Rev 2001;2(2):73-86.
- Kouvonen A, Kivimaki M, Virtanen M, Pentti J, Vahtera J.
Work stress, smoking status, and smoking intensity: an observational study of 46,190 employees. J Epidemiol Community Health 2005;59(1):63-9.
- Willi C, Bodenmann P, Ghali WA, Faris PD, Cornuz J.
Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. JAMA 2007;298(22):2654-64.
- Flegal KM.
The effects of changes in smoking prevalence on obesity prevalence in the United States. Am J Public Health 2007;97(8):1510-4.
- Haddix AC, Teutsch SM, Corso PS. Prevention effectiveness: a guide to decision analysis and economic evaluation. 2nd edition. New York (NY): Oxford University Press; 2003.
- Thom T, Haase N, Rosamond W, Howard VJ, Rumsfeld J, Manolio T, et al.
Heart disease and stroke statistics — 2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2006;113(6):e85-151.
- Mendez D, Warner KE, Courant PN.
Has smoking cessation ceased? Expected trends in the prevalence of smoking in the United States. Am J Epidemiol 1998;148:249-58.
- Sloan FA, Ostermann J, Conover C, Taylor Jr DH, Picone G. The price of smoking. Cambridge (MA): MIT Press; 2004.
- Homer J, Milstein B, Dietz W, Buchner D, Majestic E. Obesity population dynamics: exploring historical growth and
plausible futures in the US. Paper presented at 24th International System Dynamics Conference; July 23-27, 2006; Nijmegen, The Netherlands.
- Asch SM, Kerr EA, Keesey J, Adams JL, Setodji CM, Malik S, et al.
Who is at greatest risk for receiving poor-quality health care? New Engl J Med 2006;354(11):1147-56.
- Russell MW, Huse DM, Drowns S, Hamel EC, Hartz SC.
Direct medical costs of coronary artery disease in the United States. Am J Cardiol 1998;81(9):1110-5.
- Sasser AC, Rousculp MD, Birnbaum HG, Oster EF, Lufkin E, Mallet D.
Economic burden of osteoporosis, breast cancer, and cardiovascular disease among postmenopausal women in an employed population. Womens Health Issues 2005;15(3):97-108.
- Flegal KM, Graubard BI, Williamson DF, Gail MH.
Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA 2007;298(17):2028-37.
- American Diabetes Association.
Economic costs of diabetes in the US in 2002. Diabetes Care 2003;26:917-32.
- Clausen J, Jensen G.
Blood pressure and mortality: an epidemiological survey with 10 years follow-up. J Hum Hypertens 1992;6:53-9.
- Homer J. A dynamic model of cardiovascular risk: reference guide for model
version 8m. Atlanta (GA): Centers for Disease Control and Prevention; 2008.
- Sjostrom L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, Carlsson B,
et al.
Lifestyle, diabetes, and cardiovascular risk factors 10 years after
bariatric surgery. N Engl J Med 2004;351(26):2683-93.
- Magnus P, Beaglehole R.
The
real contribution of the major risk factors to the coronary epidemics: time
to end the “only-50%” myth. Arch Intern Med 2001;161(22):2657-60.
- Russell LB.
Preventing chronic disease: an important investment, but don’t count on cost savings. Health Aff
(Millwood) 2009;18(1):42-5.
- Kahn R, Robertson RM, Smith R, Eddy D.
The impact of prevention on reducing the burden of cardiovascular disease. Circulation 2008;118(5):576-85.
Back to top
|
|
