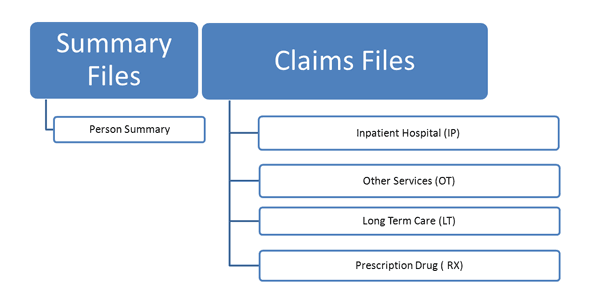
Diagram: NHANES-Medicaid Linked Data Structure
View text version of Diagram
Medicaid enrollment and traditional fee-for-service (FFS) claims data are available for NCHS respondents who are considered linkage eligible and matched to the Medicaid Person Summary (PS) File, which identifies all Medicaid recipients. Respondents are considered linkage eligible if they have sufficient personally identifiable information (PII), and/or did not refuse to provide their SSN and had a verified SSN from SSA. Similar to the Medicare linkage, to be considered a successful match, the NCHS survey respondent’s record needed to match exactly to the Medicaid PS File for the following items: SSN, date of birth (month, year) and sex. CMS provided NCHS with Medicaid enrollment and FFS claims data for all successfully matched NHANES participants. Refer to Course 1, Module 3, Task 2 “NHANES-CMS Linked Data Years of Availability” for the range of years of data that are linked.
Medicaid Analytic eXtract (MAX) data are derived from Medicaid Statistical Information Service (MSIS), and because it is necessary to allow for the delay between service delivery dates and claims adjudication dates, the availability of MAX data for a particular time period lags behind that of the MSIS data.
The following is a list and description of Medicaid files that have been linked with NHANES.
For each calendar year there are five MAX data files, one, the PS, that includes demographic, enrollment, and summary utilization statistics, and four for various types of utilization:
Person Summary (PS) File: The PS File consists of person-level information about Medicaid-eligible persons who have enrolled in a state Medicaid program; it includes demographic data, basis of eligibility, maintenance assistance status, monthly enrollment status, and a utilization summary. The file contains one record for every individual enrolled for at least one day during the year.
You should always include a request for the Person Summary (PS) File as part of the data request.
Inpatient Hospital (IP) File: The IP File contains complete stay records for enrollees who used inpatient services.
Other Services (OT) File: The OT File contains claim records for all non-institutional Medicaid services, including physician services, lab/X-ray, clinic services, durable medical equipment (DME), personal care, and premium payments. Non-institutional services take place in outpatient and hospice facilities, physician offices, and home health settings.
Long Term Care (LT) File:The LT File contains claims records for long term care services provided by Skilled Nursing Facilities (SNF), Intermediate Care Facilities (ICFs), and independent psychiatric facilities. Types of services include mental health, inpatient psychiatric, and intermediate care facilities for the mentally retarded (ICF/MR), and nursing facility days.
Prescription Drug (RX) File: The Prescription Drug File contains claims for paid drug prescriptions. The National Drug Code is used for identification of each drug product. The Prescription Drug File contains one procedure code variable, but no diagnosis codes. Drugs provided during an inpatient stay are not available. Injectable drugs administered by a health care professional are included in the OT file.
Medicaid is administered by states under general guidelines established by the federal government and is financed jointly by federal and state funds. The Federal Medical Assistance Percentage (FMAP), also called the federal match rate, represents the percent of Medicaid financed by the federal government in each state. The FMAP differs by state and takes into account the average per capita income in a state relative to the national average. You can find the FMAP for individual states for each federal fiscal year in the Federal Percentages and Federal Medical Assistance Percentages table produced by the Department of Health and Human Services’ Assistant Secretary for Planning and Evaluation. See the Resources section for the link to this material.
State Medicaid programs must cover mandatory services specified in federal law to receive federal matching funds. Beneficiaries are entitled to receive the following mandatory services:
Medicaid long-term care services include comprehensive services provided in nursing homes and intermediate care facilities for the mentally retarded (ICF‐MR). Long-term care also includes a wide range of services and supports needed by people to live independently in the community, including home health care, personal care, medical equipment, rehabilitative therapy, adult day care, case management and respite for caregivers.
States are also permitted to cover many services that federal law designates as optional, including dental services, prescription drugs, case management, and hospice services. State variation in Medicaid coverage, with regard to both program eligibility and covered services, results in state differences in enrollment rates and expenditures. Other factors, including the age distribution, the poverty rate, and the Medicaid provider reimbursement rates, also contribute to variation among states in enrollment, service use, and costs. As a result, Medicaid operates as more than 50 distinct programs – one in each state, the District of Columbia, and each of the territories. Consideration of these state-level differences may be necessary for many analyses. State identifiers for NHANES need to be specifically requested in those circumstances. State identifiers are not available in public use data files and must be specifically requested in NCHS Research Data Center proposals.