 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Measles Outbreak -- Guam, 1994One of the largest outbreaks of measles in the United States and its territories since 1992 occurred in Guam during 1994. From February 8 through June 25, 1994, a total of 280 suspected, probable, or confirmed cases of measles were reported to the Guam Department of Public Health and Social Services (GDPH). Of these cases, 228 were considered confirmed, including 47 serologically confirmed cases Figure_1. This report summarizes findings from the investigation of these 228 cases. The index case occurred in an 8-month-old child who developed a rash on February 7, 1994. This case could not be epidemiologically linked to a previous measles outbreak in Guam (22 cases) that occurred during October 20-December 26, 1993; that outbreak was initiated by an imported case from the Republic of Palau. In addition, genetic sequencing of viral isolates indicated that viruses that had circulated in Palau and in Guam were different. The outbreak peaked in April, when 104 cases were reported. The incidence of confirmed cases was 17 per 10,000 population. Patients ranged in age from 2 months to 57 years (median: 16 months), and 70% of cases occurred among preschool-aged children. The age-specific incidence was highest for children aged less than 1 year (318.0 per 10,000 population), and was higher for children aged 1-4 years (57.9) and 10-19 years (20.1) than for children aged 5-9 years (7.8) and persons aged greater than or equal to 20 years (4.8). Of the 228 cases, 133 (58%) occurred among patients who were Chamorros (an ethnic group native to Guam), 45 (20%) occurred among persons from the Chuuk State of the Federated States of Micronesia (FSM), and 29 (13%) among Filipinos. The highest ethnicity-specific attack rate was among persons from FSM (91 per 10,000 population). The incidence among U.S. military personnel and dependents was three per 10,000 population. Of the 138 (61%) patients aged greater than or equal to 12 months, measles vaccination history was known for 84 (61%). A history of receipt of at least one dose of measles-containing vaccine (MCV) was reported for 52 (62%) persons, and 14 (17%) had documentation of measles vaccination on or after their first birthday and at least 14 days before rash onset. Appropriate vaccination was documented for 7% of those aged 1-4 years and 25% of those aged 5-19 years. No cases were reported among persons who had received two doses of MCV. Twenty-three (10%) patients were hospitalized, and three died (case-fatality rate=1.3%). The three fatal cases occurred among patients aged 9 months, 17 months, and 22 years who were immigrants or children of immigrants from the Chuuk State, FSM. The hospitalization rate was highest among children aged less than 6 months (four {22%} of 18). Outbreak-control measures focused on vaccinating preschool-aged children and immigrants. Routine vaccination clinic hours were extended, and outreach clinics were provided in shopping centers, villages, and housing areas with large immigrant populations. On April 8, GDPH lowered the age for measles vaccination from 12 months to 6 months. In May, GDPH implemented a mass vaccination campaign and encouraged families to take all children aged 6 months-5 years to vaccination clinics for measles vaccination, regardless of previous vaccination history; children with documentation of two doses of MCV after age 12 months were not revaccinated. During March-June, approximately 12,000 doses of MCV were administered, 4000 of which were given to children aged less than 5 years. This was the first measles vaccination for 70% of the children who participated in the campaign. The campaign is estimated to have increased measles vaccination coverage among children aged less than 5 years to approximately 74%. Other outbreak-control efforts included improving passive surveillance by providing outbreak information to health-care providers and active surveillance through periodic phone calls to the civilian hospital and private clinics, instituting triage and isolation for patients with rash illness in medical settings, exclusion of persons with cases from day care centers and schools and vaccination of their contacts, and disseminating public education messages about measles and measles vaccination. Since June 25, when two cases imported from the Philippines were reported, no additional cases are known to have occurred. Reported by: K Cruz, MPH, E Dolor, MD, K Leonhardt, MD, L Duenas, MPH, A Mathew, MD, R Wilson, MS, L Espaldon, MD, R Haddock, DVM, Territorial Epidemiologist, Guam Dept of Public Health and Social Svcs; A Cabanero, MD, Guam Memorial Hospital Authority. Measles Virus Section, Respiratory and Enteric Viruses Br, Div of Viral and Rickettsial Diseases, National Center for Infectious Diseases; National Immunization Program, CDC. Editorial NoteEditorial Note: The mass vaccination campaign in Guam appeared to be an effective strategy for controlling measles outbreaks among island populations. Although the campaign was initiated late in the course of the outbreak, the decline of the outbreak may have been accelerated by efforts to encourage all preschool-aged children to receive a dose of MCV, regardless of prior receipt of one dose of vaccine. Most of the preschool-aged children who participated in the campaign received their first dose of MCV during the campaign; among children who had already received a dose, the campaign also effectively lowered the age at which many children received a second dose of vaccine. * Lowering the age for primary vaccination also was an important control strategy in Guam because the risk was highest among infants. Many of these infants lacked maternal antibody because they had been born to mothers who had received a maximum of one dose of measles vaccine and who had not had natural measles infection (e.g., children of immigrant mothers from islands where previous outbreaks occurred greater than 20 years ago) (1,2). The Advisory Committee on Immunization Practices (ACIP) recommends that measles vaccine be administered at age 6 months if exposure of children aged less than 1 year is likely (3). Children vaccinated before age 12 months should be revaccinated after their first birthday and should be given another dose of MCV before entering school. The outbreak in Guam was especially a consequence of the large number of unvaccinated, preschool-aged children. A retrospective survey in 1991 of the vaccination records of children entering school for the first time documented that only 55% of children on Guam had received a dose of MCV by age 2 years. Audits of records from public and private clinics in 1993 and 1994 indicated that coverage among 2-year-old children with one dose of MCV ranged from 53% to 90% depending on the site. Reasons for higher morbidity and mortality in the Chuukese population than in other ethnic groups are unclear. Possible explanations include low levels of immunity because of low vaccination coverage levels; the lower likelihood of exposure to measles (the last outbreak in Chuuk was in 1968); limited access to health care; and large family size, resulting in increased exposure to measles. Other factors associated with increased risk for measles importation and transmission on islands such as Guam include tourism and the high mobility of the local population. These factors underscore the importance of the need to achieve and maintain high vaccination coverage levels. Approaches to maintaining high vaccination coverage levels among preschool-aged children should include establishing walk-in service to provide vaccinations on a routine basis, extending clinic hours, offering door-to-door vaccination in areas with hard-to-reach populations (e.g., immigrants), educating providers and parents about contraindications to vaccinations, and taking advantage of all opportunities to vaccinate children during health-care visits, as is recommended in the United States. Optimal levels of immunity may be achieved in school children through the establishment and enforcement of requirements for receipt of two doses of vaccine. References
* The second dose of measles vaccine is routinely recommended at entry to primary or secondary school but may be given at earlier ages provided it is administered at least 30 days after the first dose, and both doses are given after age 12 months. Figure_1 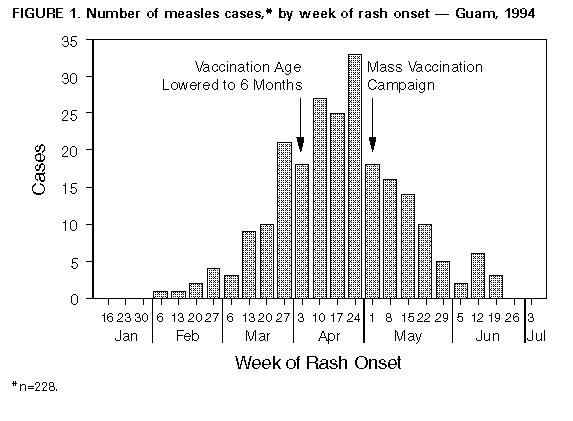 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 09/19/98 |
|||||||||
This page last reviewed 5/2/01
|