Use of Evidence-Based Interventions to Address Disparities in Colorectal Cancer Screening
Supplements / February 12, 2016 / 65(01);21–28
Djenaba A. Joseph, MD1; Diana Redwood, PhD2; Amy DeGroff, PhD1; Emily L. Butler, MPH3 (View author affiliations)
View suggested citationAltmetric:
- pdf icon [PDF]
Summary
Colorectal cancer (CRC) is the second leading cause of cancer death among cancers that affect both men and women. Despite strong evidence of their effectiveness, CRC screening tests are underused. Racial/ethnic minority groups, persons without insurance, those with lower educational attainment, and those with lower household income levels have lower rates of CRC screening. Since 2009, CDC’s Colorectal Cancer Control Program (CRCCP) has supported state health departments and tribal organizations in implementing evidence-based interventions (EBIs) to increase use of CRC screening tests among their populations. This report highlights the successful implementation of EBIs to address disparities by two CRCCP grantees: the Alaska Native Tribal Health Consortium (ANTHC) and Washington State’s Breast, Cervical, and Colon Health Program (BCCHP). ANTHC partnered with regional tribal health organizations in the Alaska Tribal Health System to implement provider and client reminders and use patient navigators to increase CRC screening rates among Alaska Native populations. BCCHP identified patient care coordinators in each clinic who coordinated staff training on CRC screening and integrated client and provider reminder systems. In both the Alaska and Washington programs, instituting provider reminder systems, client reminder systems, or both was facilitated by use of electronic health record systems. Using multicomponent interventions in a single clinical site or facility can support more organized screening programs and potentially result in greater increases in screening rates than relying on a single strategy. Organized screening systems have an explicit policy for screening, a defined target population, a team responsible for implementation of the screening program, and a quality assurance structure. Although CRC screening rates in the United States have increased steadily over the past decade, this increase has not been seen equally across all populations. Increasing the use of EBIs, such as those described in this report, in health care clinics and systems that serve populations with lower CRC screening rates could substantially increase CRC screening rates.
Introduction
Colorectal cancer (CRC) is the second leading cause of cancer death in the U.S. among cancers that affect both men and women (1). In 2012, the most recent year for which data are available, CRC was diagnosed in approximately 135,000 persons, and approximately 51,000 died from the disease (1). Evidence indicates that screening for CRC reduces its incidence and mortality (2). The U.S. Preventive Services Task Force recommends screening average risk adults aged 50–75 years for CRC with one of three options 1) a guaiac fecal occult blood test (FOBT) or fecal immunochemical test (FIT) annually, 2) a colonoscopy every 10 years, or 3) a flexible sigmoidoscopy every 5 years with a FOBT or FIT every 3 years (2).
Despite strong evidence of their effectiveness, CRC screening tests are underused. In 2012, 65% of U.S. adults aged 50–75 years reported being up-to-date with CRC screening (3). A larger proportion of Hispanics, American Indian/Alaska Native men, and persons living in nonmetropolitan areas (in comparison to non-Hispanics, white men, and those living in metropolitan areas) reported never being screened. A direct relationship between having been screened and educational attainment and annual household income level was also evident. A substantially smaller proportion of those that reported being uninsured or lacking a usual source of care were up-to-date with CRC screening.
Since 2009, CDC’s Colorectal Cancer Control Program (CRCCP) has funded states and tribal organizations to implement evidence-based population-level interventions to increase CRC screening rates in adults aged 50–75 years and to provide limited direct CRC screening services to adults aged 50–64 years who are uninsured or underinsured and below 250% of the federal poverty level. The goal of the CRCCP is to increase CRC screening prevalence to 80% in funded states and tribal areas. Program funds are used primarily to implement evidence-based interventions (EBIs) or strategies recommended in The Guide to Community Preventive Services (Community Guide) to increase use of CRC screening tests (4). These strategies include the following:
1. client reminders (telephone messages and written reminders advising clients they are due or overdue for screening);
2. high quality small media (videos or printed material such as letters, brochures, and newsletters informing and motivating persons to be screened for cancer);
3. reduction of structural barriers (noneconomic burdens or obstacles making access to screening services difficult);
4. provider reminder and recall systems (systems reminding health care providers that a patient is due or overdue for screening); and
5. provider assessment and feedback (interventions that evaluate provider performance in delivering and offering screening to clients and present providers with information about their performance).
CRCCP grantees partner with various entities to implement one or more of these EBIs in clinic, health system, or insurer populations. CRCCP implementation of EBIs has increased over time, with client-oriented EBIs used most frequently (5). Patient navigation, an approach to assist persons to overcome barriers to screening, also has been used by most CRCCP grantees (6). Although patient navigation has not been reviewed by the Community Guide as an independent strategy, several studies supporting its efficacy for increasing CRC screening have been published (7).
This report highlights the implementation of EBIs by two CRCCP grantees: the Alaska Native Tribal Health Consortium (ANTHC) and Washington State’s Breast, Cervical, and Colon Health Program (BCCHP). Alaska Native persons have the highest incidence of CRC among all racial/ethnic groups in the United States, and their CRC mortality rate is twice that among whites (1). The proportion of American Indian/Alaska Native persons who are up-to-date with CRC screening is substantially lower than other racial/ethnic groups (3). Both the incidence of and mortality from CRC in Washington are below the national average; however disparities persist with blacks, having higher CRC incidence and mortality than whites or Hispanics (1). In 2012, 66.8% of adults aged 50–75 years were up-to-date with CRC screening in Washington; a lower proportion of Hispanics, American Indian/Alaska Native persons, and persons with lower levels of education or annual household income reported being up-to-date with CRC screening (8).
CDC’s Office of Minority Health and Health Equity selected the intervention analysis and discussion that follows to provide an example of a program that might be effective in reducing colorectal cancer-related disparities in the United States. Criteria for selecting this program are described in the Background and Rationale for this supplement (9).
Methods
Intervention Methods
Alaska Native Tribal Health Consortium
ANTHC is a statewide, tribal, nonprofit, health services organization owned and managed by Alaska Native populations. ANTHC provides health services to members of the 229 federally recognized tribes in Alaska and supports the regional tribal health organizations (THOs) comprising the Alaska Tribal Health System. The Alaska Tribal Health System operates as a large system consisting of village-based clinics, regional hospitals, and a large secondary/tertiary care facility. Leveraging multiple resources, the Alaska Tribal Health System provides comprehensive care for approximately 143,000 American Indian/Alaska Native persons.
Since 2009, the ANTHC CRCCP has focused on improving CRC screening rates by partnering with the Alaska Native Medical Center in Anchorage and with five rural/remote regional THOs serving approximately 40,224 Alaska Native persons. To increase CRC screening, ANTHC facilitated implementation of provider reminders at three THOs and patient reminders at all five THOs and the Alaska Native Medical Center.
ANTHC surveyed regional partner THOs to determine whether their electronic health record (EHR) systems had the capacity to generate provider reminders and found three partner regions with this capability. Because some EHRs did not contain information about CRC screening tests performed before implementation of the intervention or were missing information on tests performed elsewhere, dedicated CRC screening patient navigators reviewed medical charts and updated the EHR system with accurate CRC screening information. Patient navigators also were used at all five partnering THOs to implement client reminders as an outreach strategy to Alaska Native community members to encourage them to get screened. Additional methods used by patient navigators to increase CRC screening included one-on-one patient education, small media distribution, and reduction of structural barriers (e.g., assisting with transportation).
Washington
BCCHP has contracts with six regional contractors to administer program services across the state. Public Health Seattle & King County (PHSKC) is the regional contractor for Clallam, Jefferson, King, and Kitsap counties. In 2011, BCCHP funded PHSKC to implement EBIs to increase CRC screening in the counties served. PHSKC partnered with HealthPoint (http://www.healthpointchc.orgexternal icon), a network of nonprofit community health centers in the Seattle metro area serving historically underserved populations such as the uninsured and racial/ethnic minority populations, to provide funding for staff time and upgrades to the clinics’ EHR to support EBI implementation. The primary goal of the partnership was to increase the proportion of the HealthPoint clinic population aged 50–75 years who were up-to-date with CRC screening.
Patient care coordinators (PCCs) (who functioned as patient navigators) were identified in each clinic to coordinate staff training on CRC screening and to integrate client and provider reminder systems. Using clinic-based EHRs, PCCs identified active panels of patients who were eligible for CRC screening for each provider. PCCs attempted to reach eligible patients by telephone to remind them that they were due or overdue for screening and to schedule an appointment in the clinic. If the patients could not be reached after two attempts, a reminder letter was sent to the patients notifying them that they were due for screening.
To implement provider reminders, medical assistants used the EHR to produce a daily report of patients coming to the clinic who were due for screening; they also ensured that each patient received a FIT kit with a preaddressed, stamped envelope for returning samples to the processing laboratory. HealthPoint waived the lab processing costs for all patients as part of the intervention. To increase FIT kit return rates, PCCs used the EHR to identify patients who had not returned their FIT kits within 2 weeks. Medical assistants then made two attempts to reach these patients by telephone, after which a reminder letter was sent. PCCs also tracked patients with positive FITs (i.e., positive for occult blood in stool) who were referred for colonoscopy to ensure complete follow-up.
Data Collection and Analysis
Alaska Native Tribal Health Consortium
The 1995 Government Performance and Results Act (GPRA) is a law requiring all federal agencies to report performance data annually to the Office of Management and Budget (10). To meet this requirement, the Indian Health Service (IHS) provides data on 22 clinical performance measures with specified benchmarks, including one on CRC screening rates that was added in 2006. This measure represents an important source of national CRC screening prevalence data among American Indian/Alaska Native populations. The CRC screening definition used for the GPRA measure is based on diagnostic and procedure codes obtained from medical records. The numerator includes patients who have had any CRC screening, defined as any of the following: 1) an FOBT or FIT during the annual report period, 2) a flexible sigmoidoscopy or double contrast barium enema in the past 5 years, or 3) a colonoscopy in the past 10 years. Use of double contrast barium enema as a screening test was included in the screening measure until 2013, when it was removed to align the measure with changes in the U.S. Preventive Services Task Force recommendations. Until 2013, the denominator included all living IHS patients aged 51–80 years without a documented history of CRC or total colectomy with two or more visits to an IHS health facility within the previous 3 years and residing in the service area during the reporting period. Participation in GPRA reporting by Alaska regional THOs is voluntary and varies by THO.
The 2005–2012 annual, Alaskan, statewide GPRA rates representing data from 9–13 regional THOs and the available annual region-specific GPRA rates from regional THOs participating in the intervention were used to evaluate differences in screening rates before and during program participation (2009–2012). Region A did not report GPRA data for 2009. Statewide rates from the 2012 Alaska Behavioral Risk Factor Surveillance System also were used to assess CRC screening rates in the American Indian/Alaska Native population and the general population in Alaska. Data from the 2010 Behavioral Risk Factor Surveillance System cannot be used for comparison because of changes in the survey methods (11).
Washington
Demographic data for 2011, the year the intervention was initiated, were obtained from the Health Resources and Services Administration Uniform Data System, and include patients who had at least one clinical visit within the calendar year for the variables presented (12). Data from the clinics’ EHR were used to generate descriptive statistics of clinic-level CRC screening rates. CRC screening rates were calculated as the proportion of adults aged 50–75 years without a documented history of total colectomy who had at least one visit to the clinic in the previous 18 months and had documentation of appropriate screening for CRC. Appropriate CRC screening was defined as documented colonoscopy within 10 years, flexible sigmoidoscopy within 5 years, or FOBT or FIT within a year of the reporting period end date.
Results
Alaska Native Tribal Health Consortium
In 2009, before initiation of the program, the proportion of all adults aged 51–80 years included in the statewide GPRA rate who were up-to-date with CRC screening was 50.9% (Figure 1). By 2012, this proportion had increased to 58.4%, with an average annual increase of 3.8% per year. Regional proportions for reporting THOs varied with Region A having the lowest proportion of eligible adults screened in 2010 (24.4%) and Region D having the highest proportion in 2009 (64.2%). All reporting regions showed increases. Region A had the largest increase in the proportion of adults who were up-to-date with CRC screening, increasing from 24.4% in 2010 to 67.6% in 2012, whereas Region D had the smallest absolute increase (64.2% to 66.8%).
Data from the Alaska 2012 Behavioral Risk Factor Surveillance System demonstrated that the proportion of Alaska Native adults aged 50–80 years who were up-to-date with CRC screening was 59.8%. The proportion of all Alaskan adults aged 50–80 years who were up-to-date with CRC screening was 58%.
Washington
In 2011, HealthPoint clinics served 65,582 patients, 59.7% of whom were aged 18–64 years (Table). A substantial proportion of patients represented racial/ethnic minority populations; most had annual household incomes ≤200% of the federal poverty level (97.4%). Most of the clinic population was either uninsured (41.8%) or insured by Medicaid or the Children’s Health Insurance Program (44.8%).
Among the seven participating clinics in 2011, the baseline proportion of adults aged 50–75 years who were up-to-date with CRC screening was 24% (Figure 2). By 2014, this proportion had increased to 48%. The proportion of adults that were up-to-date with screening in 2011 varied by clinic and ranged from 17% in clinic E to 32% in clinic G. All clinics showed increases. Clinic D had the largest absolute increase in the proportion of adults who were up-to-date with CRC screening, increasing from 24% in 2011 to 53% in 2014, and clinic E had the smallest absolute increase (17% to 32%).
Discussion
This report describes evidence-based activities implemented by health care organizations to increase CRC screening in historically underserved populations. In Alaska, use of client and provider reminders and patient navigators contributed to increases in the proportion of Alaska Native adults aged 50–80 years who were up-to-date with CRC screening from 50.9% in 2009 to 58.4% in 2012. In Washington, the use of dedicated staff to implement clinic systems to support CRC screening and the use of client reminders helped to increase the proportion of adults aged 50–75 years who were up-to-date with CRC screening from 24% in 2011 to 48% in 2014 in the participating clinics. By comparison, national data from the National Health Interview Survey indicate that 59.2% of adults of any race/ethnicity aged 50–75 years were up-to-date with CRC screening in 2010, and 58.2% were up-to-date in 2013 (13).
CDC encourages CRCCP grantees to implement one or more EBIs recommended by the Community Guide in health systems and other settings to increase CRC screening in the population. A systematic review of these interventions found their use resulted in median increases of 11%–15% in completed CRC screenings (14). On average, CRCCP grantees have implemented three EBIs, with client-oriented interventions (i.e., client reminders and small media), which grantees report as easier to implement, being the most commonly used (15). CRCCP grantees were found to be more likely to implement EBIs than state health departments without CDC funding, suggesting that with sufficient programmatic support, these interventions can be widely adopted in various settings and, if implemented, can increase CRC screening (16).
In both the Alaska and Washington programs, instituting provider reminder systems, client reminder systems, or both was facilitated by the use of EHR systems. Although efficient, embedding reminder systems in the EHR might require up-front costs and staff with the necessary skills. EHRs might contain inaccurate, missing, or outdated CRC screening information, or the information might be stored in data fields that cannot be queried systematically, resulting in the generation of inaccurate or misleading provider reminders. However, once properly established, these systems should be sustainable over time.
EHR data also can be mined to implement provider assessment and feedback reports, another EBI appropriate for use in clinical settings. Assessment reports such as those displaying quality clinical measures, including CRC screening, could be produced to assess provider performance over time. These types of reports increase CRC screening rates and allow clinics and health systems to better monitor the health of their overall patient population (14). IHS clinics, clinics funded by Health Resources and Services Administration, and health maintenance organizations (HMOs) all have reporting requirements that include CRC screening rates. EBIs such as those used by Alaska and Washington, whether in individual clinics, health care systems, or insured populations, can help to meet established benchmarks.
Patient navigation is increasingly used as an intervention to address disparities in use of cancer screening tests and to increase screening rates for several cancers, including CRC (17,18). Although shown effective in improving CRC screening adherence (6), patient navigation can be costly given the intensive, individualized approach. Few cost studies have been published; however, some have demonstrated cost savings for endoscopy centers because navigators can increase screening volume and reduce patient no-shows and cancellations (18–20).
Alaska and Washington implemented more than one EBI in their implementation sites. Rather than relying on a single strategy, using multicomponent interventions in a single clinical site or facility can support more organized screening programs and result in greater increases in screening rates. Most CRC screening in the United States is opportunistic (i.e., persons are often offered screening tests during a clinical visit conducted for other reasons). This method relies on the provider to remember to offer screening when patients appear in the office. Organized screening systems have an explicit policy for screening, a defined target population, a team responsible for implementation of the screening program, and a quality assurance structure (21). Implementing multiple interventions such as client and provider reminders and patient navigation often requires institutionalization of many of the aspects of an organized screening system. Consistent with findings described in this paper, these coordinated efforts can contribute to an increase in CRC screening rates above that seen with usual opportunistic care.
Use of multiple interventions might require more time and effort at the outset to establish routines and collect and monitor data on screening rates and follow-up; however, once these routines are established and institutionalized, less staff time and resources might be needed to maintain these efforts. Maintenance of CRC screening as a priority in the clinical setting is necessary, although it might be difficult to sustain given competing priorities (e.g., multiple chronic diseases and lack of time or desire to address nonurgent health issues) for the target patients and their providers. At ANTHC, initiating use of provider reminders in the EHR was initially hampered by competing clinical priorities, which was resolved by requiring use of provider reminders as a condition of funding. In the absence of specific grant funding to support implementation of multicomponent interventions, alternative incentives are needed to prioritize support of these efforts, such as required reporting of CRC screening rates to insurers as a quality measure. By adhering to the principles of population management and data usage, health care professionals can apply these processes to prevent other health conditions or to manage chronic disease. Organized screening systems might increase the likelihood of the uptake and maintenance of the interventions in the absence of specific funding.
Limitations
The findings in this report are subject to at least two limitations. First, CRC screening rates were not compared with a nonintervention group. The primary purpose of these interventions was to increase CRC screening in the targeted populations as measured by CRC screening rates before and after the intervention, rather than through comparison to a nonintervention group. Because the interventions implemented already have a strong evidence base demonstrating their efficacy, interventions were not evaluated with the intention of proving the effectiveness of the intervention itself. Assurance that the observed changes in CRC screening rates were due solely to the intervention alone cannot be provided. Second, systematic intermediate outcome data (e.g., the number of patients who scheduled or completed a CRC screening test after receiving a reminder, the percentage of FIT kits distributed that were returned, or the proportion of patients who received patient navigation services and completed screening) were not collected.
Conclusion
Although CRC screening rates in the United States have increased steadily over the past decade this increase has not occurred equally across all populations. Increasing the use of the types of EBIs described in this report in health care clinics and systems that serve populations with lower CRC screening rates could substantially increase CRC screening rates. State health departments, tribal organizations, and other public health entities can play a key role in these efforts by partnering with health care providers to support the use of EBIs in clinical settings.
Corresponding author: Djenaba A. Joseph, Division of Cancer Prevention and Control, National Center for Chronic Disease Prevention and Health Promotion, CDC. Telephone: 770-488-3157; E-mail: dajoseph@cdc.gov.
1Division of Cancer Prevention and Control, National Center for Chronic Disease Prevention and Health Promotion, CDC, Atlanta, Georgia; 2Alaska Native Epidemiology Center, Alaska Native Tribal Health Consortium, Anchorage, Alaska; 3Breast, Cervical, and Colon Health Program, Washington State Department of Health, Tumwater, Washington
References
- CDC, US Cancer Statistics Working Group. United States cancer statistics: 1999–2012 cancer incidence and mortality data report . Atlanta, GA: US Department of Health and Human Services, CDC; National Cancer Institute; 2014. http://www.cdc.gov/uscs.
- US Preventive Services Task Force. Final recommendation statement, colorectal cancer: screening . Rockville, MD: US Preventive Services Task Force; 2014. http://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/colorectal-cancer-screeningexternal icon.
- CDC. Vital signs: colorectal cancer screening test use—United States, 2012. MMWR Morb Mortal Wkly Rep 2013;62:881–8. PubMedexternal icon
- Community Preventive Services Task Force. Updated recommendations for client- and provider-oriented interventions to increase breast, cervical, and colorectal cancer screening. Am J Prev Med 2012;43:92–6. CrossRefexternal icon PubMedexternal icon
- Rice K, Gressard L, DeGroff A, et al. Implementation of system approaches for integrating public health and primary care delivery to increase colorectal cancer screening [Poster]. Presented at Academy Health Annual Research Meeting, San Diego, CA; June 8–10, 2014.
- Escoffery C, Fernandez ME, Vernon SW, et al. Patient navigation in a colorectal cancer screening program. J Public Health Manag Pract 2015;21:433–40. CrossRefexternal icon PubMedexternal icon
- DeGroff A, Coa K, Morrissey KG, Rohan E, Slotman B. Key considerations in designing a patient navigation program for colorectal cancer screening. Health Promot Pract 2014;15:483–95. CrossRefexternal icon PubMedexternal icon
- CDC. Behavioral Risk Factor Surveillance System survey data . Atlanta, Georgia: US Department of Health and Human Services, CDC; 2012. http://www.cdc.gov/brfss/annual_data/annual_2012.html.external icon
- Penman-Aguilar A, Boye K, Liburd L. Background and rationale. In: Strategies to reduce health disparities: selected CDC-sponsored interventions—United States, 2016. MMWR Suppl 2016;65(No. Suppl 1).
- Government Performance and Results Act of 1993, Pub. L. No. 103-62, 107 Stat. 285 (August 3, 1993).
- CDC. Methodologic changes in the Behavioral Risk Factor Surveillance System in 2011 and potential effects on prevalence estimates. MMWR Morb Mortal Wkly Rep 2012;61:410–3. PubMedexternal icon
- Health Resources Services Administration Health Center Program [Internet]. 2013 health center profile . Rockville, MD: US Department of Health and Human Services; 2013. http://bphc.hrsa.gov/uds/datacenter.aspx?q=d&bid=101300&state=WA&year=2013external icon.
- CDC, National Center for Health Statistics. United States National Health Interview Survey 2013 . Hyattsville, MD: US Department of Health and Human Services, CDC; 2013. http://www.cdc.gov/NCHS/nhis/quest_data_related_1997_forward.htm.
- Sabatino SA, Lawrence B, Elder R, et al. ; Community Preventive Services Task Force. Effectiveness of interventions to increase screening for breast, cervical, and colorectal cancers: nine updated systematic reviews for the guide to community preventive services. Am J Prev Med 2012;43:97–118. CrossRefexternal icon PubMedexternal icon
- Hannon PA, Maxwell AE, Escoffery C, et al. Colorectal Cancer Control Program grantees’ use of evidence-based interventions. Am J Prev Med 2013;45:644–8. CrossRefexternal icon PubMedexternal icon
- Maxwell AE, Hannon PA, Escoffery C, et al. Promotion and provision of colorectal cancer screening: a comparison of colorectal cancer control program grantees and nongrantees, 2011–2012. Prev Chronic Dis 2014;11:E170. CrossRefexternal icon PubMedexternal icon
- Paskett ED, Harrop JP, Wells KJ. Patient navigation: an update on the state of the science. CA Cancer J Clin 2011;61:237–49. CrossRefexternal icon PubMedexternal icon
- Wells KJ, Battaglia TA, Dudley DJ, et al. ; Patient Navigation Research Program. Patient navigation: state of the art or is it science? Cancer 2008;113:1999–2010. CrossRefexternal icon PubMedexternal icon
- Elkin EB, Shapiro E, Snow JG, Zauber AG, Krauskopf MS. The economic impact of a patient navigator program to increase screening colonoscopy. Cancer 2012;118:5982–8. CrossRefexternal icon PubMedexternal icon
- Jandorf L, Stossel LM, Cooperman JL, et al. Cost analysis of a patient navigation system to increase screening colonoscopy adherence among urban minorities. Cancer 2013;119:612–20. CrossRefexternal icon PubMedexternal icon
- Levin TR, Jamieson L, Burley DA, Reyes J, Oehrli M, Caldwell C. Organized colorectal cancer screening in integrated health care systems. Epidemiol Rev 2011;33:101–10. CrossRefexternal icon PubMedexternal icon
 FIGURE 1. Percentage of American Indian/Alaska Native adults aged 51–80 years who were up-to-date* with colorectal cancer screening, by region† and year§ — Alaska, 2005–2012
FIGURE 1. Percentage of American Indian/Alaska Native adults aged 51–80 years who were up-to-date* with colorectal cancer screening, by region† and year§ — Alaska, 2005–2012
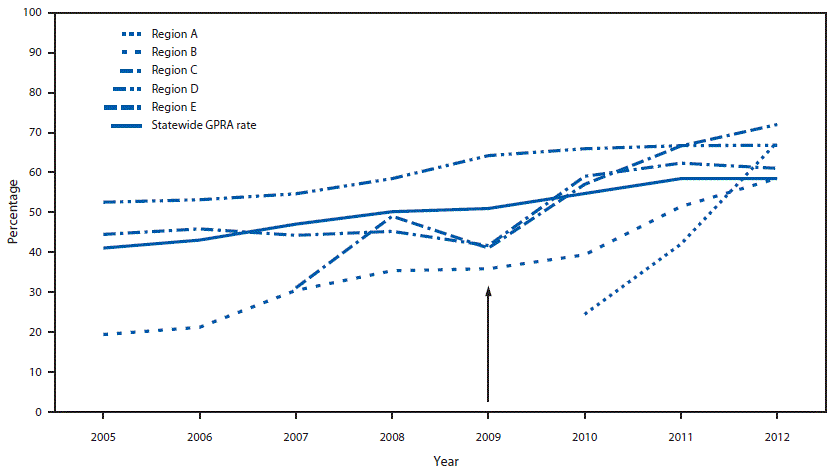
Abbreviation: GPRA = Government Performance and Results Act.
* Persons having fecal occult blood test or fecal immunochemical test within the past year, flexible sigmoidoscopy or double contrast barium enema within the past 5 years, or colonoscopy within the past 10 years.
† Regions indicate different tribal health organizations.
§ Arrow indicates year of implementation of evidence-based interventions.
 TABLE. Demographic characteristics and insurance status of the population* served by HealthPoint clinics — Washington, 2011
TABLE. Demographic characteristics and insurance status of the population* served by HealthPoint clinics — Washington, 2011
| Characteristics | %† |
| Age (yrs) | |
| <18 | 36.3 |
| 18–64 | 59.7 |
| ≥65 | 4.0 |
| Race/Ethnicity | |
| White | 63.2 |
| Hispanic§ | 32.2 |
| Black | 16.1 |
| Asian | 12.9 |
| American Indian/Alaska Native | 1.1 |
| Native Hawaiian/Other Pacific Islander | 4.3 |
| More than one race | 2.5 |
| Income¶ | |
| ≤200% FPL | 97.4 |
| ≤100% FPL | 52.1 |
| Insurance status | |
| Uninsured | 41.8 |
| Medicaid/CHIP | 44.8 |
| Medicare | 3.8 |
| Other third party | 9.6 |
Abbreviations: CHIP = Children’s Health Insurance Program; FPL = federal poverty level.
* N = 65,582.
† Percentages might not total 100% due to rounding.
§ Hispanics might be of any race.
¶ Data from patients with known income.
 FIGURE 2. Percentage of adults aged 50–75 years served by HealthPoint clinics who were up-to-date* with colorectal cancer screening, by clinic — Washington, 2011–2014†
FIGURE 2. Percentage of adults aged 50–75 years served by HealthPoint clinics who were up-to-date* with colorectal cancer screening, by clinic — Washington, 2011–2014†
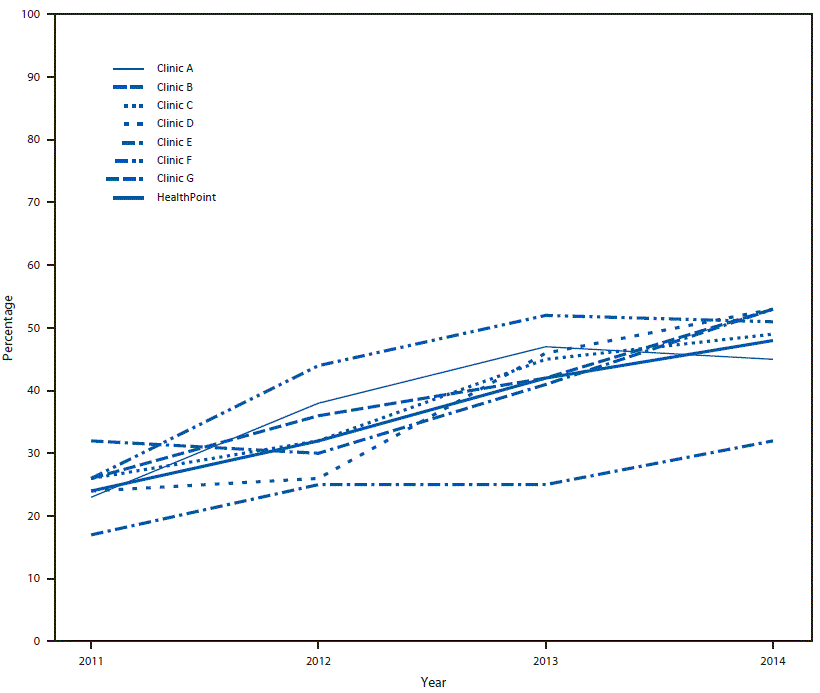
* Persons having fecal occult blood test or fecal immunochemical test within the past year, flexible sigmoidoscopy within the past 5 years, or colonoscopy within the past 10 years.
† Electronic health records provided by HealthPoint, which had the capacity to generate provider reminders, were used to collect data.
Suggested citation for this article: Joseph DA, Redwood D, DeGroff A, Butler EL. Use of Evidence-Based Interventions to Address Disparities in Colorectal Cancer Screening. MMWR Suppl 2016;65place_Holder_For_Early_Release:21–28. DOI: http://dx.doi.org/10.15585/mmwr.su6501a5external icon.
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (https://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.