
Monthy Case Studies - 1999
Case #13 - June, 1999
A 12-year-old boy from the Democratic Republic of Congo was diagnosed with malaria in a hospital in North Carolina. He had arrived in the United States three weeks earlier. Prior to his arrival, the boy spent three weeks in South Africa, and before that he was in the Democratic Republic of Congo. On examination of his blood smear, approximately 0.3% of the erythrocytes were found to be infected. Most (more than 97%) of the parasites observed were at the stage shown in Figures A through D. Some other parasite stages were also observed as shown in Figures E through I. What is your diagnosis? Based on what criteria?

Figure A
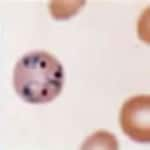
Figure B

Figure C

Figure D
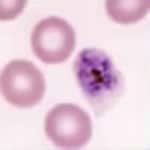
Figure E
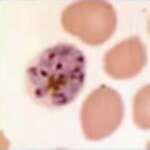
Figure F
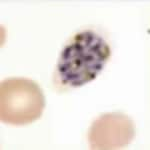
Figure G

Figure H
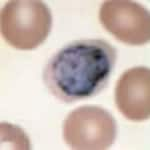
Figure I
Answer to Case #13
This was a case of malaria caused by Plasmodium ovale. However, the presence of P. falciparum rings could not be ruled out based on these images, alone. Figures A through D showed rings; Figures E through G showed schizonts; and Figures H and I showed gametocytes.
Diagnostic features observed were:
- fimbriated infected erythrocytes (Figures E through G); fimbriation is very suggestive of P. ovale.
- mature schizonts with a relatively small number of merozoites (8 to 12 merozoites in Figures E through G). The merozoites were rather large, well individualized, and on occasion nearly formed a "rosette" (Figures E and F). This presentation of schizonts is compatible with either P. ovale or P. malariae.
- enlarged infected erythrocytes (up to 1½×), some with a hint of Schüffner's dots (Figures D, E, and H). This excludes P. malariae, where the infected erythrocytes are either not enlarged or even slightly decreased in size.
Plasmiodium vivax was excluded because in P. vivax the infected erythrocytes would be more markedly enlarged (up to 2×) and/or deformed, and the schizonts would have had more (12 to 24) and smaller merozoites.
While it is not a good idea to use travel history to make malaria species determination, both diagnoses of P. ovale and P. falciparum are compatible with the fact that the child came from the Democratic Republic of Congo by way of South Africa. One way to confirm the diagnosis would have been to perform PCR. However, this option was not available: the smears were coverslipped and the hospital had no pretreatment anticoagulated blood left.
The patient should be treated for chloroquine-resistant P. falciparum (since there remains a question of P. falciparum, acquired in an area where chloroquine resistance occurs), and should also include primaquine to prevent relapses from dormant liver stages of P. ovale.
More on: Malaria
Images presented in the monthly case studies are from specimens submitted for diagnosis or archiving. On rare occasions, clinical histories given may be partly fictitious.
 ShareCompartir
ShareCompartir


