 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Risk Factors for Brucellosis --- Leylek and Kadamjay Districts, Batken Oblast, Kyrgyzstan, January--November, 2003Turatbek B. Kozukeev,1,2 S.
Ajeilat,1 E. Maes,3 M.
Favorov4
Corresponding author: Michael O. Favorov, 1600 Clifton Rd, MS E-93, Atlanta, GA 30333. Telephone: 404-498-6070; Fax: 404-498-6065; E-mail: MOF0@cdc.gov. Disclosure of relationship: The contributors of this report have disclosed that they have no financial interest, relationship, affiliation, or other association with any organization that might represent a conflict of interest. In addition, this report does not contain any discussion of unlabeled use of commercial products or products for investigational use. AbstractIntroduction: Brucellosis is a zoonotic disease that is associated with chronic serious sequelae in humans. During 1997--2002, the reported incidence of human brucellosis in Kyrgyzstan increased nearly twofold, from 20 to 36 per 100,000 population. In 2002, the highest incidence of brucellosis was reported in two rural districts of Batkan Oblast: Leylek (106 per 100,000 population) and Kadamjay (80 per 100,000 population). During January--November 2003, trainees from the Applied Epidemiology Training program in Central Asia conducted a matched, hospital-based, case-control study to identify risk factors for brucellosis and describe the epidemiology of disease in these two districts. Methods: Brucellosis cases were defined on the basis of epidemiologic, clinical, and laboratory criteria. During January--November 2003, a total of 100 persons with confirmed brucellosis were identified in the infectious disease wards of the two district hospitals; these persons were matched by age and date of admission to 100 controls who were admitted to other hospital wards for unrelated conditions. Data on socioeconomic and occupational factors and history of exposure to animals and animal products were collected by using a structured questionnaire. Conditional logistic regression was used to study the association between exposure variables and brucellosis. Results: Among the 100 persons with confirmed brucellosis during the study period, 86 (86%) owned farm animals, and 45 (45%) became ill during April--May, the birthing season for farm animals. Multivariate analysis indicated that brucellosis was associated with exposure to aborted farm animals in the household (odds ratio [OR] = 29.8; 95% confidence interval [CI] = 4.4--203.4) and consumption of home-made milk products obtained from bazaars or neighbors (OR = 11.4; CI = 1.6--83.9). Knowledge of the mode of brucellosis transmission appeared to be protective against disease transmission (OR = 0.2; CI = 0.03--0.8). Discussion: Exposure to aborted home-owned animals and consumption of home-made milk products obtained from bazaars or neighbors were identified as probable sources of human brucellosis infections in the study districts. This finding suggests that brucellosis spreads among farm animals in the area and that home-made milk products are not adequately pasteurized. Conclusion: To reduce the burden of brucellosis in Batken Oblast, veterinary services should be improved, and health education programs should be increased. Implementing these measures should minimize exposure to farm animals and reduce the risk for infection from locally produced milk products. IntroductionBrucellosis is an infectious zoonotic disease that is associated with chronic debilitating infections in humans and reproductive failure in domestic animals (1). Although brucellosis occurs worldwide, it is more common in countries that do not have effective public health and domestic animal health programs. Kyrgyzstan (estimated 2003 population: 4,892,808) is an almost entirely mountainous country in Central Asia that became independent in 1991 after the disintegration of the former Soviet Union. An estimated 3,180,000 (65%) persons live in rural areas. Agriculture accounts for 44% of the country's gross domestic product (GDP), and half of the country's agricultural GDP comes from the livestock subsector (2). Animal husbandry is the dominant form of agricultural production in the mountainous regions of Kyrgyzstan. During the Soviet era, the collective-farm system that existed in the country accounted for the majority of livestock production; a high level of state veterinary and sanitary control was maintained over the livestock population and production. The collapse of the Soviet Union in 1991 led to social changes and economic hardship that affected all government sectors. The state farming system disappeared, forcing families, especially those in rural areas, to raise farm animals themselves. These changes in the agricultural sector resulted in the loss of the state control over the livestock population and a drastic decline in the quality of veterinary services. In addition, as a result of deteriorating economic conditions, Kyrgyzstan was unable to maintain the health infrastructure inherited from the Soviet era, and the quality and availability of health services declined, especially in rural areas, where neither veterinary nor sanitary inspection agencies provide adequate health services (3,4). Brucellosis can be transmitted to humans through contact with animals or their products; it is an occupational hazard to persons engaged in certain professions (e.g., veterinarians, slaughterhouse workers, and farmers) (5--7). During 1997--2002, countrywide incidence of human brucellosis increased substantially, from 20 to 36 cases per 100,000 population (Kyrgyz Ministry of Health [MoH], unpublished data, 2003) (Figure 1); during the same period, the State Veterinary Department did not report an increase in incidence of brucellosis in animals. The greatest increase in incidence during this 5-year period (from six to 68 cases per 100,000 population) was reported in Batken Oblast, a mountainous area in the southwestern part of the country. In two districts of this oblast, Leylek and Kadamjay, incidence of human brucellosis in 2002 was 106 and 81 per 100,000 population, respectively. MethodsDuring January--November 2003, in response to a request from the Kyrgyz MoH, trainees from the Applied Epidemiology Training Program in Central Asia conducted a hospital-based, matched case-control study in Leylek and Kadamjay districts of Batken Oblast to identify risk factors for brucellosis and describe the epidemiology of disease in these districts. During the study period, 100 persons with confirmed cases of brucellosis were identified in the infectious disease wards of the two district hospitals. A case was defined as illness occurring in a permanent resident of one of the two study districts who was admitted to either of the two local hospitals and who received a clinical diagnosis of brucellosis for the first-time on the basis of the following symptoms: fever (>99.5°F [>37.5°C]) for >5 days, headache and arthralgias, and Wright agglutination test dilution >1:100. A control was defined as a patient with no recent history of brucellosis who was a permanent resident of one of the two study districts and who was admitted to the same hospital with a noninfectious condition during the study period. One control per case was selected and matched by age (±2 years) and date of admission (<2 weeks of the brucellosis patient's date of hospitalization). The Schlesselman formula for matched case-control design was used to calculate sample size, with the following parameters: the significant level was set at 0.05, the desired power was 0.8, and the case-to-control ratio was 1:1. To adjust for confounding, 10% was added to the result. The total number of pairs needed was 100. Informed consent was obtained from all study participants, and person-to-person interviews were conducted. Data on socioeconomic and occupational factors and on exposure to animals and animal products were collected by using a structured questionnaire. Clinical and laboratory data were abstracted from medical records. A period of 2 months before date of illness onset for cases and the same period for corresponding controls was used as the relevant time for measuring these variables. Data management and analysis were performed using Epi Info, version 3.2 (CDC, Atlanta, Georgia). Conditional logistic regression was used to study the association between exposure variables and brucellosis. Potential risk factors were first assessed in the univariate analysis. All variables with p values of <0.2 in univariate analysis were selected for multivariate analysis. The stepwise method of model building was used to arrive at the final statistical model. A p value of <0.05 was defined as statistically significant. ResultsOf 100 persons with brucellosis who participated in the study, 69 (69%) became ill during February--May; with the highest number of illnesses beginning during late April--early May (Figure 2). The age of ill persons varied (range: 1--75 years; mean: 32 years); 66 were males and 87 were of Kyrgyz nationality (Table 1). Twelve patients were collective farm workers; 86 patients reported owning farm animals at home, including cattle (n = 80), goats (n = 70), dogs (n = 50), and sheep (n = 49). Among the 86 persons with brucellosis who had farm animals at home, 70 (81%) cleaned barns, 60 (70%) assisted in animal delivery, and 22 (26%) slaughtered animals (Table 1). Univariate analysis indicated that exposure to aborted animals (OR = 16.0; CI = 4.5--99.2), assistance in animal delivery (OR = 5.6; CI = 2.3--16.3), keeping goats at home (OR = 5.2; CI = 2.1--15.2), cleaning animal barns (OR = 3.0; CI = 1.1--9.2) and being of Kyrgyz nationality (OR = 2.4; CI = 1.1--5.6) were significantly associated with risk for having brucellosis; limited evidence in the univariate analysis suggested that milk products purchased in bazaars or from neighbors (OR = 1.7; CI = 0.9--3.2) might be associated with brucellosis. Multivariate analysis indicated that exposure to aborted home-owned animals (OR = 29.8; CI = 4.4--203.4), exposure to home-made milk products purchased in bazaars or from neighbors (OR = 11.4; CI = 1.6--83.9), and being of Kyrgyz nationality (OR = 4.8; CI = 1.2--20.3) were independent risk factors for having brucellosis. Knowledge of the mode of brucellosis transmission was protective (OR = 0.2; CI = 0.03--0.8). Owning a cow at home was borderline associated with brucellosis (OR = 4.5; CI = 0.9--23.5) (Table 2). DiscussionAlthough brucellosis can occur any time, the majority of cases occurred during February--May 2003, which is the birthing season for farm animals. In this season, Brucella can be excreted in high numbers from infected animals, and the likelihood of exposure to infected animals increases. Similar trends have been observed in other countries (7,8). Humans become infected with Brucellae by coming into contact with animals or animal products that are contaminated with these bacteria. Inadequately heated milk and other dairy products from infected animals are a primary source of infection (6,9,10). Person-to-person transmission of Brucella is extremely rare (1,10). In the two districts studied, exposure to aborted home-owned animals and eating home-made milk products purchased in bazaars or from neighbors were independent risk factors for having brucellosis. Being of Kyrgyz nationality was associated with brucellosis; this might be explained by residual confounding or to other unmeasured risk. Knowledge of the mode of brucellosis transmission was protective, which underscores the importance of health education in preventing of brucellosis. Increased government efforts are necessary to improve education regarding risk factors for brucellosis transmission, especially in rural areas, where human contact with domestic animals is widespread. Brucellosis in Batken Oblast is probably spread among home-owned animals, and home-made milk products obtained from bazaars or neighbors probably are not adequately pasteurized. The spread of brucellosis in farm animals might be attributable to the privatization of collective farms as a result of the changed political and economic situation in the country. Collective farm animals were distributed among small private farms; families who own these animals might disregard or not be aware of sanitary and health requirements necessary to prevent transmission of brucellosis to humans. A probable consequence of privitization of the animal sector is an increased volume of home-made animal food products with inadequate sanitary control over production. Despite the increase in the number of registered human brucellosis cases, the State Department of Veterinary Services did not report an increase in the number of brucellosis cases among animals during the same period. This might reflect the inadequacy of veterinary services. In addition, persons who own their own animals might not seek veterinary service if needed because of fear that they might lose their source of income. These findings were discussed by MoH staff and were presented at conferences attended by staff of international agencies (e.g., the World Bank and the Swiss Emergency Relief Agency). Public health and veterinary officials in Kyrgyzstan have determined that the best approach to reduce the country's brucellosis burden is to focus their resources on improving health education. Together with the nongovernment organization Rural Activists for Health, MoH has developed a prevention campaign that targets persons on rural privately owned farms with livestock. Prevention messages are delivered through the mass media and focus on use of protection methods (e.g., wearing protective clothes, especially when assisting in delivery; not permitting children to have contact with animals; and having sick animals checked by a veterinarian) during contact with animals and adherence to adequate sanitary standards (e.g., boiling or pasteurizing) when processing milk and milk products. Brucellosis health education brochures and flyers are being distributed at infectious disease hospitals, local clinics, and health outposts. In addition, MoH has applied for a grant from the World Bank to fund brucellosis prevention efforts. References
Table 1 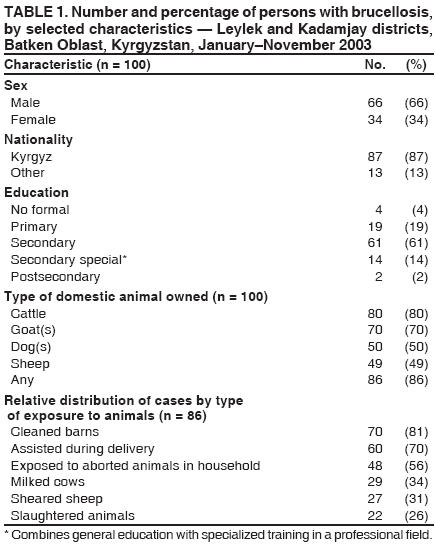 Return to top. Figure 1 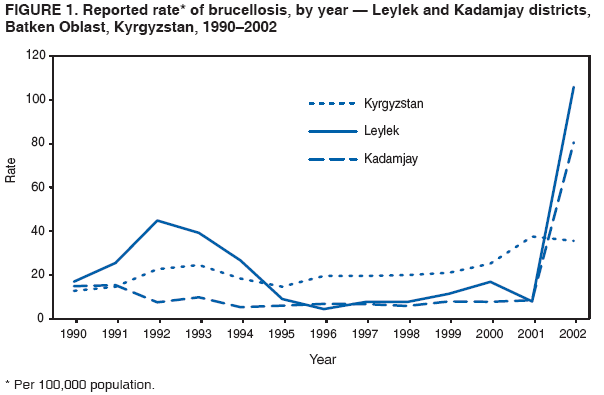 Return to top. Table 2 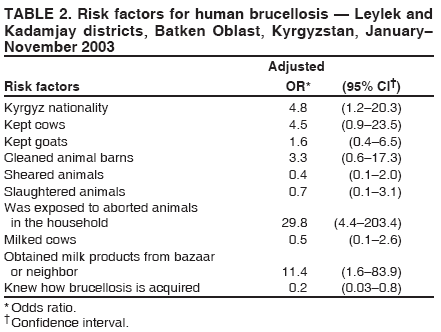 Return to top. Figure 2 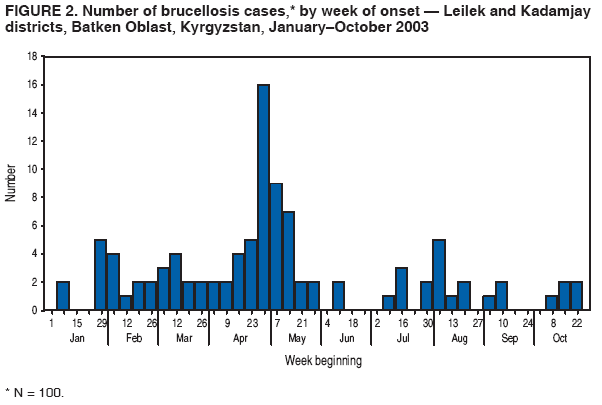 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 4/6/2006 |
|||||||||
|