 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Update: Mortality Attributable to HIV Infection Among Persons Aged 25-44 Years -- United States, 1994During the 1980s, human immunodeficiency virus (HIV) infection, the cause of acquired immunodeficiency syndrome (AIDS), emerged as a leading cause of death in the United States (1). In 1993, HIV infection became the most common cause of death among persons aged 25-44 years. This report updates national trends in deaths caused by HIV infection in 1994, which continue to increase. * Provisional estimates of deaths in 1993 and 1994 were based on a 10% sample of death certificates of U.S. residents filed in all 50 states and the District of Columbia (2,3). Demographic data were reported by funeral directors, and causes of death were reported by physicians, medical examiners, or coroners and encoded according to the International Classification of Diseases, Ninth Revision. Underlying causes of death were classified into the categories in CDC's "List of 72 Selected Causes of Death" for ranking (2). Rates were calculated using midyear U.S. population estimates based on decennial census data compiled by the U.S. Bureau of the Census. Information on Hispanic ethnicity and races other than white and black was unavailable in the provisional mortality data; each race includes Hispanics. In 1994, an estimated 41,930 U.S. residents died from HIV infection, a 9% increase over the estimated 38,500 in 1993; of these, 3% were aged less than 25 years; 72%, 25-44 years; and 25%, greater than or equal to 45 years. HIV infection was the eighth leading cause of death overall, accounting for 2% of all deaths. Among persons aged 25-44 years, HIV infection was the leading cause of death and accounted for 19% of deaths in this age group. In 1994, HIV infection became the fourth leading cause of years of potential life lost before age 65 (YPLL-65) (compared with fifth in 1993), accounting for 9% of YPLL-65 from all causes. Among men aged 25-44 years, HIV infection was the leading cause of death for all men (23% of deaths) (Figure_1) and for white and black men (20% and 32% of deaths, respectively). HIV infection was the third leading cause of death for all women in this age group (11% of deaths) (Figure_2), the fifth leading cause for white women (6% of deaths), and the leading cause for black women (22% of deaths). In 1994, the death rate from HIV infection per 100,000 population among persons aged 25-44 years was almost four times as high for black men (177.9) as for white men (47.2) and nine times as high for black women (51.2) as for white women (5.7). Compared with 1993, the rate for white men in 1994 was similar (47.5 and 47.2, respectively), and rates for the three other sex-racial groups continued to increase: the percentage increase was 13% for black men, 28% for black women, and 30% for white women (Figure_3). Reported by: Surveillance Br, Div of HIV/AIDS Prevention, National Center for Prevention Svcs; Mortality Statistics Br, Div of Vital Statistics, National Center for Health Statistics, CDC. Editorial NoteEditorial Note: This analysis of provisional mortality data for 1993 and 1994 indicates a continuing increase in HIV infection as a leading cause of death in the United States, particularly among persons aged 25-44 years. Among persons in this age group, HIV infection became the most common cause of death for black men in 1991, for all men (all racial/ethnic groups combined) in 1992, and for white men in 1994. HIV became the third leading cause of death among women in this age group in 1994. In addition, as reflected by YPLL-65, HIV infection has become a leading cause of premature mortality. Because this analysis was based on the underlying cause of death recorded on death certificates, the findings in this report probably underestimate the impact of HIV infection on mortality in the United States. Previous studies have indicated that, among persons aged 25-44 years, deaths for which HIV infection was designated the underlying cause represent approximately two thirds to three fourths of all deaths attributable to HIV infection (4,5). The estimated number of death certificates with any mention of HIV infection (i.e., underlying or nonunderlying cause) in 1994 was 48,000 (CDC, unpublished data, 1995), compared with the approximately 42,000 on which HIV was listed as an underlying cause. Based on survival analysis of cases reported to CDC through the AIDS surveillance system -- which includes other sources in addition to data from death certificates -- and the completeness of reporting of AIDS cases and of deaths, an estimated 55,000 to 60,000 persons with AIDS died in 1994 (CDC, unpublished data, 1995). Trends in HIV-related mortality reflect changes in the demographic patterns of the HIV epidemic. For example, from 1993 to 1994, the death rate for HIV infection for white men aged 25-44 years did not change, and rates for women and black men increased; in 1994, the rate for black women aged 25-44 years surpassed that for white men in that age group. The increasing death rate for women affects the care of their children: the estimated 80,000 HIV-infected women of childbearing age who were alive in 1992 will leave approximately 125,000 to 150,000 children when they die during the 1990s (6). Racial differences in death rates for HIV infection probably reflect social, economic, behavioral, and other factors associated with HIV transmission risks. Such factors are being addressed through prevention efforts designed to meet the needs of specific communities (7). Because of the prolonged period from initial HIV infection to onset of severe HIV disease (AIDS) (8), recent trends in HIV-related mortality reflect trends in HIV transmission several years earlier. Similarly, trends in HIV-related mortality in several years will indicate, in part, the effectiveness of current efforts to prevent HIV infection. Despite recent increases in HIV-related mortality, decreases in the percentages of HIV-related deaths resulting from particular opportunistic infections (pneumocystosis, cryptococcosis, and candidiasis) (9) suggest some success in the treatment and prevention of opportunistic infections resulting from HIV infection and underscore the importance of following recently published guidelines for preventing HIV-related opportunistic infections (10). References
Figure_1 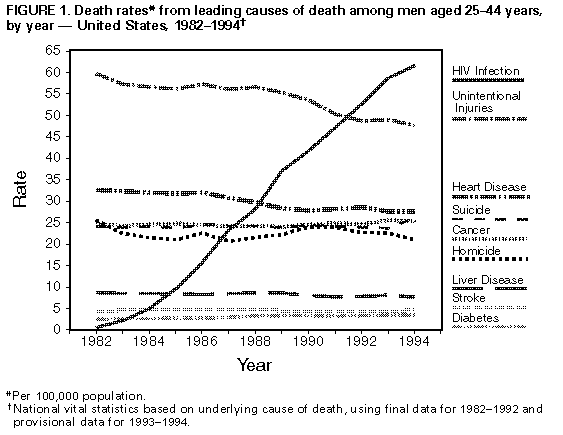 Return to top. Figure_2 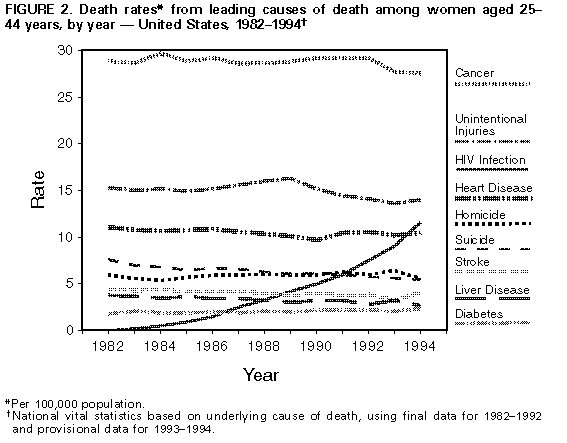 Return to top. Figure_3 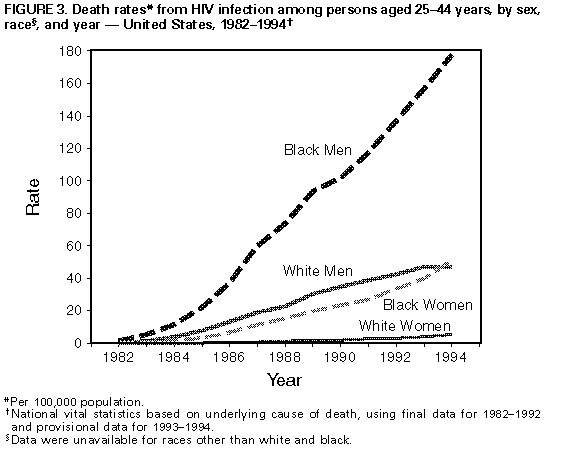 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 09/19/98 |
|||||||||
This page last reviewed 5/2/01
|