Bhutanese Refugee Health Profile
Priority Health Conditions
A list of priority health conditions to consider when caring for or assisting Bhutanese refugees.
Background
Group Origins, Language and Literacy, Religious Beliefs, Caste System, Family and Kinship, Gender Roles, Cultural Approach to Healthcare
Population Movements
From Bhutan to Nepal, From Nepal to the United States
Healthcare and Diet in Camps
Immunizations, Reproductive Health, Gender-Based Violence, Diet and Rations
Medical Screening of US-Bound Refugees
Visa Medical Examination, Pre-Departure Medical Screening, Pre-Embarkation Checks, Surveillance, Post-Arrival Medical Screening
Health Information
General Health Information, Communicable Disease, Non-Communicable Disease, Nutrition, Mental Health
Background
Group Origins
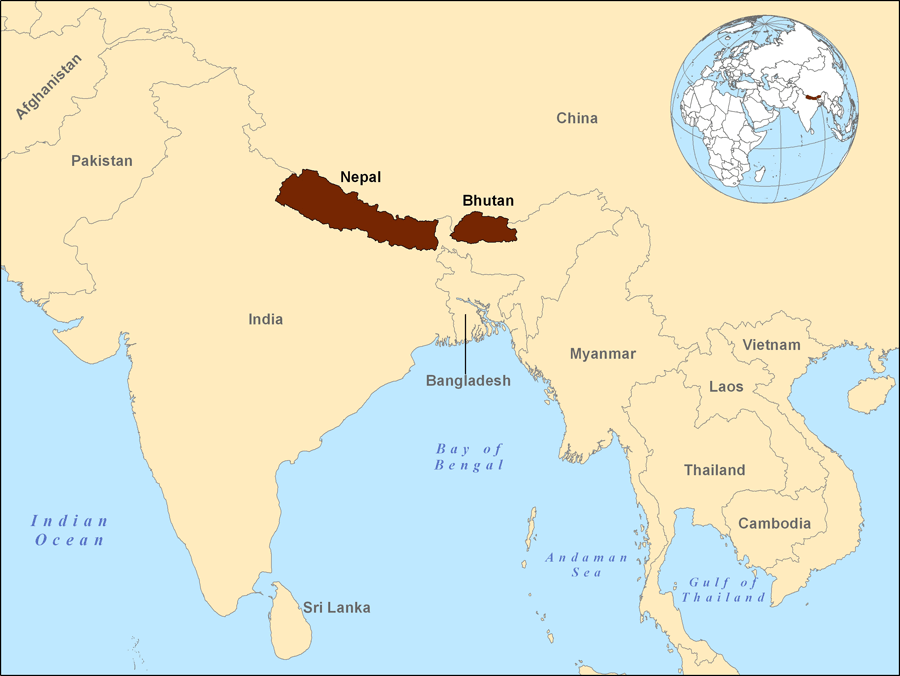
Bhutan is located in the Himalayan Mountains between India and China (Figure 1). The ethnically Nepali, Nepali-speaking Bhutanese, or Lhotsampas (“People of the south”), are a largely Hindu people who moved from Nepal to Bhutan. They lived peacefully in Bhutan until the mid-1980s when Bhutan’s king and the ruling Druk majority feared that their population could overrun the majority group and dilute the traditional Buddhist culture of the Druk Bhutanese. 1 A cultural campaign known as “One country, one people,” or “Bhutanization,” was initiated in order to forge a Bhutanese national identity. The policies forced the Druk dress code, religious practices, and language on all Bhutanese regardless of heritage. These adopted policies alienated the Lhotsampas by attempting to forcibly integrate them into the majority culture. 1 Difficult requirements for proving citizenship were also imposed on the Lhotsampa people, and even those who could provide documentation were usually denied citizenship. 1 Human rights violations were commonplace and by the early 1990s, the “One country, one people” campaign had precipitated a humanitarian emergency. By 1993, more than 100,000 Lhotsampa Bhutanese had fled or were forced out of Bhutan and resettled in southeastern Nepal.
Figure 1: Location of Nepal and Bhutan
Language and Literacy
The majority of Bhutanese refugees are bilingual. Most speak Nepali at home, but some also speak the Bhutanese language, Dzongkha. 1 Younger members of the refugee community have also been exposed to English in the camps in Nepal. The Office of the United Nations High Commissioner for Refugees (UNHCR) estimates that about 35% of refugees in Nepali camps have a functional grasp of English. 3 Among the older refugees, those not born in camps, men speak more English than women. 4 Nepali interpreters, however, were required for nearly 90% of Bhutanese refugee post-arrival medical screening examinations carried out from 2008-2011 in Texas. 15 Among Bhutanese refugees, the literacy rate in their native language is estimated at 65%. 5
Religious Beliefs
Approximately 60% of the refugees are Hindu, 27% are Buddhists, 10% are Kirat (an indigenous animistic faith), and the remaining refugees are Christian. 3
Caste System
Bhutanese refugees follow a complex caste system very similar to that of their Nepalese counterparts. In the refugee camps, there are a total of 64 castes, groups, and parties. 4 The Hindus have four castes, of which Bahun is the highest. In the refugee camps in Nepal and in U.S. communities after resettlement, caste has been declining in importance for many people, while still retaining its value for others. Those who still adhere to the social and behavioral rules of the caste system are unlikely to discuss it openly with outsiders. 1
Family and Kinship
The typical household is large and often includes elderly parents, married sons and their wives and children, and unmarried children. 3 The younger generation is generally responsible for the care of older relatives, reflecting the tradition of respecting one’s elders, regardless of relation. 1 It is common for family disputes, health problems, and financial troubles to be brought to discussions with the elders within the family before action is taken. The Bhutanese community as a whole is tightly-knit, and kinship ties are important. 1
Gender Roles
In Bhutan and in refugee camps in Nepal, gender roles are clearly demarcated. Females perform far more housework, have less access to information and resources, and usually have less decision-making power than males. 3 In some castes, female victims of sexual violence and their families can face alienation from their community.
Cultural Approach to Health Care
Bhutanese refugees often use home remedies as first-line treatment for illness and seek outside medical advice only if their symptoms are not relieved. 1 Traditional healers, called dhami-jakhri, also continue to play a role in health care for many resettled refugees. Patients may need encouragement and positive reinforcement to feel comfortable sharing their use of traditional practices with American providers. Bhutanese refugees tend to seek out care in response to a serious health problem rather than seeking preventive care. The reluctance of the community to seek care unless severely ill may be amplified by the fact that refugees may not have adequate health coverage after the eight-month period of federal resettlement benefits ends, and may be unable to meet the financial costs of medical care. 1 Health care utilization is also affected by traditional gender roles, as mothers may be hesitant to describe their own health concerns but will voice the health concerns of their children or spouse. 4
Additional Resources
For more information about the orientation, resettlement, and adjustment of Bhutanese refugees visit the Cultural Orientation Resource Center.
Population Movements
To Nepal
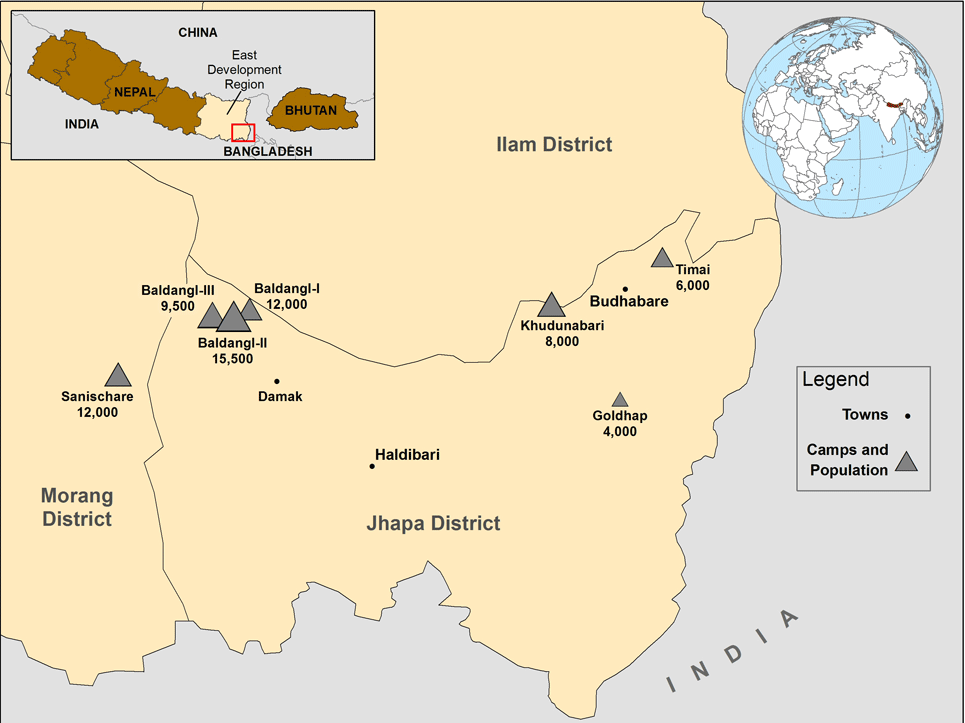
In the early 1990s, more than 100,000 ethnic Nepali left Bhutan and resettled into seven refugee camps in southeast Nepal: Beldangi I, Beldangi II, Beldangi II extension, Goldhap, Khudunabari, Timai (all in Jhapa District), and Sanischare (Morang District) near the township of Damak (Figure 2). Nearly all Bhutanese refugees in Nepal reside in these refugee camps, as opposed to an urban setting. In 2006, the United States and other governments began to offer resettlement to Bhutanese refugees living in these camps. 2 As of early 2012, more than 49,000 Bhutanese refugees have been resettled to the United States. 8 Smaller numbers have been resettled to Australia, Canada, and other countries. Since 2006, the camp population decreased by nearly 40%, but as of 2011, approximately 67,000 refugees remain, including 5,800 children under 5 years of age. Due to the decline in camp populations, in February 2011, the Nepalese government expressed the intent to consolidate the camps into two settlements. Of the seven original camps, two (Timai and Goldhap) have been closed and the remaining population moved to Beldangi and Sanischare. The last camp of the Eastern group, Khudunabari, will be relocated in March–May, 2012. Three Beldangi camps (Beldangi I, II, and II extension) are now collectively named Beldangi (though all three remain), and Sanischare remains. By the end of May 2012, there will be two official camps – Beldangi (three camps in one) and Sanischare. 5
Figure 2. Location and size of Bhutanese refugee camps in Nepal (April, 2011)
To the United States
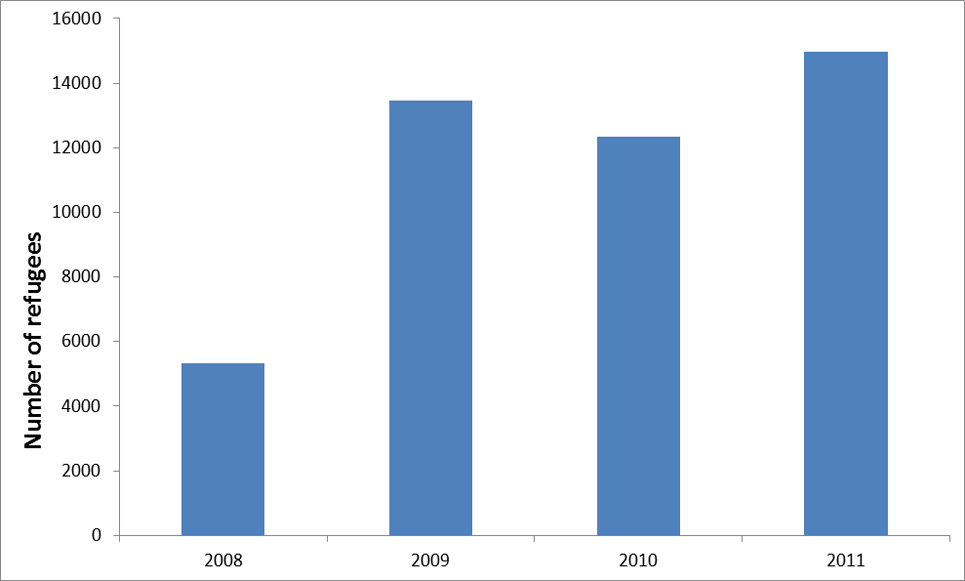
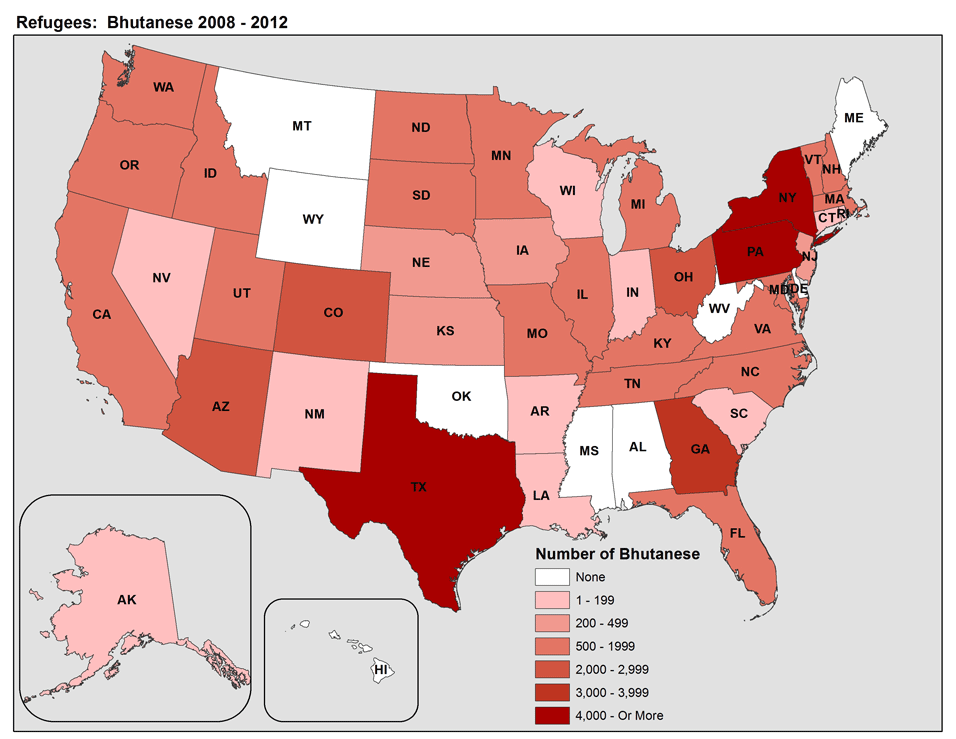
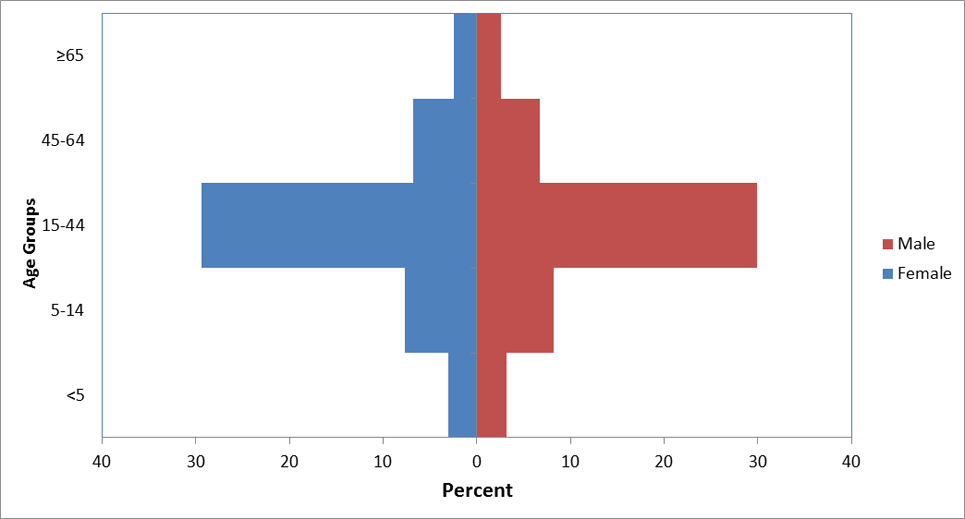
From 2008 to 2011, between 5,000 and 15,000 Bhutanese refugees arrived annually in the United States (Figure 3). A similar number is anticipated in 2012 as the United States “remains committed to considering for resettlement as many refugees as express interest”. 7 Refugees have been resettled to 41 states, with Pennsylvania, Texas, New York, and Georgia each receiving ≥ 7% of total arrivals (Figure 4). 8 However, once refugees arrive in a state, they are free to relocate elsewhere, and secondary migration to join an already established Bhutanese community is common. Most (60%) Bhutanese refugees resettled to the United States are young adults aged 15–44 years, 15% are 45–64 years old, 5% are 65 years or older, and the remainder are children under 15 years old (Figure 5).
Figure 3: Bhutanese refugee arrivals to the US, FY 2008-FY 2011 (N=46,069)
Figure 4: State of primary resettlement for Bhutanese refugees, FY 2008-FY 2012 (N=49,010)
Table 1: Top 10 States of primary resettlement for Bhutanese refugees
| Top 10 States | Number | Percent (%) |
|---|---|---|
| Pennsylvania | 4909 | (10.0) |
| Texas | 4873 | (9.9) |
| New York | 4000 | (8.1) |
| Georgia | 3446 | (7.0) |
| Ohio | 2335 | (4.7) |
| Arizona | 2329 | (4.7) |
| Colorado | 2117 | (4.3) |
| Washington | 1944 | (3.9) |
| Virginia | 1883 | (3.8) |
| North Carolina | 1671 | (3.4) |
* The remaining 19,503 refugees resettled to 31 other states. Source: WRAPS
Figure 5: Demographic characteristics of Bhutanese refugees resettled to the United States, 2008-2011 (N=48,846)
Healthcare and Diet in Camps
The Association of Medical Doctors of Asia (AMDA)-Nepal, a non-governmental organization, provides inpatient and outpatient medical care and community health education in all refugee camps in Nepal. UNHCR collects health information in refugee camps and reports this information in their Health Information System (HIS). Much of the camp-level information in this profile comes from HIS. Services include pediatrics and integrated management of childhood illness, reproductive health, psychiatric consultation, emergency medical services and referrals, basic laboratory services, tuberculosis (TB) management (Directly Observed Therapy with first-line agents), voluntary testing and counseling for human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS) with referral services for antiretroviral treatment, and nutrition promotion.
Immunizations
AMDA-Nepal also provides routine immunizations in the camps (Table 1).
Table 1: Routine immunizations provided in Bhutanese refugee camps in Nepal
| Routine immunizations provided in Bhutanese refugee camps in Nepal | ||
|---|---|---|
| Vaccine | Number of doses | Age at Administration |
| Bacille Calmette Guerin (BCG) | One | Newborn to 1 month |
| Diphtheria, Pertussis, Tetanus (DPT) | Three | 6, 10, and 14 weeks |
| Hepatitis B | Three | 6, 10, and 14 weeks |
| Haemophilus influenzae type b (Hib) | Three | 6, 10, and 14 weeks |
| Measles | One | 9 months |
| Oral Polio Vaccine (OPV) | Three | 6, 10, and 14 weeks |
| Tetanus Toxoid (TT) | Two (one month apart) | Pregnant women (2nd trimester) |
Source: International Organization for Migration (IOM)
Precise estimates of vaccine coverage are difficult to obtain because the number of people living in in the camps is inexact. However, the best available data indicate the following (Source: HIS 2008- 2011):
- Bacille Calmette Guerin (BCG) for TB: 94%
- Diphtheria, Pertussis, and Tetanus (DTP): 95%
- Measles: 98%
- Polio: 94%
Supplemental mass immunization campaigns are also carried out by AMDA-Nepal and other non-governmental organizations following announcements from the government of Nepal. These include polio and Japanese encephalitis campaigns conducted approximately once a year for children younger than 5 years of age and vitamin A and anti-intestinal parasite campaigns 1–2 times a year for children younger or equal to 13 years of age.
Reproductive Health
In Bhutanese refugee camps, prenatal care coverage is approximately 91-97% including antenatal tetanus toxoid administration. 6 Contraception and family planning services are also widely used and accepted. However, most Bhutanese refugee women have never had a mammogram or Pap smear. 1 They may not feel comfortable discussing sexuality and gynecological issues with non-family members, especially male clinicians.
Gender-Based Violence
Sexual assault, rape, trafficking, polygamy, domestic violence, and child marriage have all been reported in the camps. Domestic violence is probably the most pervasive form of gender-based violence suffered by Bhutanese refugees. 9
Diet and Rations
Food rations are provided by the World Food Programme (WFP) and UNHCR. They consist of rice, lentils, chickpeas, vegetable oil, sugar, salt, and fresh vegetables.23 Only certain refugees, including young or malnourished children, pregnant and lactating women, and infectious tuberculosis patients, receive additional rations and multivitamin supplements. A locally made, fortified, blended food containing micronutrients (called “Unilito”) is included in the rations but is not consumed regularly by all refugees. 10 Additional foods are available for purchase at markets outside the refugee camps, but the refugees often lack resources to purchase these products. The frequency of consumption of these foods, including meat and dairy products, appears to be highly variable among refugees. 10 Vegetarianism is relatively rare (6%) but frequency of meat consumption is low. Hindu refugees (approximately 60% of the population) generally do not consume beef or buffalo. 10
The results of a survey conducted in 2007 showed that only 4.9% of mothers exclusively breastfed their children up to 6 months, and 76.1% introduced other liquids to their children aged 3 months or less. 11 Bhutanese refugee children aged 6–59 months receive packages of a micronutrient powder called Vita-Mix-It that is designed to be mixed with meals after cooking. Distributed monthly to be consumed every two days, Vita-Mix-It provides an average of 50% of the Recommended Nutrient Intake (RNI) for children 1–3 years of age. 12
Medical Screening of US-Bound Refugees
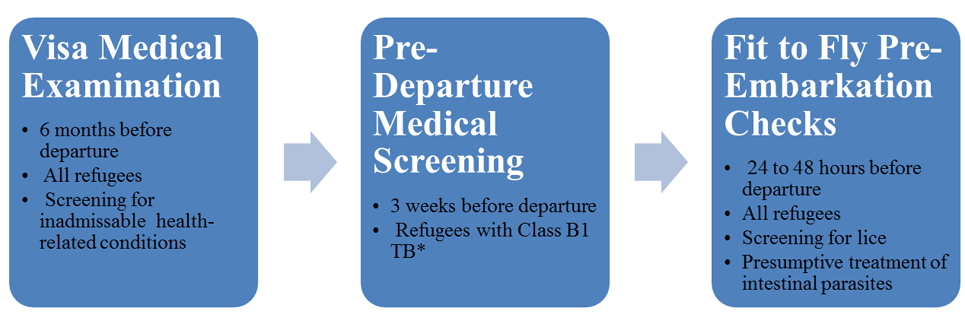
Bhutanese refugees who have been identified for resettlement to the United States receive additional medical assessments (Figure 6). Some assessments occur several months prior to departure and some occur immediately before departure to the US.
Figure 6: Medical assessment of US-Bound Bhutanese refugees
Visa Medical Examination
A visa medical examination is mandatory for all refugees coming to the United States and must be performed according to the CDC’s Technical Instructions for visa medical examinations. The purpose of the medical examination is to identify applicants with inadmissible health-related conditions. These examinations are performed by panel physicians who are selected by Department of State (DOS) consular officials. CDC provides the technical oversight and training for the panel physicians. In Nepal, all panel physicians work for the International Organization for Migration (IOM). Information collected during the refugee visa medical examination is reported to CDC’s Electronic Disease Notification System (EDN) and is available to state health departments where the refugees are resettled.
Unlike immigrant visa applicants, vaccination requirements do not apply to refugees at the time of their initial admission to the United States. However, currently one dose of each of the vaccines in Table 2 is offered to Bhutanese refugees of the appropriate age group during the visa medical examination.
Table 2: Vaccinations offered to US-bound Bhutanese refugees during the visa medical examination
| Vaccine | Age group |
|---|---|
| Oral Poliovirus (OPV) | 2 months–11 years |
| Diphtheria, Pertussis, and Tetanus (DTP) | 2 months–11 years |
| Tetanus and Diphtheria (Td) | ≥ 11 years |
| Measles, Mumps, and Rubella (MMR) | ≥ 1 year to adults born after 1957 |
| Hepatitis B Virus (HBV) | Zero–18 years |
Source: IOM
Pre-Departure Medical Screening
In Nepal, a pre-departure medical screening is conducted about three weeks before departure for the United States for refugees previously diagnosed with class B1 TB (TB fully treated using Directly Observed Therapy, or abnormal chest x-ray with negative sputum smears and cultures, or extrapulmonary TB). The screening includes a repeat physical examination with a focus on TB signs and symptoms, chest x-ray, and sputum collection.
Pre-Embarkation Checks
IOM clinicians perform two pre-embarkation checks within 48 hours of the refugee’s departure to the United States to assess fitness for travel and administer presumptive therapy for intestinal parasites (worms). The first pre-embarkation check is conducted in Damak, one day prior to travel from Damak to Kathmandu. To combat intestinal parasites, all refugees aged ≥2 years receive a single 400 mg dose of albendazole (since February 2012) and children aged 12–23 months receive a single 200 mg dose of albendazole. Chronically ill refugees receive a 4-week supply of their prescription medications. The second pre-embarkation check is performed in the Kathmandu transit center one day before departure from Kathmandu for the United States, primarily to ensure that refugees are fit to fly. Both checks also include screening and treatment for head lice infestation, as needed.
Surveillance
Communicable diseases of public health significance (such as TB), especially as relates to safe travel, are identified during active surveillance through all phases of overseas medical processing. This surveillance is designed to identify refugees with conditions that may result in deferred travel or other interventions, if they are transmissible. In addition, when disease outbreaks occur in the camps, IOM coordinates with AMDA-Nepal to identify refugees in the resettlement program who may be affected. Depending on the nature of the disease outbreak, various interventions may then be employed, such as deferral of travel, additional vaccinations, and/or presumptive or directed therapy.
Post-Arrival Medical Screening
Once refugees have arrived in the US, CDC recommends that they receive a post arrival medical screening (domestic medical screening) within 30 days after arrival. The Office of Refugee Resettlement (ORR) reimburses providers for screenings conducted during the first 90 days after arrival. The purpose of these more comprehensive examinations is to identify conditions that may have been missed during visa medical examinations and to serve as an introduction to the US healthcare system. CDC provides guidelines and recommendations and state health departments oversee and administer the domestic medical screenings. Health departments and private physicians conduct the examinations themselves. Health departments determine who conducts the examinations within their jurisdiction. Data from the screenings are collected by most state health departments.
Health Information
In general, the health and nutrition status of Bhutanese refugees is better than that of the typical Nepalese citizen 13. Mortality and acute malnutrition rates are well below emergency thresholds.
The following rates are calculated based on data collected from 2008–2011 in camps in Nepal, except where noted.
Mortality rates 2008–2011
| Type of Rate | Rate per Population | Bhutanese in Nepal * | General US Population Rates |
|---|---|---|---|
| Crude Birth Rate | per 1,000 population | 17.5 | 13.5 ** |
| Crude Mortality Rate | per 100,000 population | 416 | 794 *** |
| Under 5 Mortality Rate | per 100,000 population | 479 | 620 (< 1 year) 26 (1-4 years) |
Sources: Mortality rates 2008–2011
Communicable Disease
Malaria
Routine malaria screening is not conducted during overseas or domestic medical assessments; screening is based on the presence of signs or symptoms of disease. During the required visa medical examinations, 1.6% of refugees reported a history of malaria infection. 14The crude (all ages) incidence of confirmed malaria infection was 0.16 cases per 1,000 population per month, while the suspected malaria (not laboratory confirmed) incidence was ten times higher at 1.6 cases per 1,000 population per month. The incidence of confirmed malaria infection in children under 5 years old was 0.06 cases per 1,000 population per month, while the suspected malaria incidence was 0.4 cases per 1,000 population per month.
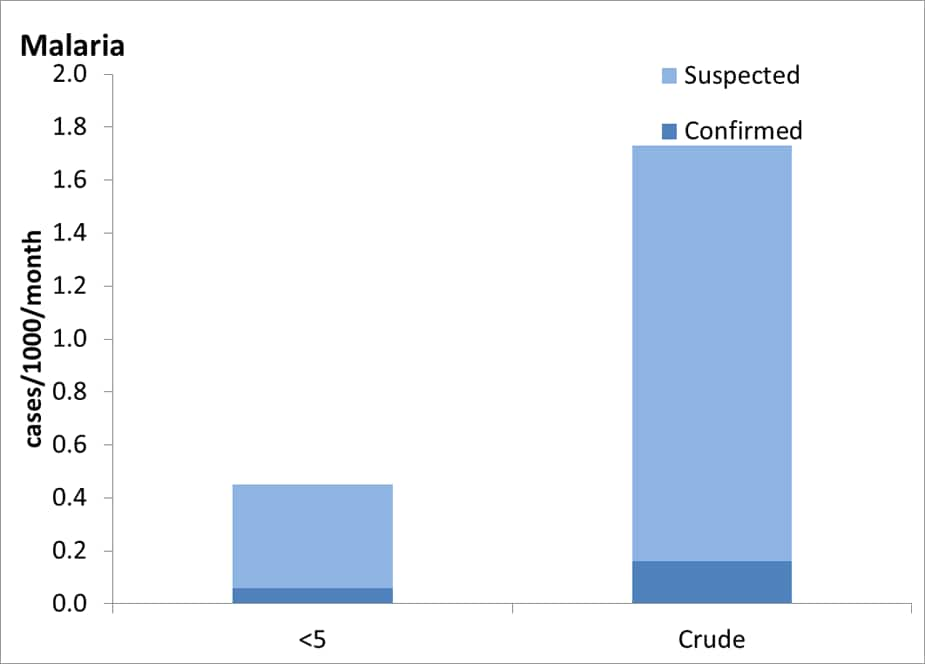
For children under 5 years old there were approximately 0.5 suspected cases of malaria per 1000 population per month and approximately 0.1 confirmed cases of malaria per 1000 population per month. For all ages there were approximately 1.5 suspected cases of malaria per 1000 population per month and approximately 0.3 confirmed cases of malaria per 1000 population per month.
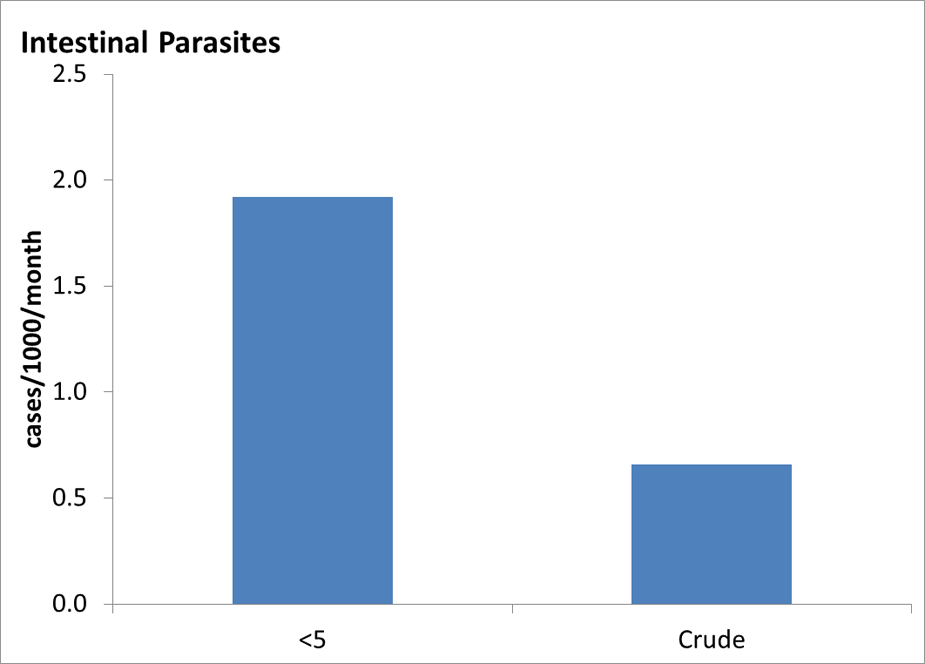
Intestinal Parasites
As mentioned, resettling refugees > 1 years of age receive 400 mg of albendazole 48 hours prior to departure for the United States as a presumptive treatment for helminthiasis. Approximately 20% of new arrivals into Texas between June 2009 and May 2011 had positive ova and parasite stool samples during post-arrival screening exams. 15 Of 295 records that specified a parasite, more than 50% were positive for Giardia, 36% for Dientamoeba, 20% for Entamoeba, and 2% or less for Ascaris, Clonorchis, hookworm, Schistosoma, Strongyloides, and Trichuris. On serological tests, a more sensitive means of detecting Schistosoma and Strongyloides infection, of 272 refugees tested, 20% were positive for Strongyloides while only 2% of 64 tested were positive for Schistosoma. 15
Tuberculosis
Of more than 44,000 refugees screened for active TB during visa medical examinations conducted by IOM in Nepal, fewer than 400 (0.8%) were sputum smear or culture positive for Mycobacterium tuberculosis. Of those who were culture positive and submitted for drug susceptibility testing, nearly 90% were pansusceptible, fewer than 4% were isoniazid (INH) resistant, approximately 2% were monoresistant to a drug other than INH or rifampin, fewer than 2% were poly-resistant but not multi-drug resistant (MDR), and fewer than 1% were MDR TB. 5
Approximately 8% of Bhutanese refugees arrive in the United States with a class B1 TB designation (TB fully treated using Directly Observed Therapy, or abnormal chest x-ray [CXR] with negative sputum smears and cultures, or extrapulmonary TB). Of these, fewer than 1% had extrapulmonary TB.
During the visa medical examinations, tuberculin skin tests (TST) are routinely performed on children aged 2–14 years (whereas all adults receive chest x-rays). Children who have a positive TST and latent TB infection are designated as TB class B2. Approximately 8% of children examined by IOM in Nepal during 2008–2011 had a positive TST with >10 mm induration. Adult contacts of infectious TB case-patients are also screened using a TST. Of 357 adult contacts screened by IOM in Nepal, 1.1% were classified with class B2 TB]. 15 During post-arrival screening exams inTexas, however, all refugees (adults and children) are administered either a TST or interferon-gamma release assay (IGRA) test. Of these refugees, 22% of 569 children aged 2–14 years had a positive TST or IGRA while 48% of 1,905 adults aged 15 years and over had a positive TST or IGRA.
Hansen’s Disease
Hansen’s disease (leprosy) is endemic in Nepal. Visa medical examinations include a search for symptoms and lesions consistent with Hansen’s disease. During screening exams conducted by IOM panel physicians in Nepal, fewer than 0.1% of Bhutanese refugees reported a history of Hansen’s disease. 15 During 2008–2011, four Bhutanese refugees arrived in the United States with a class B designation for Hansen’s disease. A class B designation is given to refugees who either received six months of treatment for the lepramatous or borderline (dimorphous) form of Hansen’s disease with a satisfactory clinical response, or were diagnosed with the indeterminate or tuberculoid form of the disease.
Infectious Hepatitis
Upon arrival in Texas, 1.3% (33/2558) of refugees screened in June 2009–May 2011 had chronic infection with hepatitis B as indicated by detectable serum hepatitis B surface antigen. 15 Of those who tested negative for hepatitis B surface antigen, 24% demonstrated hepatitis B core and/or surface antibody indicating some degree of immunity; 2.7% were positive for both hepatitis B core and surface antibodies indicating clearance of natural infection, 20% of refugees demonstrated only surface antibodies most likely due to past vaccination, and 1.4% had only positive core antibodies, most likely indicating clearance of past infection (although this can also be due to low-level chronic infection, resolving acute infection, or false positive test). It should be noted that a positive hepatitis B surface antibody may be positive if measured after the first or second dose of vaccination and does not necessarily indicate long-term immunity. Refugees generally do not receive the full hepatitis B series prior to migration.
Approximately 45% of Bhutanese refugees resettled in one large resettlement state in June 2009–May 2011 tested positive for hepatitis A antibodies, indicating previous exposure. 15 There are no data available on the prevalence of infectious hepatitis in the camps in Nepal.
HIV & Syphillis
Overseas screening for HIV infection has been discontinued as a requirement for US immigration since January 2010. Testing is offered to refugees by many state health departments. If a refugee is known to have TB, this is documented in their medical examination paperwork and they are listed as class B-Other HIV. Among more than 2000 Bhutanese refugees screened in Texas between 2008–2011, fewer than 0.5% were positive for HIV infection. 15
Syphilis screening is still a visa medical examination requirement and treatment is provided to those who test positive. Less than 0.5% of Bhutanese refugees tested positive for syphilis during post-arrival screening exams in Texas. 15
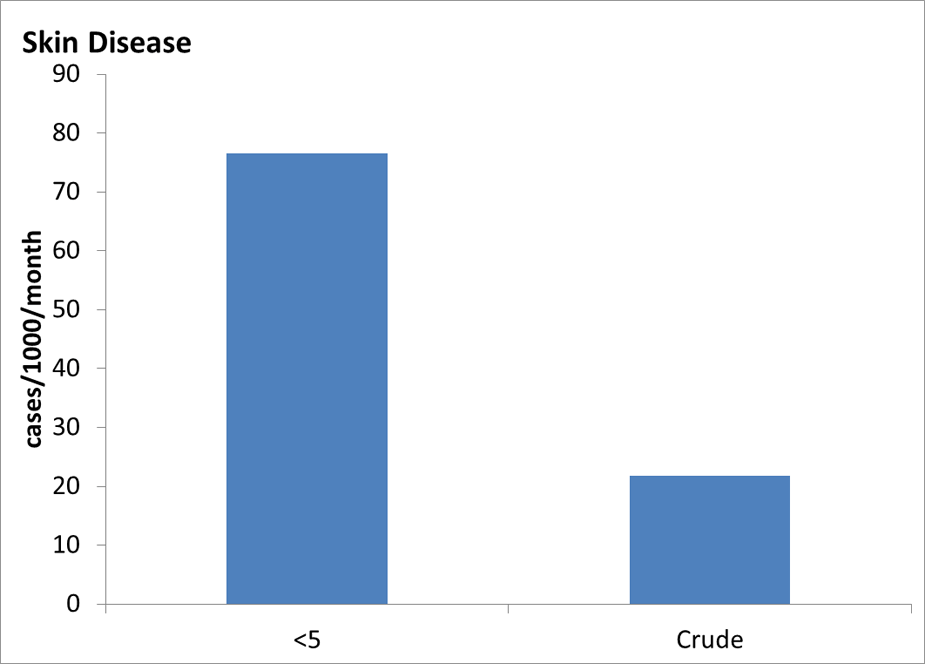
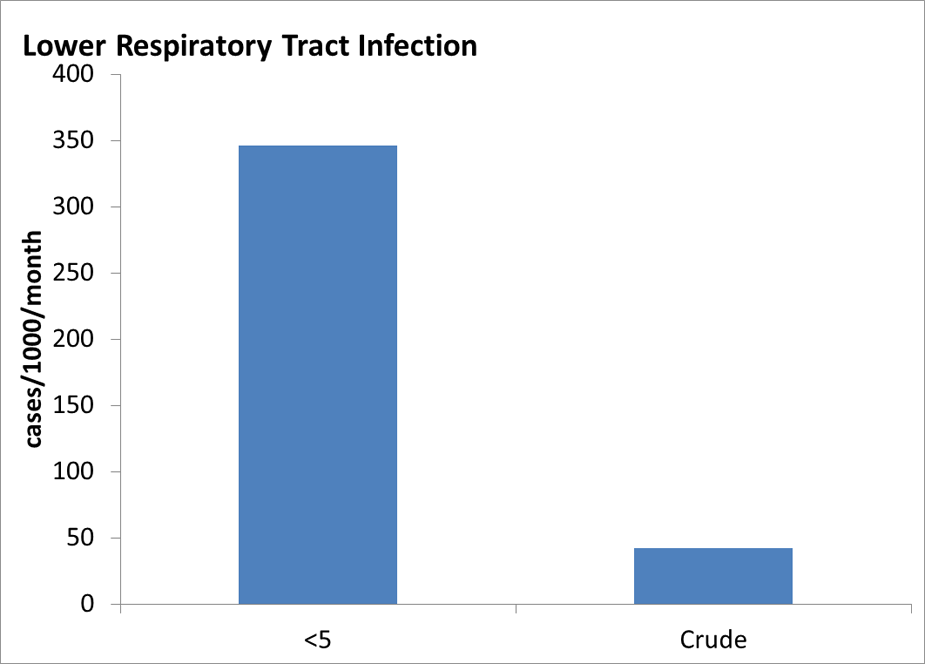
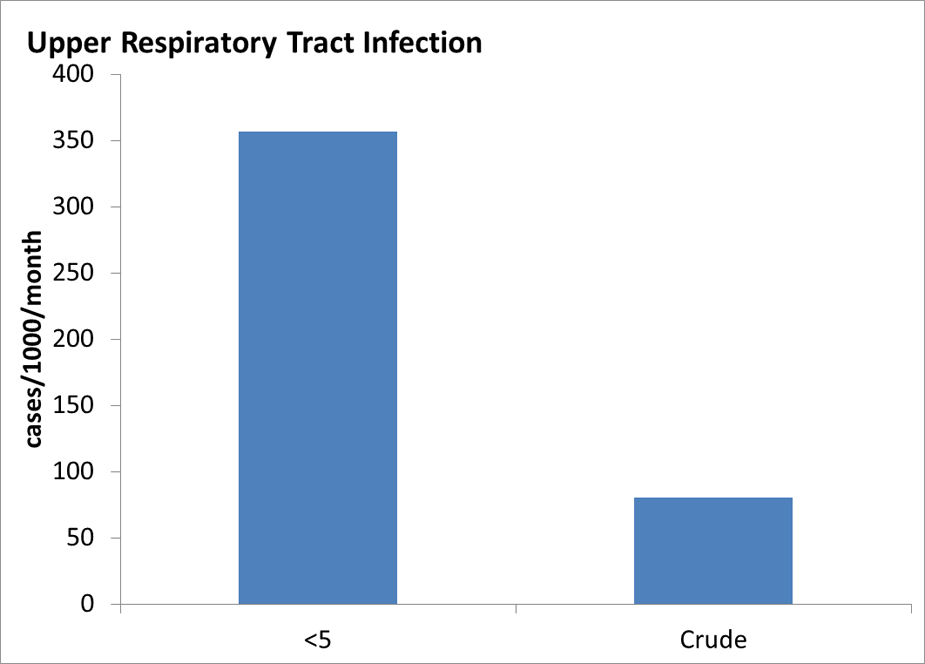
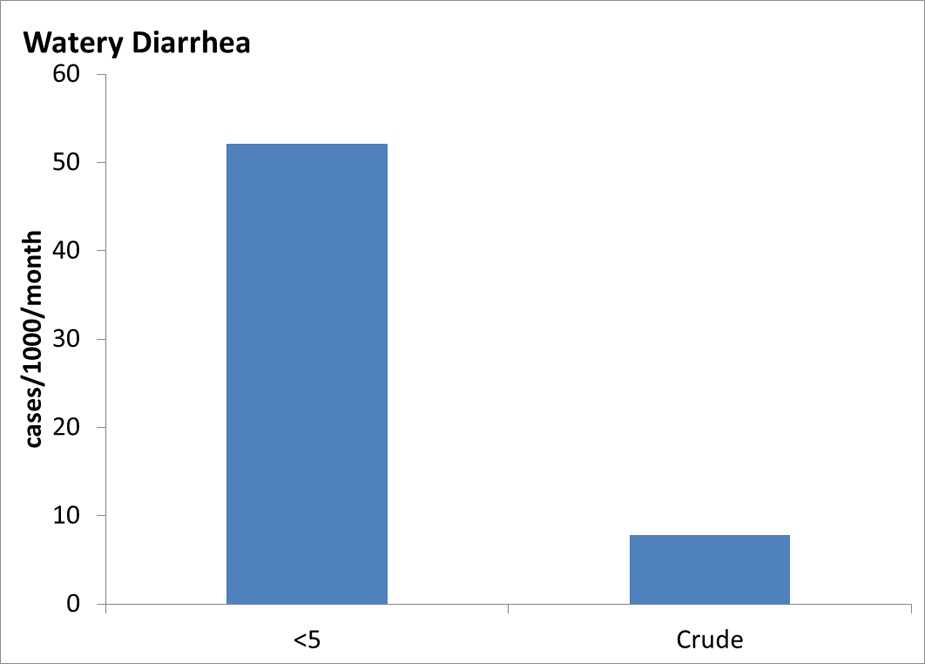
Additional Communicable Disease Graphs
Under 5 years old and Crude (all ages) Incidence Rates of Communicable Disease Conditions in Bhutanese Refugee Camps in Nepal 2008-2011
Non-Communicable Disease
Hypertension
Blood pressure is measured during the visa medical exam and during post-arrival screening exams in the United States. Although two or three measurements are required to diagnose an individual with hypertension, single measurements may be used to estimate prevalence of hypertension in a population. The prevalence of high blood pressure increases with age among Bhutanese refugees, as expected; however, the estimated rate of hypertension in adults over the age of 65 (15%) is much lower than that seen in the same age group in the United States (>65%). 16 Three percent of applicants reported a history of hypertension during their visa medical examination (Table 4).
Table 4: Self-Reported Non-Communicable Health Conditions and Tobacco use During Visa Medical Examinations Among US-Bound Bhutanese Refugees, 2008 – 2011
| Non-Communicable Health Condition | Percent |
|---|---|
| Hypertension | 3.0% |
| Asthma | 0.5% |
| Chronic obstructive pulmonary disease (emphysema) | 0.7% |
| Seizure disorder | 0.7% |
| Major impairment in learning, intelligence, self-care, memory, or communication | 0.8% |
| Major mental disorder including major depression, bipolar disorder, schizophrenia, mental retardation | 1.2% |
| Diabetes mellitus | 0.7% |
| Thyroid disease | 0.2% |
| Visible disabilities including loss of arms and legs | 0.5% |
| History of tobacco use | 6.5% |
| Current tobacco use | 4.8% |
Note: Other conditions including angina pectoris, cardiac arrhythmia, congenital heart disease, history of stroke with current impairment, drug addiction, or other substance-related disorders including alcohol addiction, malignancy, chronic renal disease, and chronic liver disease were reported by less than 0.2% of applicants. Source: EDN
Lead Poisoning
Bhutanese refugee children do not appear to be at higher risk of lead poisoning than US. children. Only 1.3% of Bhutanese children ≤16 years of age screened in one large resettlement state during 2008–2011 had elevated blood lead levels (≥10 ug/dL). In general, refugee children are thought to be at higher risk for lead poisoning, not only because anemia and malnutrition increase lead absorption but also because of an increased risk for exposure to products containing lead. 21
Nutrition
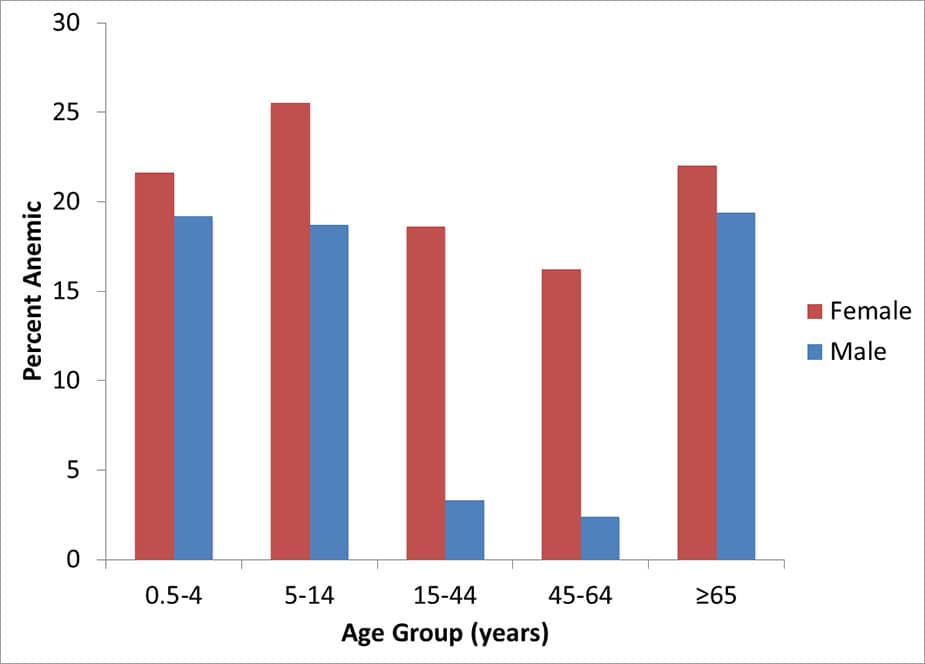
Anemia
Anemia is a common condition among Bhutanese refugees, reflecting global rates among people of a similar age and gender. 17 Approximately 20% of children under 15 as well as 20% of refugees aged 65 and older were anemic upon arrival in Texas in June 2009–May 2011 (Figure 8). 15 The prevalence of anemia in women of reproductive age is approximately 19% while pregnant women have an anemia prevalence of 28%. 15 The most common cause of anemia is due to iron deficiency but a number of other conditions affecting Bhutanese refugees could play a contributory role, including malaria, intestinal parasites, deficiencies of vitamin B12 and other micronutrients, tuberculosis, hemoglobinopathies, and chronic disease. According to another survey administered to refugee children aged 6-59 months and their mothers in Nepali refugee camps in 2007, anemia was detected in 13.6% of mothers and 43.3% of children and decreased with age in children. 11
Figure 8: Anemia found in Bhutanese refugees during post-arrival screening examinations in one large resettlement state, June 2009–May 2011
Malnutrition
Limited food diversity, frequent illness, and feeding practices have been identified as underlying causes of malnutrition in the Bhutanese refugee population. 11 In 2007, acute malnutrition (i.e., wasting) was found in 4.2% of Bhutanese children aged 6–59 months living in camps in Nepal while chronic malnutrition (i.e., stunting) was found in 26.9% of children. 11 Similar rates of acute and chronic malnutrition were detected in Bhutanese refugee children resettling in Texas from 2008–2011 (5.7% and 22.8%, respectively). 15
Micronutrient Deficiencies
In addition to iron deficiency anemia, other micronutrient deficiencies have been identified among Bhutanese refugees. Vitamin B12 deficiency, a rare condition in the United States, was found in approximately 30-60% of Bhutanese refugees who resettled to the United States during 2008–2011 in an investigation conducted by CDC. 18 This high proportion was likely due to a lack of vitamin B12 in their diet in refugee camps in Nepal. Vitamin B12 deficiency can result in megaloblastic anemia, peripheral neuropathy, and other potentially permanent neurologic signs. All Bhutanese refugees should be given nutritional advice and should receive supplemental vitamin B12 upon arrival in the U.S. Other micronutrient deficiencies, including vitamin B2 (riboflavin), which results in high rates of angular stomatitis in adolescents, have been identified in this population. 19 A survey conducted in 1999 demonstrated vitamin A deficiency in 30% of Bhutanese refugee adolescents. 20
Obesity
The prevalence of obesity in Bhutanese refugees (defined as BMI >30 kg/m2 in adults > 15 years old or BMI > 95% in children 5–14 years of age), is much lower than that seen in the US population. 16 Obesity was observed in the following proportions of Bhutanese refugees screened in Texas from 2008-2011:
- 5-14 years: 2.1%
- > 15 years: 5.7%
Mental Health
Since 2009, there have been at least 16 suicides among the 49,010 Bhutanese refugees resettled to the United States. 1 Community leaders believe that isolation, substance abuse, domestic violence, depression, and resettlement issues may influence suicide attempts and other mental health-related decisions. 1 CDC and other partners are conducting an investigation to better understand the rate of Bhutanese suicides. Some refugees may have been tortured prior to fleeing Bhutan. Men are more likely to report having been tortured than women, but tortured women are more likely to report mental health conditions than tortured men. 22 According to IOM, of the 55,604 refugees examined during December 2007–December 2011, 1,694 (3.0%) were referred for psychiatric evaluation. The resulting diagnoses are described in Table 5.
Table 5: Prevalence of psychiatric conditions in Bhutanese refugees diagnosed during psychiatric referral as part of the visa medical examination in Nepal, 2008-2011(N=55,604)
| Psychiatric Conditions | Percent |
|---|---|
| Developmental disorders | 0.51% |
| Mood disorders, including bipolar disorder and major depression | 0.54% |
| Anxiety disorders (including PTSD) | 0.34% |
| Psychotic disorders, including schizophrenia | 0.31% |
| Somatoform disorders | 0.18% |
| Substance-related disorders, including alcohol abuse | 0.41% |
| Personality disorders | 0.1% |
| Adjustment disorders | 0.4% |
| Cognitive disorders | 0.5% |