Diagnoses of HIV Infection in the United States and Dependent Areas 2019: National Profile

All rates are per 100,000 population. The standard used for reporting trends in numbers and rates is an increase or a decrease of 5% or more during the specified time frame (e.g., when comparing 2015 and 2019). The exceptions to this standard are where numbers were small (i.e., less than 12) or rates were based on small numbers.
Please read all titles and footnotes carefully to ensure a complete understanding of the displayed data.
Figure 1. Rates of Diagnoses of HIV Infection among Adults and Adolescents, 2019—United States and 6 Dependent Areas
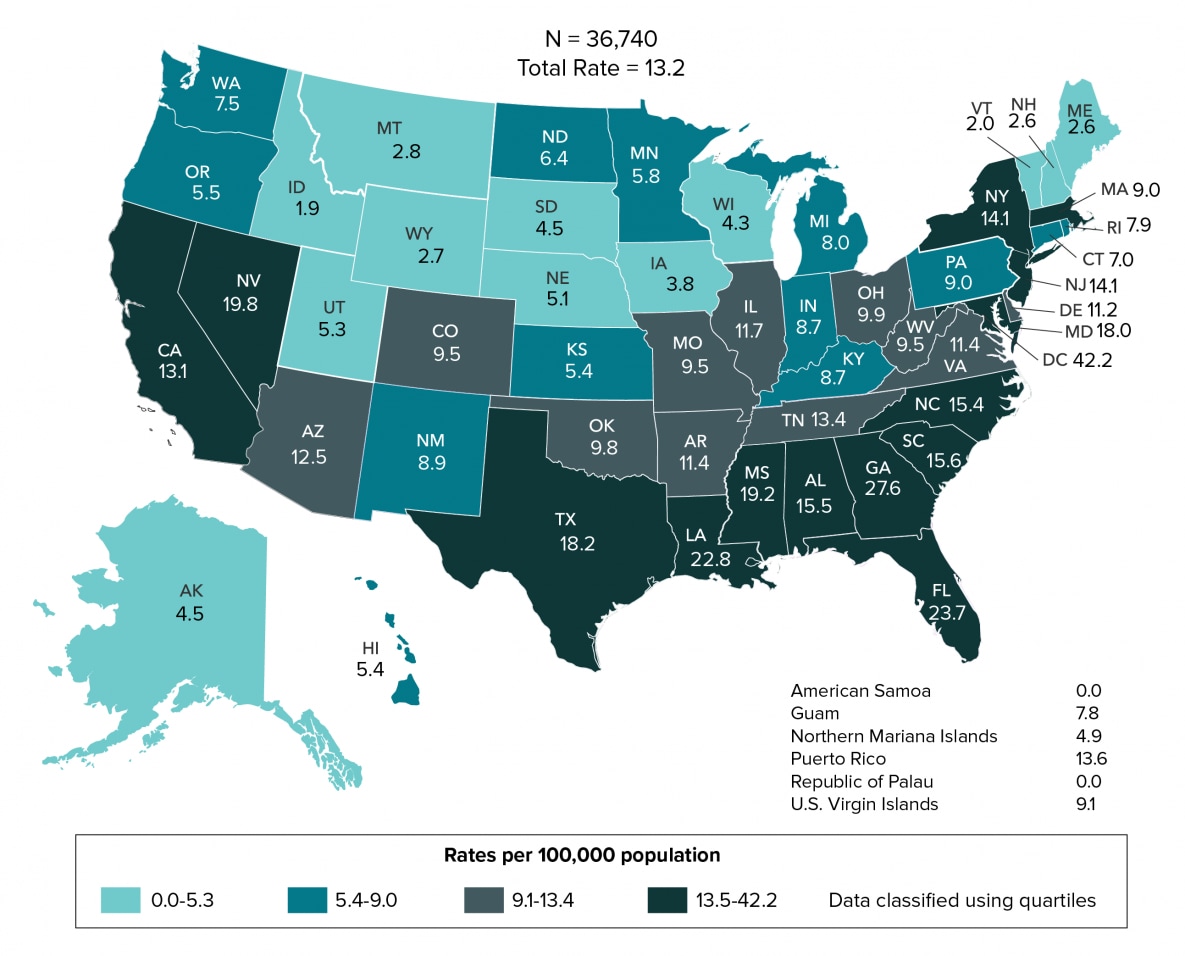
From 2015 through 2019, the annual number and rate of diagnoses of HIV infection in the United States and 6 dependent areas decreased (Table 1b). By region, the rate of diagnoses of HIV infection in all regions decreased. In 2019, the overall rate was 11.1; among adults and adolescents, the rate was 13.2 (Figure 1). By region, the rates were 15.2 in the South, 9.4 in the Northeast, 9.2 in the West, and 7.0 in the Midwest (Table 1b).
Gender: From 2015 through 2019 in the United States and 6 dependent areas, the number of diagnoses of HIV infection for transgender male-to-female (MTF) and transgender female-to-male (FTM) adults and adolescents increased (Figure 2). The number of diagnoses among male and female adults and adolescents decreased. In 2019, diagnoses of HIV infection among all males (79%) and females (19%) accounted for approximately 98% of HIV diagnoses (Table 1b). Transgender MTF accounted for slightly more than 1% of annual diagnoses and transgender FTM accounted for less than 1%. Please use caution when interpreting data for additional gender identity (AGI) adults and adolescents: the numbers are small.
Figure 2. Diagnoses of HIV Infection among Adults and Adolescents, by Gender, 2015–2019—United States and 6 Dependent Areas
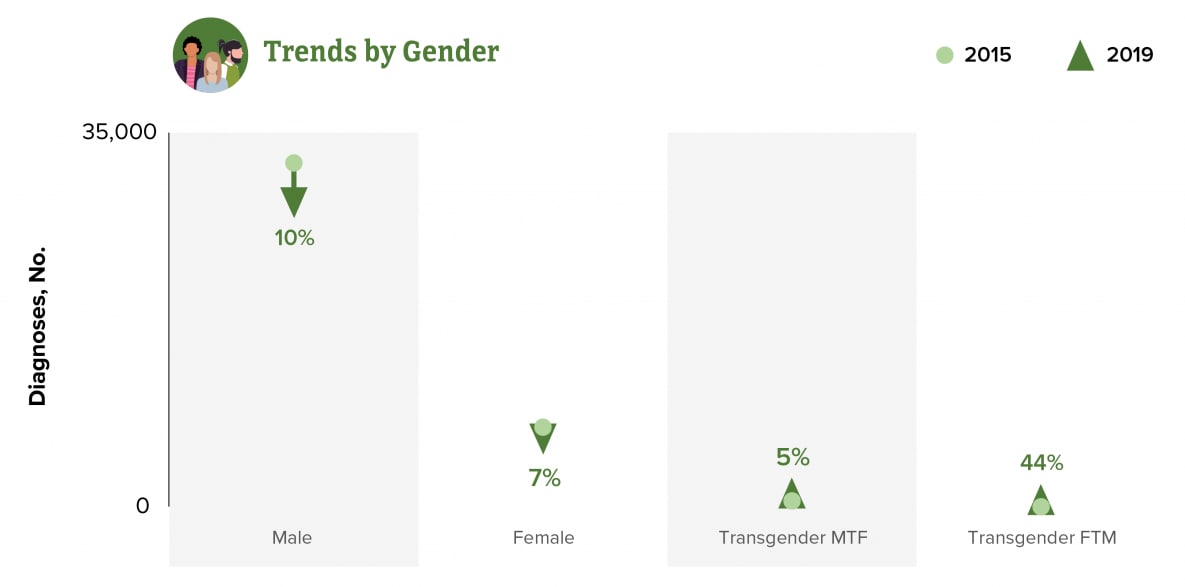
Note: See section D2.2 in the Technical Notes for more information on gender.
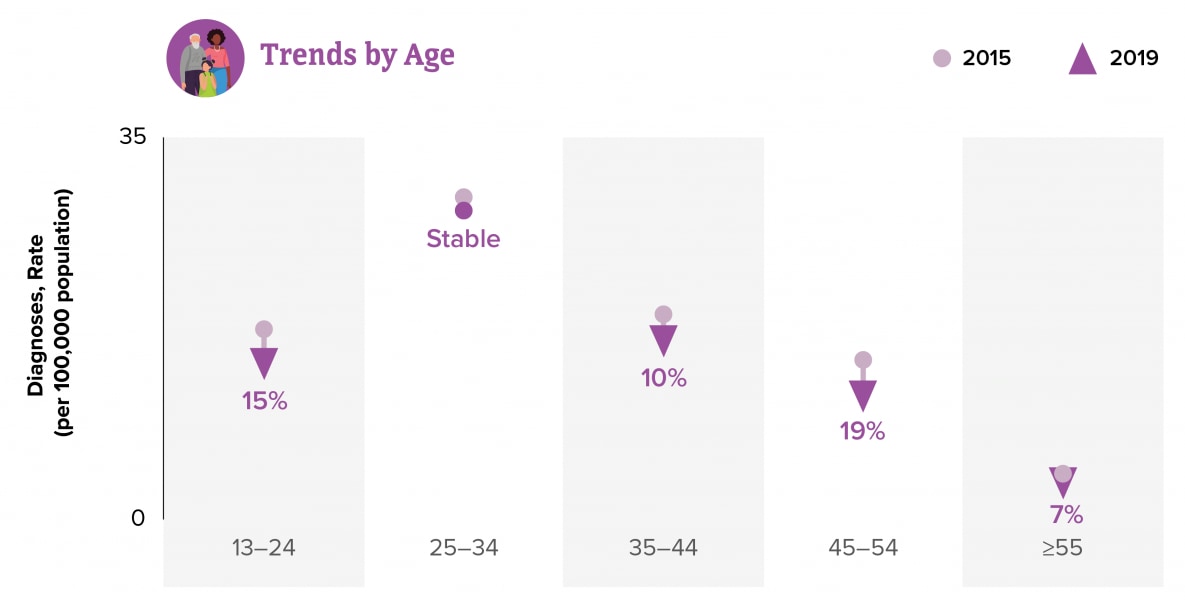
Age group: From 2015 through 2019 in the United States and 6 dependent areas, the rates for persons aged 13–24, 35–44, 45–54, and ≥55 years decreased. The rate for persons aged 25–34 years remained stable (Figure 3). Using smaller age groups, the rates for children (aged less than 13 years) and persons aged 13–14, 15–19, 20–24, 25–29, 35–39, 40–44, 45–49, 50–54, and ≥65 years decreased (Table 1b). The rates for persons aged 30–34, 55–59, and 60–64 years remained stable. In 2019, the highest rate (31.1) was for persons aged 25–29 years, followed by the rate (27.3) for persons aged 20–24 years (Table 1b).
Figure 3. Rates of Diagnoses of HIV Infection among Adults and Adolescents, by Age at Diagnosis, 2015–2019—United States and 6 Dependent Areas
Race/ethnicity: From 2015 through 2019 in the United States, the rate for diagnoses of HIV infection among American Indian/Alaska Native adults and adolescents increased (Figure 4). The rates of diagnoses of HIV infection for Asian, Black/African American, Hispanic/Latino, Native Hawaiian/other Pacific Islander, White, and multiracial adults and adolescents decreased. In 2019, the highest rate of diagnosis of HIV infection was 45.0 for Black/African American adults and adolescents, followed by 21.5 for Hispanic/Latino, 18.8 for multiracial, 13.5 for Native Hawaiian/other Pacific Islander, 10.5 for American Indian/Alaska Native, 5.3 for White, and 4.5 for Asian adults and adolescents.
Figure 4. Rates of Diagnoses of HIV Infection among Adults and Adolescents, by Race/Ethnicity, 2015–2019—United States
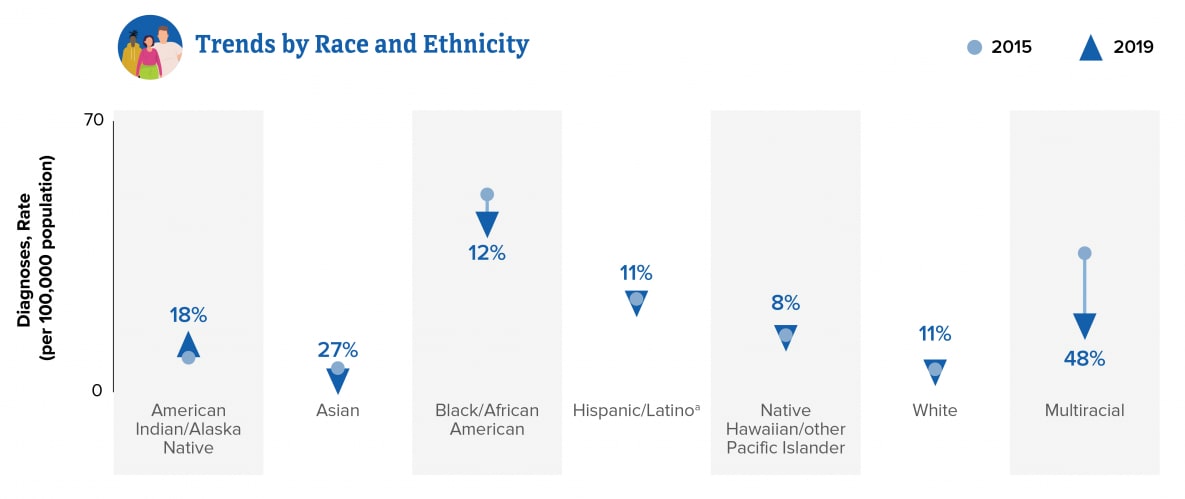
Note: See section D3 in the Technical Notes for more information on race/ethnicity. aHispanic/Latino persons can be of any race.
Sex (at birth) and Transmission category: From 2015 through 2019 in the United States and 6 dependent areas among all adults and adolescents, the annual percentage of diagnoses of HIV infection attributed to male-to-male sexual contact (MMSC) accounted for over 65% of diagnoses (Figure 5 and Table 1b). In 2019, diagnoses of HIV infections attributed to MMSC (approximately 70%, including 4% MMSC and injection drug use [IDU]) and those attributed to heterosexual contact (23%) accounted for approximately 93% of diagnoses in the United States (Figure 6). Among male adults and adolescents, the annual number of diagnosed HIV infections attributed to MMSC decreased and the number attributed to heterosexual contact decreased (Table 1b). The number of infections attributed to IDU and MMSC and IDU remained stable. The perinatal and “Other” transmission categories accounted for less than 1% of cases. Among female adults and adolescents, the number of infections attributed to IDU increased. The number of infections attributed to heterosexual contact decreased. The perinatal and “Other” transmission categories accounted for less than 1% of diagnoses.
Figure 5. Percentages of Diagnoses of HIV Infection among Adults and Adolescents, by Transmission Category, 2015–2019—United States and 6 Dependent Areas
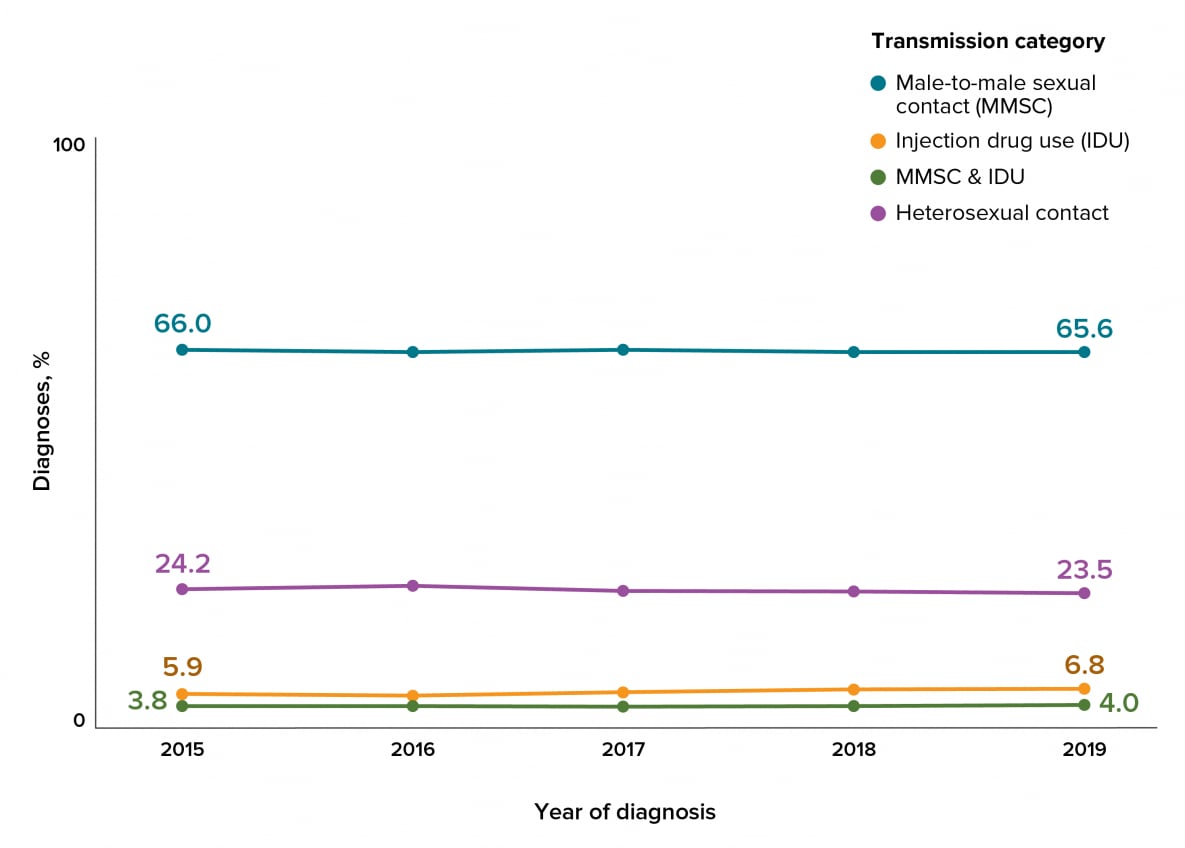
Note: Data have been statistically adjusted to account for missing transmission category. See section D4 in the Technical Notes for more information on transmission categories.
Figure 6. Diagnoses of HIV Infection among Adults and Adolescents, by Transmission Category, 2019—United States and 6 Dependent Areas
![cdc-hiv-surveillance-vol32-fig6 In 2019, diagnoses of HIV infections attributed to MMSC (approximately 70%, including 4% MMSC and injection drug use [IDU]) and those attributed to heterosexual contact (23%) accounted for approximately 93% of diagnoses in the United States.](/hiv/images/library/reports/hiv-surveillance/vol-32/cdc-hiv-surveillance-vol32-fig6.png)
Note: Data have been statistically adjusted to account for missing transmission category. See section D4 in the Technical Notes for more information on transmission categories.
Figure 7. Rates of Deaths of Persons with Diagnosed HIV Infection among Adults and Adolescents, 2019—United States and 6 Dependent areas
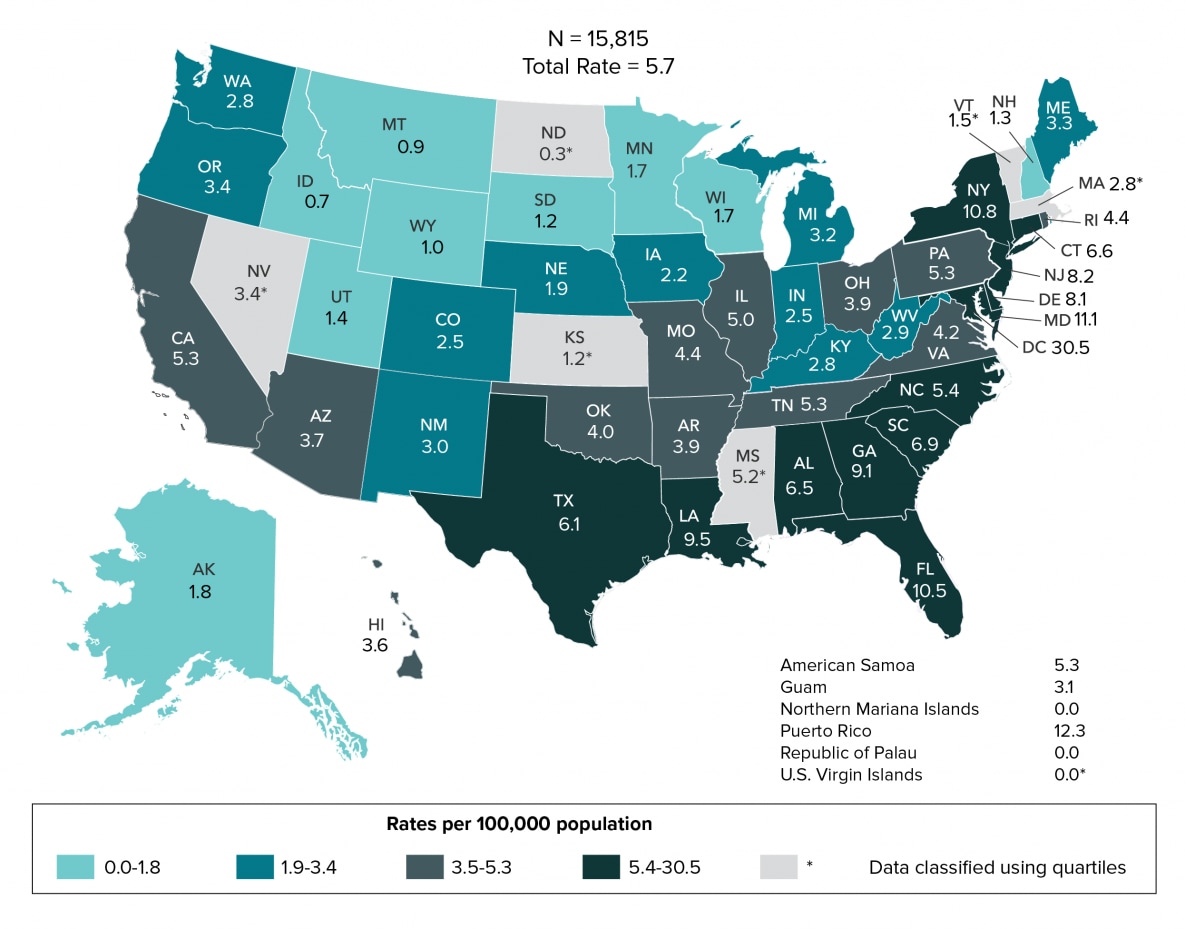
Note: Data for the year 2019 are preliminary and based on deaths reported to CDC as of December 2020. Data are based on address of residence as of December 31, 2019 (i.e., most recent known address). Asterisk (*) indicates incomplete reporting. See section C1.2 in Technical Notes for more information on deaths
From 2015 through 2019 in the United States and 6 dependent areas among persons with diagnosed HIV infection, the rate and number of deaths remained stable (Table 11b). By region, the rate of deaths in the South decreased; and remained stable in the Northeast, Midwest, and West. In 2019, the rate of deaths among adults and adolescents was 5.7 (Figure 7); and by region, rates were 6.2 in the Northeast, 6.0 in the South, 3.4 in the West, and 2.7 in the Midwest (Table 11b). Deaths of persons with diagnosed HIV infection may be due to any cause (i.e., may or may not be related to HIV infection). Data for the year 2019 are preliminary and based on deaths reported to CDC through December 2020.
Gender: From 2015 through 2019 in the United States and 6 dependent areas, the number of deaths for transgender MTF with diagnosed HIV infection increased (Table 11b). The number of deaths for females decreased, and the number of deaths for males remained stable. Please use caution when interpreting data for transgender FTM and AGI adults and adolescents: the numbers are small.
Age group: From 2015 through 2019 in the United States and 6 dependent areas, the rate of deaths for persons aged 60–64 and ≥65 years increased (Table 11b). The rates of deaths for persons aged 20–24, 25–29, 35–39, 40–44, 45–49, and 50–54 years decreased. The rates of deaths for persons aged 30–34 and 55–59 years remained stable. Please use caution when interpreting data for children (aged less than 13 years at death) and persons aged 13–14 and 15–19 years: the numbers are small.
Race/ethnicity: From 2015 through 2019 in the United States, the rates of deaths for Asian persons increased (Figure 8 and Table 11a). The rates of deaths for American Indian/Alaska Native, Black/African American, and multiracial persons decreased. The rates for Hispanic/Latino and White persons remained stable. In 2019, the highest rate of deaths (16.1) was for Black/African American persons (Table 11a). Please use caution when interpreting data for Native Hawaiian/other Pacific Islander persons: the numbers are small.
Figure 8. Rates of Deaths among Persons with Diagnosed HIV Infection, by Race/Ethnicity, 2015–2019—United States
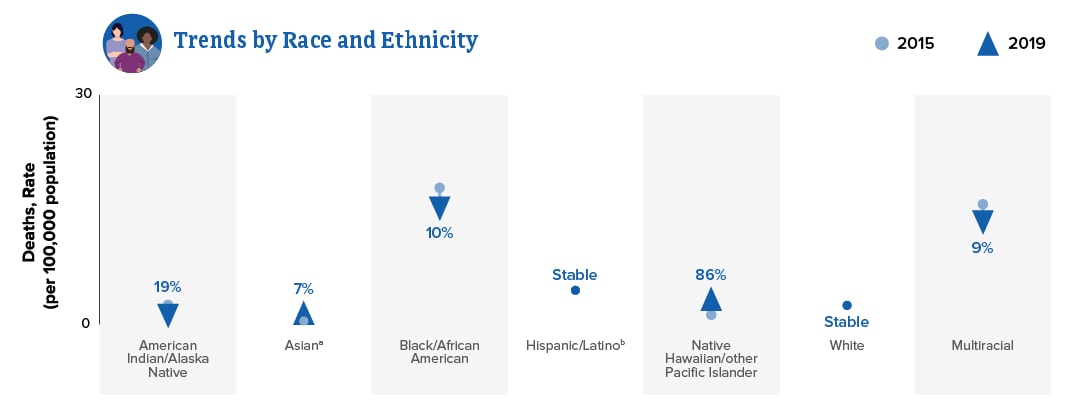
Note: See sections C1.2 and D3 in Technical Notes for more information on deaths and race/ethnicity.
aIncludes Asian/Pacific Islander legacy cases.
bHispanic/Latino persons can be of any race.
Sex (at birth) and transmission category: From 2015 through 2019 in the United States and 6 dependent areas, the overall rate of death among male adults and adolescents with diagnosed HIV infection remained stable (Table 11b). The number of deaths among male adults and adolescents with HIV attributed to perinatal transmission increased. The number of deaths among male adults and adolescents with HIV attributed to IDU or MMSC and IDU decreased. The number of deaths among male adults and adolescents remained stable for those with HIV attributed to MMSC and remained stable for those with HIV attributed to heterosexual contact. The perinatal and “Other” transmission categories accounted for less than 1% of diagnoses. Overall, the rate of deaths for female adults and adolescents decreased. The number of deaths among female adults and adolescents with infection attributed to IDU, perinatal transmission, and heterosexual contact decreased. The “Other” transmission category accounted for less than 1% of diagnoses.
Figure 9. Rates of Adults and Adolescents Living with Diagnosed HIV Infection, Year-end 2019—United States and 6 Dependent Areas
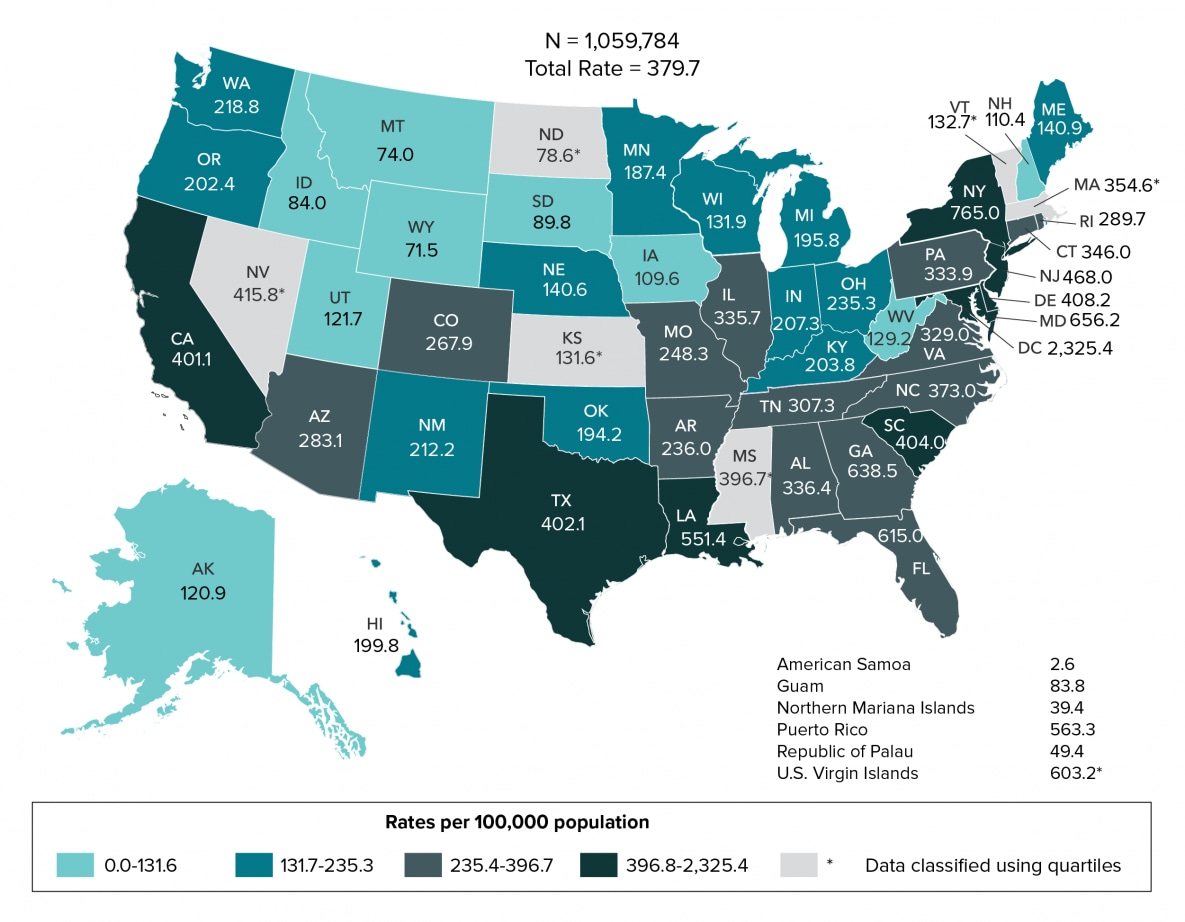
Note: Data for the year 2019 are preliminary and based on deaths reported to CDC as of December 2020. Data are based on address of residence as of December 31, 2019 (i.e., most recent known address). Asterisk (*) indicates incomplete reporting. See section C1.3 in Technical Notes for more information on prevalence.
From 2015 through 2019 in the United States and 6 dependent areas, the number and rate of persons living with diagnosed HIV infection increased (Table 15b). By region, the rates of persons living with HIV in the Midwest, South, and West increased. The rate in the Northeast remained stable. The largest percentage increase in the rate (10%) was in the Midwest (from 165.9 in 2015 to 183.3 in 2019). At year-end 2019 in the United States and 6 dependent areas, 1,061,482 persons were living with diagnosed HIV infection. The prevalence of diagnosed HIV infection was 319.9. By region, the rate was highest in the Northeast at 422.5, followed by 378.7 in the South, 265.1 in the West, and 183.3 in the Midwest. At year-end 2019 in the United States and 6 dependent areas among adults and adolescents only, the prevalence of diagnosed HIV infection was 379.7 (Figure 9). Data for the year 2019 are preliminary and based on deaths reported to CDC through December 2020.
Gender: From 2015 through 2019 in the United States and 6 dependent areas, the largest percentage increase (49%) in the number of persons living with diagnosed HIV infection was among AGI persons (Table 15b). At year-end 2019, the largest percentage (75%) of persons living with diagnosed HIV infection were male, followed by females (23%). (Table 15b). Transgender MTF accounted for 1%, and transgender FTM and AGI persons each accounted for less than 1% of persons living with diagnosed HIV infection.
Age group: From 2015 through 2019 in the United States and 6 dependent areas, the largest percentage increase (48%) in the rate of persons living with diagnosed HIV infection was among persons aged ≥65 years (from 145.5 in 2015 to 216.0 in 2019) (Table 15b). At year-end 2019, persons aged 55–59 years made up the largest percentage (15%) of persons living with diagnosed HIV. The highest rate (741.1) was among persons aged 50–54 years, followed by those aged 55–59 years (737.7), and those aged 45–49 years (577.2).
Race/ethnicity: At year-end 2019 in the United States, 1,044,977 persons were living with diagnosed HIV infection (Table 15a). The highest rate (1,027.5) and the largest percentage (40%) were for Black/African American persons, followed by rates of 673.1 for multiracial, 411.3 for Hispanic/Latino, 153.9 for White, 153.0 for Native Hawaiian/other Pacific Islander, 132.0 for American Indian/Alaska Native, and 82.3 for Asian persons.
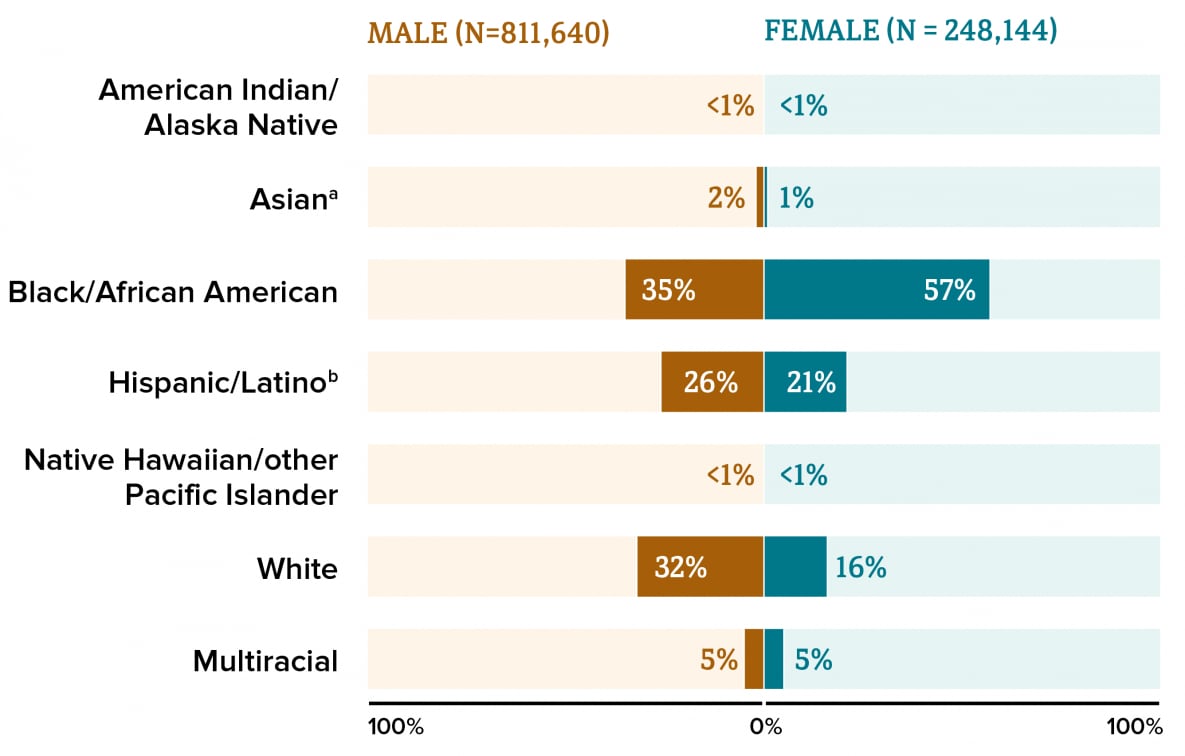
At year-end 2019 in the United States and 6 dependent areas, 1,059,784 adults and adolescents were living with diagnosed HIV infection (Figure 10). Among 811,640 adults and adolescents assigned male sex at birth living with diagnosed HIV infection, 35% were Black/African American, 32% were White, 26% were Hispanic/Latino, 5% were multiracial, and 2% were Asian. Less than 1% each were American Indian/Alaska Native and Native Hawaiian/other Pacific Islander male adults and adolescents. Among 248,144 adults and adolescents assigned female sex at birth living with diagnosed HIV infection, 57% were Black/African American, 21% were Hispanic/Latino, 16% were White, 5% were multiracial, and 1% were Asian. Less than 1% each were American Indian/Alaska Native and Native Hawaiian/other Pacific Islander female adults and adolescents.
Figure 10. Percentages of Adults and Adolescents Living with Diagnosed HIV Infection, by Sex at Birth and Race/Ethnicity, Year-end 2019—United States and 6 Dependent Areas
Note: Data for the year 2019 are preliminary and based on deaths reported to CDC as of December 2020. See section D3 in Technical Notes for more information on race/ethnicity.
aIncludes Asian/Pacific Islander legacy cases.
bHispanic/Latino persons can be of any race.
Sex (at birth) and Transmission Category: At year-end 2019 in the United States and 6 dependent areas, the rates were 594.9 for male adults and adolescents, 173.9 for female adults and adolescents, and 3.2 for children (aged less than 13 years) (Table15b). Among a total of 811,640 male adults and adolescents, 73% of infections were attributed to MMSC, 10% to heterosexual contact, 9% to IDU, 7% to MMSC and IDU, and 1% to perinatal transmission. Among a total of 248,144 female adults and adolescents, 77% of infections were attributed to heterosexual contact, 20% to IDU, and 2% to perinatal transmission. Among a total of 1,698 children (aged less than 13 years), 81% of infections were attributed to perinatal transmission.