 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Mortality During a Famine --- Gode District, Ethiopia, July 2000Recurrent famine has been a major cause of mortality in the Horn of Africa (1,2). In Ethiopia, three consecutive years of drought led to widespread loss of livestock, population displacement, and malnutrition, placing an estimated 10 million persons at risk for starvation in 2000 (3). A large proportion of the population of the Gode district in Somali region was displaced in a search for food and food aid (CDC, unpublished data, 2000). From April through July 2000, nongovernmental organizations (NGOs) opened feeding centers in the Gode district. Because no vital statistics or public health surveillance system existed in the district, and no representative mortality or morbidity data were available, during July 2000, CDC, in collaboration with Save the Children U.S., the Office of Foreign Disaster Assistance of the U.S. Agency for International Development, and the United Nations Children's Fund (UNICEF), conducted a mortality survey. This report summarizes the results of this survey, which found persistently high levels of mortality, with measles representing an important cause of mortality in children aged <5 years and 5--14 years. Mass measles vaccination with vitamin A distribution is an important intervention during the acute phase of famines in sub-Saharan Africa. During a two-stage cluster survey in Gode district, the collaborating agencies collected retrospective mortality data from December 9, 1999, through July 31, 2000. A sample size of 3832 persons was required to achieve a 95% confidence interval (CI) with 2% precision around an estimated cumulative incidence of mortality of 10%. The design effect is the factor by which the sample size calculated for a simple random sample needs to be multiplied to account for the dependence of a given variable within a cluster. Although a design effect of two generally is assumed for nutrition surveys, deaths were expected to be more clustered than malnutrition, and a design effect of four was used in this survey. After adjusting for more recent estimates by NGOs involved in food distribution and by the Ethiopian army conducting comprehensive headcounts, the 1994 census (4) was used as the basis for the sampling frame. In the first stage of the survey, 30 clusters were assigned proportionally to village population size. In the second stage, households were selected using Expanded Program on Immunization methods (5). A household was defined as a group of persons who normally lived together and shared meals. Age at death and month of death were identified. Cause of death was assigned using standard case definitions for easily recognized causes of death. Analysis was performed using EpiInfo version 6.04b (6). A total of 595 households comprising 4032 persons was surveyed. In stable, developing countries, the crude mortality rate (CMR) is generally <0.5 deaths per 10,000 persons per day and the mortality rate for children aged <5 years (<5MR) is <1 per 10,000 persons per day (7). During the study period, the CMR was 3.2 (95% CI=2.4--3.8), three times the cut-off level of one per 10,000 per day used to define an emergency (7). The CMR peaked in January 2000 at 6.3 but during July was still 2.0. During the study period, the <5MR was 6.8 (95% CI=5.3--8.0). The <5MR was highest in December 1999 at 12.5 but during July 2000, was 5.5, above the emergency threshold for <5MR of 2--4 (7). Of the 293 deaths that occurred during the study period, 158 (54%) were in children aged <5 years, and 73 (25%) were in children aged 5--14 years. Measles and malnutrition (without an accompanying major communicable disease) each contributed to approximately one fourth of the 159 deaths among children aged <5 years; diarrhea was reported as the cause of death for approximately one third of deaths in this age group (Figure 1). Measles also contributed to 12 (17%) of 72 deaths among children aged 5--14 years. As a result of these findings, the following emergency measures were recommended: 1) accelerating plans for a mass measles vaccination campaign and vitamin A distribution targeting children aged 9 months--5 years; 2) extending coverage of the campaign to include children aged 6 months--14 years; 3) implementing water and sanitation programs to prevent diarrheal disease; 4) continuing treatment for severely malnourished children in therapeutic feeding centers and moderately malnourished children in supplementary feeding programs; and 5) ongoing monitoring of malnutrition (Figure 2) and mortality using cross-sectional surveys in the absence of a regular mortality surveillance system. Reported by: A Teklehaimanot, I Jabr, A Paganini, United Nations Children's Fund. Disaster Preparedness and Prevention Commission, Government of Ethiopia; F Assefa, T Degefie, M Shibeshi, K Zeynu, A Makki, P Brandrup, M Clark, Save the Children US, Gode, Ethiopia. P Morris, R Machmer, K Lattu, Office of Foreign Disaster Assistance, US Agency for International Development. International Emergency and Refugee Health Br, Div of Emergency Environmental Health Svcs, National Center for Environmental Health; and an EIS Officer, CDC. Editorial Note:The age distribution for mortality during the famine in Ethiopia is similar to other famine- and emergency-affected populations. Children, particularly those aged <5 years, usually account for most deaths in such situations (8). Malnutrition, diarrheal diseases, acute respiratory infection, malaria, and measles account for 60%--95% of reported deaths in famines and complex emergencies (7). For children aged <5 years, measles is a leading cause of mortality during these emergencies. Most famines occur in areas of rural sub-Saharan Africa, where measles vaccination coverage is rarely adequate to prevent measles outbreaks during periods of mass displacement and malnutrition. Mass measles vaccination campaigns targeting children aged 6 months--5 years are likely to be cost-effective in such situations (9) and may prevent many more deaths than more high-profile interventions (e.g., feeding centers). The large proportion of measles-related deaths among children aged 5--14 years identified in this survey highlights the importance of extending coverage to children aged >5 years when measles-related mortality is high in this age group (9). The findings in this report are subject to at least three limitations. First, data are subject to recall bias; as a result, the study period was limited to 8 months, and the beginning of the study period was defined by a religious date known to the entire population. Second, only households present on the day of the survey were sampled, possibly resulting in an underestimation of mortality because households in which all members had died during the famine could not have been selected. Finally, because no surveillance system and no birth and death registration existed in the district, comparing verbal reports of mothers with case definitions was used to determine causes of death. Inadequate sensitivity and specificity of case definitions could have resulted in some misclassification of causes of death. Guidelines for humanitarian interventions prioritize interventions to be implemented: rapid assessment, measles vaccination with vitamin A distribution, water and sanitation programs, and food aid (10). In refugee camps, mass measles vaccination campaigns accompanied by vitamin A distribution and water and sanitation programs have become standard practice. This report underscores the importance of these programs in the acute phase of famines in sub-Saharan Africa. Such programs are more difficult to implement in widely dispersed famine-affected populations than in refugee or internally displaced camps, particularly in remote areas, such as the Somali region of Ethiopia, that have no cold chain and poor health infrastructure. Even though food aid and feeding centers also are a priority during famine, attracting a large concentration of susceptible persons to feeding centers may increase transmission of infectious diseases such as measles and diarrhea. Public health programs targeting major causes of mortality should be integrated with feeding programs during famine from the outset of the humanitarian response. References
Figure 1 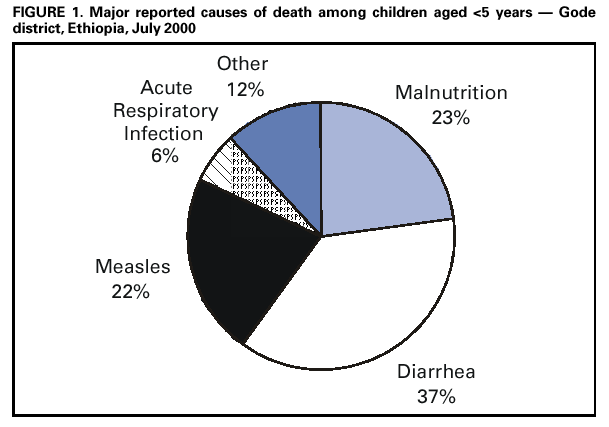 Return to top. Figure 2  Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 4/19/2001 |
|||||||||
This page last reviewed 5/1/2001
|