 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Salmonellosis Outbreak Among Factory Workers --- Huizhou, Guangdong Province, China, July 2004Lunguang Liu,1,2 H.F.
He,3 C.F. Dai,2 L.H.
Liang,3 T. Li,2 L.H.
Li,2 H.M. Luo,2 R.
Fontaine4
Corresponding author: Lunguang Liu, Sichuan Center for Disease Prevention and Control, 40 Huaishu Street, Chengdu, Sichuan 610031, China. Telephone: 852-28-86770124; Fax: 852-28-86770121; E-mail: liulunguang@vip.sina.com. Disclosure of relationship: The contributors of this report have disclosed that they have no financial interest, relationship, affiliation, or other association with any organization that might represent a conflict of interest. In addition, this report does not contain any discussion of unlabeled use of commercial products or products for investigational use. AbstractIntroduction: During July 9--14, 2004, an outbreak of gastroenteritis occurred among workers at an electronics factory in Huizhou, Guangdong Province, China; 199 cases were reported. A case-control investigation was initiated to identify the agent and the mode of transmission. Methods: Stool samples were collected from 142 workers and food handlers and cultured for enteric pathogens. A questionnaire concerning meals and foods eaten in the factory cafeteria during July 11--13 was administered to 92 ill workers and 100 controls. Results: Of approximately 2,000 workers who worked during the outbreak, 197 (10%) had illness consistent with the case definition. Salmonella enteritidis was identified from 44 (31%) of 142 stool samples collected from ill workers. Ill workers were more likely than controls to have eaten breakfast in the factory cafeteria during July 11--13. Of eight foods served at breakfast in the factory cafeteria, three were associated with illness: cake, bread (on July 12 only), and congee (i.e., rice porridge). Stratification of bread and congee exposure by cake consumption indicated that only bread eaten on July 12 was associated with gastroenteritis. The cake was baked on July 11, and a mixture that included raw eggs was poured on top; the cake was then stored at room temperature and served for breakfast on 3 consecutive days (July 11--13). The bread was stored together with the cake on July 11 and 12. No leftover food was tested. Discussion: The investigation indicated that an outbreak of S. enterica serotype Enteritidis resulted from consumption of an unusual food vehicle (i.e., cake) that had been contaminated from a more typical source (i.e., raw eggs). The bread was stored at room temperature together with cake on which a mixture made from raw eggs had been poured. The bread was probably contaminated by contact with the cake. Conclusion: Food handlers should be instructed that intact fresh eggs can harbor S. enteritidis, foods made from eggs must be cooked, and prepared food must be stored under refrigeration. IntroductionOn July 13, 2004, a local hospital reported to the Huizhou City Center for Disease Control (CDC) that approximately 70 patients had been admitted that day to the hospital with gastroenteritis characterized by diarrhea, fever, nausea, and vomiting. All 70 patients were workers at a local factory that manufactured electrical products. Investigators from the Huizhou and Guangdong CDCs visited the hospital and the factory to identify the agent causing this outbreak. Initial interviews and review of medical records indicated that for the majority of patients, onset of gastroenteritis occurred during a 2-day period (July 12--13). MethodsA case of gastroenteritis was defined as illness occurring in either a factory worker or in a family member who ate a meal at the factory cafeteria during July 7--16 and who had diarrhea (two or more liquid stools per day) or fever >99.5ºF (>37.5ºC) in addition to one of three symptoms: nausea, vomiting, or abdominal pain. Ill workers were identified from doctors' reports and from an announcement to workers. Stool samples were collected from 142 patients (136 workers and six food handlers) and 24 healthy food handlers. Stool samples were inoculated to Shigella-Salmonella agar and common agar culture of enteric bacterial pathogens, including Shigella, Salmonella, and Escherichia coli. Slide agglutination tests were used to identify the suspected bacteria and later the serotype of Salmonella. As the investigation proceeded, other workers were learned to have sought treatment at a second local hospital. A case-control study was conducted to identify the probable vehicle of transmission; 92 ill workers from the two hospitals were selected as a convenience sample, and 100 factory workers with no symptoms of gastroenteritis were selected as controls. Controls lived in the same dormitory or were employed in the same workshop as the ill patients. Ill workers and controls shared similar demographic characteristics. During July 13--15, the workers were administered a standard questionnaire that collected demographic information and asked to state where and what they had eaten at each meal during July 11--13. Because patients reportedly ate all their recent meals in the factory cafeteria and drank only boiled water, the investigation focused on foods served in the cafeteria. Respondents were asked to identify which foods they had eaten for breakfast, lunch, and dinner and to report symptoms of gastroenteritis. Frequencies of exposure of ill workers and controls were compared for all meals. For meals associated with illness, exposures of different foods served were compared among patients and controls. Respondents who did not answer a specific question were not included in the analysis for that exposure. In addition, a field survey was conducted to identify whether anything had happened in the factory cafeteria that was associated with the outbreak, especially in the environment of the cafeteria and the food preparation process. ResultsOf approximately 2,000 factory workers who worked during the 3-day outbreak, 197 (10%) had an illness consistent with the case definition. An additional two family members who also ate in the factory cafeteria became ill. Stool specimens from 44 (31%) of 142 ill workers yielded Salmonella enterica serotype Enteritidis. Of 92 patients interviewed in the case-control study, the most common clinical symptoms were diarrhea (80 [87%]), abdominal pain (72 [78%]), fever (61 [66%]), nausea (26 [28%]), and vomiting (17 [18%]). Onset of illness time was clustered from midnight July 11 through midnight July 13 (Figure). Patients' ages varied (range: 17--50 years; median: 25 years) and reflected the age distribution of the factory workforce. Between one and three cases occurred in each of the factory's 100 dormitories, each of which housed 15--20 workers. A comparison analysis indicated that eating breakfast in the factory cafeteria during July 11--13 was significantly associated with having gastroenteritis (odds ratio [OR] range: 3.5--7.5) (Table 1). Eating lunch or dinner on these days was not associated with illness. Of 92 ill workers, 84 (91%) ate breakfast at least once during July 11--13. Time intervals between eating breakfast and onset of illness varied (range: 12--54 hours). Eight food items were served each day at breakfast: cake, bread, congee (i.e., rice porridge), steam bread, meat-stuffed steam patties, fried rice, fried noodles, and boiled noodles. Eating cake, bread, or congee was associated with illness (Table 2). These three foods were not served at either lunch or dinner. The same cake was served on all 3 days and had the highest OR (OR = 19.0; 95% confidence interval [CI] = 7.4--47.0), whereas bread was associated with illness only on July 12 (OR = 8.9; CI = 2.9--27.0). On all 3 days, the OR for congee was lower (OR = 3.6; CI = 2.0--6.6) than that for cake (OR = 19.0; CI = 7.4--47.0). The bread and cake were baked on the evening of July 10 and first served on July 11; they were then stored together in the same container. The bread was used up after breakfast on July 12 and replaced with newly baked bread on July 13. Cake that was left over on July 12 was served again on July 13. Congee was prepared fresh daily and was not in contact with the bread or cake. Flies were present in the kitchen, and food handlers seldom washed their hands while working. To understand how three different foods could be associated with a single outbreak, investigators stratified the analysis of these three foods, comparing them alone and in combination to a single reference exposure (i.e., workers who had not eaten any of the three foods at any breakfast). This analysis indicated that cake eaten on any of the 3 days and bread served on July 12 were associated with illness (Table 3). Congee alone had no association with illness when eaten without cake but an OR of 53 if eaten with cake. The cake and bread were baked at midnight July 10. Sela oil (a mixture prepared from raw eggs, sugar, vinegar, and water) was poured over the baked cake. On July 10 at midnight, the Sela oil was heated at approximately 104ºF (40ºC) and stored at room temperature (77ºF--86ºF [25ºC--30ºC]) for 3 hours before it was poured on the cake. Then the cake was stored at room temperature for another 4 hours until breakfast. At breakfast, the cake and bread were placed on the same serving platter. After breakfast, the cake and bread were placed together in an open container, stored at room temperature for another 24 hours, and served for breakfast on July 12. The bread was completely eaten on July 12, but leftover cake was served on July 13. Congee was made fresh each morning by boiling rice in water for 1 hour and served while still hot. No cake or bread remained for culture. All eggs used to make the Sela oil were consumed before samples could be collected. Salmonella enterica serotype Enteritidis was isolated from the stool specimens of 10 (33%) of 30 food handlers. Of the 10 food handlers infected with S. enteritidis, six (60%) had gastroenteritis (attack rate: 20%). Swabs from the hands of one food handler also yielded S. enteritidis. DiscussionThe investigation indicated that an outbreak of S. enterica serotype Enteritidis resulted from consumption of an unusual food vehicle (i.e., cake) that had been contaminated from a more typical source (i.e., raw eggs). Sela oil poured on the cake was probably responsible for the initial contamination, and the cake was the source of the infection. The high risk for illness from eating both cake and congee, compared with the absence of risk for eating congee alone, indicates that the cake was the source of the infection. The congee might have had a synergistic effect on the occurrence of illness. The method of preparing congee (boiling rice in water for 1 hour) would not permit salmonella survival to occur once, let alone in three batches on 3 consecutive days. However, congee has a relatively high pH (6.4) and could neutralize stomach acid, thus permitting salmonellae from cake to reach the small intestine. In addition, congee could speed gastric emptying, leading to more of the ingested dose of organisms reaching the small intestine. S. enteritidis was probably transferred from the cake to the bread by contact with a common serving platter or utensil, the hands of a kitchen worker, or flies. Storage for a sufficient time at room temperature then facilitated multiplication of S. enteritidis on the bread. Cross contamination without multiplication of S. enteritidis probably did not occur because this would have caused infection on any or all of the 3 days that the cake was served. The key event in the outbreak was the preparation of the Sela oil. After initial contamination from either raw eggs or another source, both suitable temperature and nutrition were available for 3 hours for salmonellae to multiply before application to the surface of the cake. Once the oil was on the cake, suitable temperatures for growth of S. enteritidis continued for another 4 hours. By the time the cake was sold at breakfast on July 11, it likely was contaminated. Additional incubation of the same cake for 24--48 hours is consistent with the continuing association of illness with the cake for 3 days. The original contamination of the Sela oil with S. enteritidis probably came from the raw eggs. Intact shell eggs are known to become infected with S. enteritidis by vertical transmission (1--3). S. enteritidis is the only salmonella in chicken embryo that can be found inside eggs. One infected egg typically contains 10--20 S. enteritidis bacterial cells, but only a few eggs per 1,000 or even 10,000 become infected (3). Infected eggs are the most likely source of this outbreak. Other less likely possible sources of infection are a food handler having contaminated hands, flies, or other ingredients in the Sela oil. Transmission of S. enteritidis in association with intact chicken eggs was first recognized in the United States in 1986 (4,5). Since then, it has been recognized worldwide (6,7). This is the first outbreak of S. enteritidis in China that has been attributed to raw eggs. However, salmonella surveillance and other outbreak reports suggest that S. enteritidis outbreaks occur more commonly than has been recognized previously. At approximately the same time as this outbreak, gastroenteritis outbreaks attributed to S. enteritidis occurred in two nearby cities (Hong Kong and Guangzhou City, Guangdong Province). Investigation of the Hong Kong outbreak implicated a mango pudding made from raw eggs (8). The Guangzhou outbreak was not investigated. In Hong Kong, salmonella surveillance has indicated that S. enteritidis isolations doubled during 1995--2000 whereas other serotypes remained stable (9). In 10 of China's 31 provinces that have conducted food surveillance, S. enteritidis is among the top seven salmonella serotypes isolated (10). In 2000, S. enteritidis was a leading cause of foodborne salmonellosis in the United States (11,12). The findings in this report are subject to at least four limitations. First, no cake or eggs remained available for testing. Second, certain workers could not recall exactly which foods they had consumed. Third, because of time constraints, ill patients and controls were selected by convenience and might not be representative of all persons. Finally, other possible routes of contamination (e.g., food handlers) could not be excluded. ConclusionAs a result of this investigation, changes were suggested in the methods of preparing Sela oil or any other sauce made from uncooked eggs. Heating the Sela oil to pasteurization temperatures (132.8ºF [56ºC]) for 30 minutes during preparation and storage of the prepared Sela oil or sauce under refrigeration should reduce the risk for salmonellosis. Food handlers should be instructed that intact fresh eggs might harbor S. enteritidis. Because direct use of raw eggs without cooking might cause salmonella contamination of food, food handlers should apply these guidelines to all foods made from eggs and store foods prepared with eggs under refrigeration. Researchers and health-care workers should investigate whether such outbreaks occur more frequently than has been reported previously. References
Table 1 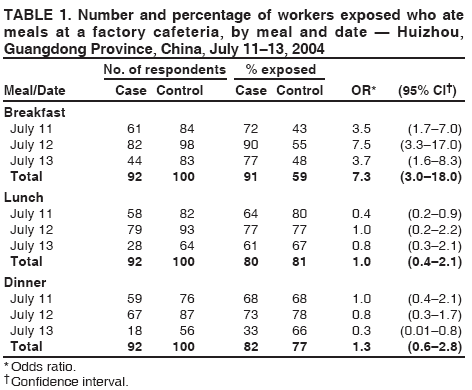 Return to top. Table 2  Return to top. Table 3 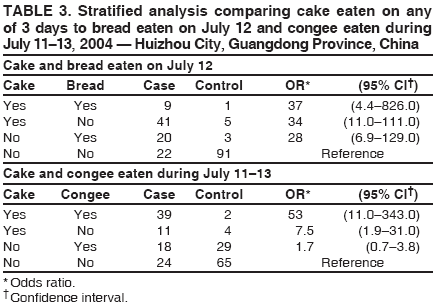 Return to top. Figure 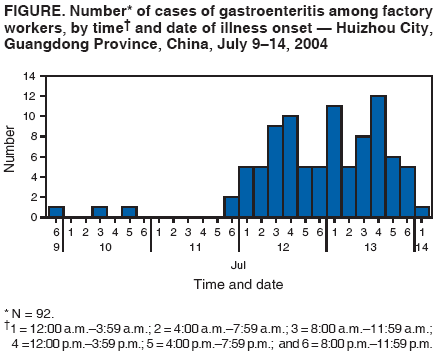 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 4/6/2006 |
|||||||||
|