 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Current Trends Core Public Health Functions and State Efforts to Improve Oral Health -- United States, 1993Since the 1988 Institute of Medicine report on the future of public health (1), state health agencies (SHAs) have focused on the role of the core functions of public health (i.e., assessment, policy development, and assurance) in improving health in the United States. Oral diseases and conditions are among the most prevalent and preventable chronic health problems in the United States (2). Through use of the core functions as a guideline to identify basic public health practices integral to oral health, SHAs can improve oral health in the United States. To assess the level of involvement among SHAs with core public health functions related to oral health, in January 1994 the Association of State and Territorial Dental Directors (ASTDD) conducted a survey of SHAs in the 50 states and the District of Columbia. This report summarizes the survey findings. ASTDD mailed a 10-question survey about the three core functions related to oral health to the public health official known by ASTDD to have overall responsibility for oral health activities within the SHA. SHAs that did not respond were contacted by telephone. The response rate for the survey was 100%. Respondents were asked about their involvement in oral health-related assessment activities (i.e., use of prevalence data for oral diseases, conditions, treatment needs, or risk factors and methods of collecting such data) since January 1, 1990, and in policy-development and assurance (i.e., primary and secondary prevention services) activities. Of the 51 SHAs, 35 (69%) had full-time (minimum of 40 hours worked per week) dental directors, and 16 (31%) had either part-time (mean: 11 hours worked per week; range: 4-20 hours) (n=5) or no directors (n=11). Of the 11 SHAs with no directors, four reported having vacant director positions, and seven reported having no dental program. Of the 44 states with programs, 20 were mandated by specific legislation or authorized by SHAs. Assessment. The reported level of involvement of SHAs in oral health assessment activities varied substantially (Table_1, page 207). The proportion of states that used selected types of oral health prevalence data ranged from 55% (levels of dental caries among children) to 26% (dental fluorosis). The proportion of states that used selected methods of collecting oral health data ranged from 53% (screenings to assess the dental treatment needs of children) to 31% (statewide dental surveys) (Table_1, page 207). Compared with states with part-time or no dental director, states with full-time directors reported substantially greater involvement in assessment related activities. The difference was greatest for use of prevalence data about dental sealants (Table_1, page 207). Policy development. Seventy-five percent of states reported either "active" or "some" involvement in nine of 12 selected policy-development activities (Figure_1, page 208). The highest levels of active involvement were reported for oral health policies related to fluoride mouthrinsing (67%), water fluoridation (61%), maternal and child health programs for prevention of oral disease (57%), and dental care for low-income persons (53%); the lowest levels were reported for policies related to dental care for underserved populations (i.e., persons who are elderly, human immunodeficiency virus-infected, or eligible for Medicaid). Compared with states with part-time or no dental director, states with full-time directors reported involvement in three times as many policy-development activities. Assurance. Forty-three (84%) states reported that basic oral health education or fluoride-related prevention services were provided in schools; 12 (26%) of 47 states reported that they provided dental restorations (secondary prevention). Of 24 (47%) states that provided dental sealants to children through school-based programs, 20 (83%) had full-time dental directors. Reported by: Association of State and Territorial Dental Directors. Div of Oral Health, National Center for Prevention Svcs, CDC. Editorial NoteEditorial Note: The findings in this report document the variable presence of activities related to core public health functions for oral health in the 50 states and the District of Columbia. The presence of all three core functions was greater in states with full-time dental directors than in those with part-time or no directors or no dental program. Assessment activities provide decision makers with information for policy-development and assurance activities. However, only 56% of SHAs reported involvement in oral health assessment activities, while 82% have reported involvement in general health assessment activities (3). Cost-effective programs that address priority oral health needs are most appropriately based on information representative of groups within a state. Although SHAs conduct surveillance for reportable diseases and conditions, no oral diseases are reportable. Some states have used screenings, surveys, and the Behavioral Risk Factor Surveillance System to estimate oral disease morbidity in defined populations. These assessments permit analysis of factors associated with particular oral health needs and assist in targeting prevention interventions to those at greatest risk for developing disease. Oral health policy development emphasizes activities traditionally managed by dental programs (e.g., water fluoridation and fluoride mouthrinsing). However, state dental programs increasingly are becoming involved with other health issues (e.g., tobacco use, oral cancer, and infection control in the dental environment) that may provide opportunities to integrate oral health-related core function activities into other SHA programs. Since 1971, dental sealants (a clinical oral-health measure used for both secondary and primary prevention) have been used to prevent the most common form of dental caries among children (4). The levels of involvement by SHAs in core function activities, especially those related to dental sealants, demonstrate the importance of full-time dental directors in state efforts to improve oral health. The findings in this report indicate that substantially more oral health-related assessment, policy- development, and assurance activities occurred in states with full-time directors. Such leadership is essential to meet the national oral health objectives for the year 2000 (objectives 13.1- 13.16) (5) -- including one for dental sealants (objective 13.8) -- and assure that persons at greatest risk for oral disease are effectively targeted for prevention interventions. Strategies to improve oral health in the United States through use of the core public health functions related to oral health should include increasing the number of states with full-time dental directors, increasing the level of involvement among states in core function-related activities, and using assessment activities to target disease prevention and health promotion efforts to populations at greatest risk for oral disease. References
TABLE 1. Reported use by state health agencies of oral health prevalence data and
methods of collecting such data, by employment status of dental director --
United States, * 1990-1993
=====================================================================================
Employment status of dental director
-------------------------------------
States with States with
full-time + dental part-time & /no
director dental director @ Total
(n=35) (n=16) (n=51)
------------------ ----------------- ------------
Category No. (%) No. (%) No. (%)
----------------------------------------------------------------------------------
Types of prevalence data used
Dental caries among children 24 (69) 4 (25) 28 (55)
Tobacco use 20 (57) 6 (38) 26 (51)
Dental sealants 23 (66) 2 (13) 25 (49)
Baby bottle caries 13 (37) 3 (19) 16 (31)
Oral cancer 11 (31) 3 (19) 14 (28)
Dental fluorosis 12 (34) 1 ( 6) 13 (26)
Methods of collecting
prevalence data
Screenings to access dental
treatment needs of children 21 (60) 6 (38) 27 (53)
Clinical program data 17 (49) 5 (31) 22 (43)
Behavioral Risk Factor
Surveillance System
dental questions 17 (49) 3 (19) 20 (39)
Statewide dental survey 14 (40) 2 (13) 16 (31)
----------------------------------------------------------------------------------
* The 50 states and the District of Columbia.
+ Minimum of 40 hours worked per week.
& Mean hours worked per week = 11 (range: 4-20 hours).
@ Of the 11 states with no dental director, four had vacant director positions, and
seven had no dental program.
=====================================================================================
Return to top. Figure_1 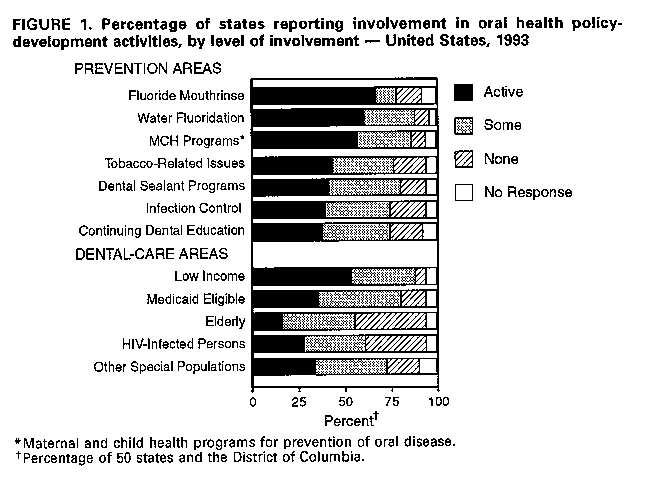 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 09/19/98 |
|||||||||
This page last reviewed 5/2/01
|