

|

|

Volume 4: No.
4, October 2007
ORIGINAL RESEARCH
Adapting Evidence-Based Strategies to Increase Physical Activity Among African Americans, Hispanics, Hmong, and Native Hawaiians: A Social Marketing Approach
Mary Ann S. Van Duyn, PhD, MPH, RD, Tarsha McCrae, MPH, CHES, Barbara K. Wingrove, MPH, Kimberly M. Henderson, MA, Jamie K. Boyd, PhD, RN, FNP, Marjorie Kagawa-Singer, PhD, Amelie G. Ramirez, PhD, Isabel Scarinci-Searles, PhD, Lisa S. Wolff, MA, Tricia L. Penalosa, MPH, Edward W. Maibach, PhD
Suggested citation for this article: Van Duyn MAS, McCrae T, Wingrove BK, Henderson KM, Boyd JK,
Kagawa-Singer M, et al. Adapting evidence-based strategies to increase physical activity
among African Americans, Hispanics, Hmong, and Native Hawaiians: a social marketing approach. Prev Chronic Dis
2007;4(4).
http://www.cdc.gov/pcd/issues/2007/
oct/07_0025.htm.
Accessed [date].
PEER REVIEWED
Abstract
Introduction
Using a social marketing approach, we studied how best to adapt proven, evidence-based strategies to increase physical activity for use with
underserved racial or ethnic groups.
Methods
We conducted focus groups with low-income Hispanic women in Texas, Hmong parents and their children in California, low-income African American women and men in the Mississippi Delta, and Native Hawaiian college students in Hawaii. We also interviewed key leaders of these communities. Topics of discussion were participants’ perceptions about 1) the benefits
of engaging in
physical activity, 2) the proposed evidence-based strategies for increasing each community’s level of physical activity, and 3) the benefits and barriers to following the proposed interventions for increasing physical activity. A total of 292 individuals participated in the study.
Results
All groups considered that being physically active was part of their culture, and participants found culturally relevant suggestions for physical activities appealing. Overwhelmingly, strategies that aimed to create or improve social support and increase access to physical activity venues received the most positive feedback from all groups. Barriers to physical activity were
not culturally specific; they are common to all underserved people (lack of time, transportation, access, neighborhood safety, or economic resources).
Conclusion
Results indicate that evidence-based strategies to increase physical activity
need to be adapted for cultural relevance for each racial or ethnic group. Our research shows that members of four underserved populations are likely to respond to strategies that increase social support for physical activity and improve access to venues where they can be physically active.
Further research is needed to test how to implement such strategies in ways that are embraced by community members.
Back to top
Introduction
The rising rate of obesity and the diminishing level of physical activity contribute to the increasing health problems among a growing proportion of the U.S. population (1). Research indicates that being overweight, physically inactive, or eating unhealthfully increases risk for certain cancers, particularly breast and colon cancers (2–7). In particular, people from minority racial or
ethnic groups and other underserved populations suffer disproportionately from overweight and obesity: 70% of African American adults and
73% of Hispanic adults are overweight (8). In addition to experiencing higher rates of overweight and obesity than white Americans, African Americans, Hispanics, and other minority racial or ethnic groups are less likely to engage in healthful levels
of physical activity (PA) (9) and more likely to experience a high incidence of some cancers and high related mortality rates (10). The high levels of insufficient activity and the persistent disparity in cancer rates underscore the need for better promotion of culturally appropriate strategies to increase levels of physical activity in order to prevent cancer.
The number of community programs to increase physical activity among U.S. residents is growing. Several recent intervention studies show how to plan and implement community interventions that promote physical activity among racially and ethnically diverse populations. The
interventions tend to emphasize involving the target community early (i.e., during the planning stage), tailoring the physical activity
programs to suit the predominant race or ethnicity of the community, and creating partnerships among diverse groups. These interventions also focus on the social determinants of health (e.g., levels of income, racial segregation, social support) and on needed structural and policy changes (11-15). However, these interventions do not always use evidence-based strategies for increasing PA.
The number of proven, evidence-based strategies to increase PA is small but expanding rapidly. Some strategies that work address the needs of individuals and the community as a whole. However, research findings do not show clearly how best to adapt and promote these strategies for use in various racial or ethnic communities. To promote evidence-based strategies for increasing PA effectively
and to improve their use with people from various cultures, we need to understand what these various cultures see as the benefits of and barriers to engaging in PA. With such information, public health organizations and practitioners can create guidelines for implementing PA programs in ways that emphasize the benefits (as seen by the target community) and recommend ways of reducing or altogether
avoiding the barriers of greatest concern to these communities. Tailoring evidence-based strategies to increase PA in this way could also aid in their dissemination.
To learn how best to adapt and disseminate evidence-based strategies to
increase PA, the National Cancer Institute's (NCI's) Center to Reduce Cancer
Health Disparities and NCI's Center for Strategic Dissemination funded four
research projects in 2004 through
its established Special Populations Networks (SPN) (16-19). The goal of these projects was to improve the dissemination of proven approaches to increasing PA among communities with high rates of health problems. Racially, ethnically, and geographically diverse SPN research teams conducted focus groups with members of three low-income communities: Redes en Accíon worked with Hispanic women in
Texas; the Asian American Network for Cancer Awareness, Research, and Training worked with Hmong parents and their children in California; and Deep South Network for Cancer Control worked with African American women and men in the Mississippi Delta. A fourth community consisted of Native Hawaiian college students who were not necessarily low income; the SPN project
`Imi Hale conducted the focus
groups and interviews with this group. In addition focus groups and interviews were conducted with gatekeepers (also known as key informants). These are the leaders and others who serve these communities and who can influence how community members behave.
This article discusses the background and framework for this four-site study and gives an overview of lessons learned and the common themes that emerged from all four communities. Detailed findings from each study site are available elsewhere (20-23). Here we highlight the similarities and differences among these study populations and discuss findings distilled from the research that may
prove useful in adapting proven, evidence-based strategies to increase PA in order to control or prevent cancer.
Back to top
Methods
Framework
A social marketing framework was the theoretical basis for the study. Social marketing aims to influence the voluntary behavior of target audience members by offering a package of benefits for engaging in the desired behavior, reducing barriers to engaging in the behavior, and focusing on the target population’s needs and wants with regard to the behavior (24-26). Social marketing
further posits the importance of fulfilling the interests of those whose health would benefit from a change in behavior and those who are promoting the desired behavior (27).
The figure shows two paths that researchers must take to learn how best to disseminate an intervention. On one path the researchers learn by segmenting the intervention’s target population and studying what will appeal to each population segment. On the other path, researchers work with gatekeepers (i.e., community leaders and others who influence the target population) to learn about
each population’s culture and beliefs. Gatekeepers can be intermediaries between researchers and the target population and can help to implement strategies to improve the general health of their communities. The results of both sets of research must be taken into account if we are to design and disseminate successful energy balance programs (i.e., programs that help people maintain a
healthy balance between calories consumed and calories expended). In our study, we followed both paths in order to learn how individuals and gatekeepers in each of the study’s four populations perceive the benefits of, and barriers to, PA. We also wanted to get their reactions to selected evidence-based interventions to increase PA so that we could learn how 1) to adapt those
interventions in ways that appealed to each group and 2) to disseminate them successfully to each population.
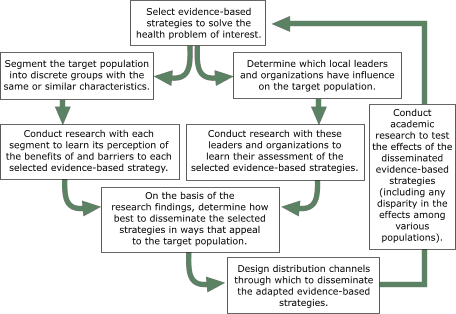
Figure. A
framework for adapting evidence-based public health strategies to appeal to
specific populations. [A text description of this chart is also available.]
Design
SPN grantees at each of the four study sites agreed to interview or conduct focus groups with community members and gatekeepers in order to assess each community’s perceptions of the benefits of, and barriers to, five recommended strategies for increasing PA. With the community members, they conducted only focus groups. With gatekeepers, they interviewed some individually and conducted
focus groups with others. Since each study site had a unique racial or ethnic community, researchers opened with a culturally appropriate introduction and then asked similar questions of focus group participants and interviewees. The results were categorized by the theoretical constructs that support the recommended approaches.
Participants at each site were informed about the purpose of the project, and each participant signed an informed consent agreement. The consent agreements, which were written in participants’ native languages, were reviewed and approved by the Institutional Review Boards
of the institutions associated with each project site (Table 1). Group discussions were held at a local community setting: a church (Latina women),
a community center (African American women and Hmong parents and children), and a college campus (Native Hawaiian college students). Each session was moderated by a trained interviewer, audiotaped, translated when necessary, and transcribed. In addition, a recorder took notes
to ensure that the transcriptions were accurate.
Participants
Table 1 shows the characteristics of the community members (n = 244: 45 men, 159 women, and 40 children aged 11 to 14 years) and gatekeepers (n = 48) who participated in focus groups or interviews in each study community. Gatekeepers for Latinas were church leaders in Texas; for the Hmong, a family social worker, a church leader, a teacher, and a leader from a community organization in
California; for African Americans, Community Health Advisors trained as Research Partners (CHARPS) in Mississippi; and for Native Hawaiians, community elders in Hawaii.
Measures
To help us decide on five core strategies for all four communities, we used the
review of the effectiveness of interventions to increase PA in the Centers for Disease Control and Prevention’s (CDC’s) Guide to Community Preventive Services (28,29).
Table 2 describes each of the five evidence-based strategies under study: 1) mount communication campaigns to increase PA
throughout the community, 2) change individual behavior related to PA, 3) improve social support for PA, 4) increase access to places for PA, and 5) place point-of-decision prompts at strategic locations. Together the five strategies form a wide-ranging, multilevel approach to addressing the behavioral, psychological, and environmental factors related to increasing PA.
Back to top
Results
Table 3 summarizes findings from the focus groups and interviews conducted at each site. An analysis of those findings follows:
Relationship Between Health and PA
Most participants and gatekeepers at all four sites said that they value PA
and that being active is an inherent part of their culture. Culture influenced
how participants perceived the relationship between health and PA (e.g. most saw
physical activity as something grounded in their culture through activities such
as growing food or running on the beach) rather than through more mainstream
activities such as attending aerobics classes or swimming laps.
Participants and gatekeepers viewed being active as a “natural” way of life. In earlier generations, being “naturally” active was achieved simply through one’s daily routine (e.g., farming, doing manual labor, walking to the store). With the current reliance on cars, concerns about neighborhood safety, and jobs requiring little physical labor, even in these
communities few people sustain a sufficient level of PA through the activities of their day-to-day life. Having to purposefully think about being active seemed to be a strange concept for some, particularly for those in the Native Hawaiian and Hmong groups.
Strategy 1: Mount Community Campaigns to Increase PA
Focus Group Participants (Individual Community Members)
Community members at all four sites supported culturally based community events and suggested activities and venues that incorporated aspects of their cultural heritage. Native Hawaiians, for example, reported preferring activities such as dancing hula, farming, canoeing, and running on the beach. Hmong families mentioned the benefits of outreach activities at Asian grocery stores, community
organizations, churches, and festivals; and Latina women expressed a desire for programs sponsored by the church or other familiar—and safe—locations. All four groups felt a strong sense of community pride.
Community members recognized the value of the media (e.g., radio, television) in community campaigns but wanted media messages to include culturally appropriate information and advice. Hmong and Latina participants said that having media messages in their native language was important and that they should be broadcast through channels that used those languages. Community members also said that
word-of-mouth in small communities is a powerful dissemination method. They preferred health messages delivered by peers or role models and related stories that involved local people.
Several concerns were raised related to community-wide campaign strategies. For example, focus group members believed health messages get lost within the cluttered media environment and that some community members have difficulty reading campaign print materials. Others noted few opportunities for interaction or group activities at community events as well as lack of transportation, time, and
child care. Another problem is motivation to attend activities if they are perceived as one-time events and not part of an ongoing program.
Gatekeepers
Gatekeepers at all the sites had a positive view of a community campaign to increase PA. For them, the primary appeal of this strategy was that it provides information to the entire community and does not single out people who are at different fitness levels. In addition, gatekeepers said that using native languages, tailoring messages specifically for their community, using trusted role
models (e.g., doctors, teachers, cultural leaders), and disseminating messages through community organizations could help ensure meaningful interpersonal experiences for the target population.
The major barrier reported by the gatekeepers to a community campaign, even one that is culturally appropriate, is that it does not allow for further segmentation of the audience. Cultural groups are not homogeneous, and individuals vary
in literacy levels, health status, psychological issues (e.g., self-esteem, shame, depression), financial status, and strength of cultural and family
values.
Strategy 2: Change Individual Behavior Related to PA
Focus Group Participants (Individual Community Members)
Most community participants reported enjoying cultural activities such as tai
chi, walking, stretching, farming, and hunting. However, the specific evidence-based activities that fall under this strategy (e.g., keeping track of one’s steps with a free pedometer) were not well received by most participants. Participants cited a cultural preference for group activities over individual
activities. Some participants believed that individual approaches are not effective or sustainable and that activity should not be planned but part of an active life.
Focus group participants at three sites reported that an approach that focuses on the individual might be effective only for those who are already motivated. The exception was African Americans in Mississippi, who said that working with a personal trainer (of the same sex), being given personal diet and exercise plans, and learning about fitness through hands-on activities were appealing
options, particularly if available at no cost.
Gatekeepers
Gatekeepers at the four sites viewed the individual behavior-change approach somewhat more positively than the community members did. They said that, since this strategy is an individual approach to increasing PA, it could address some personal issues (e.g., low self-esteem, personal health problems) and interpersonal issues (e.g., family and cultural pressures). Yet, they noted that numerous
logistical barriers would make implementing this strategy challenging. They also noted that providing personal trainers community-wide would be difficult and costly.
Strategy 3: Improve Social Support for PA
Focus Group Participants (Individual Community Members)
Improving social support for PA received the strongest positive feedback at all sites because it was considered in line with cultural norms. Participants reacted positively to the idea of group activities that were culturally relevant, hands on, purposeful (e.g. walking children to school, the market, or church), and inclusive (doable by people at many fitness levels). It was considered
essential to involve and engage the support of family and friends in group activities. For Hmong families and Native Hawaiian young adults, group activities were particularly important. Latina women preferred that incentives, such as prizes or friendly competition, be incorporated into group activities. African American adults said they would be motivated by support through church activities such
as messages from the pulpit, group walks with other church members, and competitions between churches.
Participants reported few barriers associated with improving social support for PA, and the barriers they did suggest related to lifestyle issues. Participants acknowledged that lack of time and, to some extent, lack of transportation were barriers. For Latinas and African Americans, lack of child care was a barrier to engaging in this strategy.
Gatekeepers
At all sites, gatekeepers supported improving social support for PA because extended families, church, and community—major pillars in the culture of these four communities—would be involved. However, we did learn of some barriers that were specific to one site. For Native Hawaiians, community leaders reported as barriers western influences (e.g., commercialization of
‘aina [land] once used for farming and hunting) and assimilation (e.g., support systems burdened with demands of the modern mainstream culture). Health practitioners in the Latino community said that barriers were lifestyle issues such as difficulties with transportation and lack of time. The Hmong gatekeepers said that they had little ability to influence their environments (e.g.
workplace, schools), and African American gatekeepers said that the powerful social forces in their community — the family, church, and community organizations — were usually conservative and therefore often resistant to change. Changing the views and behavior of these influential forces in the various communities is a key requisite to being successful in having community members
adopt more active lifestyles than they now lead.
Strategy 4: Improve Access to Places for PA
Focus Group Participants (Individual Community Members)
For all four ethnic groups, creating or improving access to PA was an appealing strategy and garnered the second most positive feedback, almost as positive a reaction as that for improving social support for PA. Participants reported valuing their community resources and wanting to use their parks, walking trails, community recreation centers, churches (African Americans and Latina women), beaches (Native Hawaiian college students), and playgrounds (Hmong families). In general, all placed a high priority on places for PA in their communities, particularly if facilities are free of charge, have flexible hours, are available for groups and families, and offer outdoor activities during good weather.
All participants said they faced overwhelming barriers to accessing available PA resources. Latina, African American, and Hmong participants cited safety concerns as significant barriers to accessing resources because many live in communities with high crime rates and poor infrastructure (particularly lack of sidewalks and bad lighting). In addition, some participants said that their
communities did not possess adequate public areas for activity. They reported a lack of walking trails and bicycle paths and poor or intimidating equipment. Latina women also cited cultural issues related to modesty and machismo. At each site, many participants reported lack of time, lack of transportation, and the high cost of admission to some venues as barriers to this strategy.
Gatekeepers
Gatekeepers stressed that, although creating access to new places for PA is important, equally important is improving access to existing community facilities. Gatekeepers also cited the same safety and lifestyle issues reported as obstacles by the community members. In addition, Native Hawaiian gatekeepers noted that access to farming lands has diminished drastically in recent years.
Strategy 5: Place Point-of-Decision Prompts to Encourage PA at Strategic Locations
This strategy was not discussed in detail at any sites by either community members or gatekeepers. Participants found it challenging to relate to this strategy because the main location where prompts would be placed is next to elevators or escalators, and these four communities have few elevators or escalators. When the strategy was expanded to include other everyday opportunities to walk
instead of ride (e.g., parking farther from shops or walking instead of driving to work), participants reported time and safety constraints as barriers. Overall, participants did not see this strategy as useful for promoting behavior change.
Back to top
Discussion
Evidence-based strategies to promote PA frequently lack cultural relevance. The purpose of our study was to use a social marketing approach to find ways in which these strategies could be adapted to suit various cultures. Our findings confirm and refine what practitioners know to be true: that one size does not fit all and that tailoring proven approaches to suit each racial, ethnic, or
geographic community is important to fostering behavior change. Our study also suggests that a social marketing approach to eliciting perceptions about the benefits of and barriers to participating in physical activities is viable and useful for adapting evidence-based strategies in ways that are embraced by members of specific communities. Multilevel, culturally adapted, social intervention
approaches to adopting healthy lifestyles, including increasing PA, are important both for mainstream (30-32) and for underserved populations who deal with numerous barriers to active lifestyles (33-41).
Our research indicates that the strategies that appeal most to these four populations are those aimed at improving social support and increasing access to places for PA. Desirable components of physical activity programs are those that involve group activities (all sites) or partners (Latina women and African Americans), incorporate cultural components (Native Hawaiians and Hmong), are
family-centric or encourage family and community support (all). Community members and gatekeepers also placed high value on increasing access to places for PA in their communities, particularly if these facilities are easy to get to, accommodate family and work schedules, and are available at low or no
cost.
Participants in our study believed that it was important to be active and wanted their activities to be culturally relevant. Messages to encourage increased PA and associated activities need to be 1) tailored to the unique cultural and sociodemographic characteristics of each community and 2) sensitive to individual factors such as time and financial constraints. Ideally, activities should be
group-focused, hands-on, purposeful, and inclusive. They should engage not only families and friends, but also extended families, church, and community — major social forces within the culture of these four communities. Messages to these groups should also stress that setting aside time to be active is important. Many participants assumed that the recommended amount of activity could be
done through one’s daily activities. It is also critical that messages emphasize 1) that the recommended levels of PA can be achieved through culturally relevant activities and 2) that everyone needs to purposefully set aside time for these activities.
On the basis of our findings, interventions would benefit from efforts to decrease physical or environmental barriers to places where people can be physically active. Interventions need to incorporate existing community facilities into their strategies, but these facilities may need to be modified so that they are easy to reach, safe, and available for various kinds of PA. Partnerships with
community leaders to overcome social and physical barriers to PA (e.g., concerns about crime, lack of infrastructure, inadequate transportation, lack of access to places where people can be physically active) should be an integral part of any intervention (14). Community leaders, for example, can help recruit community and, possibly, state partners in health- and nonhealth-related divisions
of local government (e.g., transportation, education, commerce) that can increase opportunities for PA within the community. Mobilizing relevant individuals and organizations (such as
CHARPS in Mississippi and the Native Hawaiian elders recruited for our study) to advocate for outlets for PA is critical to sustaining increases in PA.
Interestingly, many participants’ reported barriers to PA were not culturally specific; they are common among underserved populations of diverse heritage (38-40,42). Lack of time, lack of transportation, lack of economic resources to pay for programs and membership fees, literacy problems, unsafe neighborhoods, and lack of access to places to engage in PA were common to the Hmong,
Latina, African American, and Native Hawaiian groups. These groups were also mainly low income, and with the exception of the Native Hawaiians, not well educated. Having a low income and a low level of education (regardless of race, ethnicity, or culture) poses major challenges to improving fitness (43). Policy changes at the community level are critical, since interventions that target the
cultural, physical, social, and economic environment of a community will be more effective than interventions that target individuals in reducing the barriers to physical activity that many low-income populations face.
The use of social marketing methods in this study is consistent with the community-based participatory research (CBPR) approach. This approach involves communities in all phases of research that affects them and recognizes the community as an equal research partner (44). This collaborative process — involving both community members and leaders — is integral to CBPR and will help
produce useful results for the participating communities and their partners.
During this study we learned the perceived benefits of, and barriers to, strategies to increase PA among groups whose perspectives were not previously explored. Results are not, however, statistically representative of a larger population because of nonrandom recruiting techniques, small sample sizes, and use of qualitative rather than quantitative research methods (45).
Another weakness of this study is the limited discussion about point-of-place
prompts (i.e., signs to encourage activities such as taking the stairs rather
than the elevator). Other studies show that point-of-place prompts are effective in a Latino community (46) but not in a suburban African American community (47). Given these limited and mixed findings, future qualitative research on this strategy is warranted.
Our study focused on the perceived benefits and barriers associated with proven PA strategies, which may have precluded our generating ideas for other strategies for increasing PA. However, the strategies we did discuss are evidence-based and have a high chance of succeeding. In future qualitative research, participants might first brainstorm to come up with strategies and then discuss
in-depth any suggested strategies for which there is evidence to indicate they were successful in other communities.
Back to top
Acknowledgments
This study was sponsored by National Cancer Institute’s (NCI’s) Special Populations Network (SPN) and funded by NCI’s Center to Reduce Cancer Health Disparities and NCI’s Center for Strategic Dissemination. The following institutions and investigators also contributed to this study: Redes in Accíon, National Latino Cancer Research Network: A. Ramirez (principal
investigator), K. Gallion (pilot project leader), P. Chalela (investigators) U01-CA86117;
`Imi Hale, Native Hawaiian Cancer Network: C. Chong (principal investigator), J. Boyd (pilot project leader), K. Braun (investigator), J. Tsark (investigator) U01-CA86105; Asian American Network for Cancer Awareness, Research and Training: M.S. Chen, Jr. (principal investigator), M. Kagawa-Singer (pilot
project leader), G. Harrison (investigator) U01-CA86322; The Deep South Network for Cancer Control: E. Partridge (principal investigator), G. Parham (pilot project leader), I. Scarinci-Searles (investigator) U01-CA86128; NCI, Center to Reduce Cancer Health Disparities: H. Freeman (Director), B. Wingrove (pilot project leader), T. McCrae (investigator), R. Washington (investigator), K. Henderson
(investigator), T. Penalosa (investigator); NCI’s Center for Strategic Dissemination: E. Maibach (director), M. Van Duyn (pilot project leader), B. Bloodgood (investigator), E. Macario (consultant), L. Wolff (consultant).
Back to top
Author Information
Corresponding Author: Mary Ann S. Van Duyn, National Cancer Institute, Center to Reduce Cancer Health Disparities, 6116 Executive Blvd., Suite 602, Rockville, MD 20852. Telephone: 301-451-4284; Email:
vanduynm@mail.nih.gov
Author Affiliations: Tarsha McCrae, Barbara K. Wingrove, Kimberly M. Henderson, Tricia L. Penalosa, National Cancer Institute, Rockville, Maryland; Jamie K. Boyd, Papa Ola Lokahi, Honolulu: Marjorie Kagawa-Singer, University of California, Los Angeles; Amelie G. Ramirez, Baylor College of Medicine, San Antonio; Isabel Scarinci-Searles, University of Alabama, Birmingham; Lisa S. Wolff,
Harvard School of Public Health, Boston; Edward W. Maibach, George Washington University, Washington, DC.
Back to top
References
- Preventing obesity and
chronic diseases through good nutrition and physical activity. Atlanta (GA): Centers for Disease Control and Prevention; 2005.
http://www.cdc.gov/nccdphp/publications/ factsheets/Prevention/obesity.htm.
Accessed January 8, 2007.
- Dallal CM, Sullivan-Halley J, Ross RK, Wang Y, Deapen D, Horn-Ross PL, et al.
Long-term recreational physical activity and risk of invasive and in situ breast cancer:
the California teachers study. Arch Internal Med 2007;167(4):408-15.
- Weight control and physical activity. Lyon (FR): International Agency for
Research on Cancer; 2002.
- McTiernan A.
Obesity and cancer: the risks, science, and potential management strategies. Oncology
(Williston Park) 2005;19(7):871-82,885-6.
- Vainio H, Kaaks R, Bianchini F.
Weight control and physical activity in cancer prevention: international evaluation of the evidence. Eur J Cancer Prev 2002;11 Suppl 2:S94-100.
- Bianchini F, Kaaks R, Vainio H.
Overweight, obesity, and cancer risk. Lancet Oncol 2002;3(9):565-74.
- Obesity and cancer: questions and answers. Bethesda (MD): National Cancer Institute;2004.
http://cancer.gov/cancertopics/factsheet/risk/obesity. Accessed January 8,
2007.
- Obesity in minority populations. Washington (DC): American Obesity
Association;2005. http://www.obesity.org/subs/fastfacts/Obesity_Minority_Pop.shtml.*
Accessed January 8, 2007.
- Behavioral Risk Factor Surveillance System. Atlanta (GA): Centers for
Disease Control and Prevention;2007. http://www.cdc.gov/brfss/. Accessed June
11, 2007.
- Cancer facts and figures 2007. Atlanta (GA): American Cancer Society; 2007.
http://www.cancer.org/downloads/STT/CAFF2007PWSecured.pdf.* Accessed May 1,
2007.
- Kumanyika SK.
Minisymposium on obesity: overview and some strategic considerations. Annu Rev Public Health 2001;22:293-308.
- Tanjasiri SP. Shared responsibility: California’s state and community partnerships to promote physical activity among diverse populations. J Health Educ 1999;30(2):S64-71.
- Yancey AK, Kumanyika SK, Ponce NA, McCarthy WJ, Fielding JE, Leslie JP, et
al. Population-based interventions engaging communities of color in healthy eating and active living: a review. Prev Chronic Dis
2004;1(1).
http://www.cdc.gov/pcd/issues/2004/jan/03_0012.htm.
- Schulz AJ, Zenk S, Odoms-Young A, Hollis-Neely T, Nwankwo R, Lockett M, et
al. Healthy eating and exercising to reduce diabetes: exploring the potential of social determinants of health frameworks within the context of community-based participatory diabetes prevention. Am J Public Health 2005;95(4):645-51.
- Banks-Wallace J, Conn V.
Interventions to promote physical activity among African American women.
Public Health Nurs 2002;19(5):321-35.
- Lisovicz N, Johnson RE, Higginbotham J, Downey JA, Hardy CM, Fouad MN, et al.
The Deep South Network for cancer control. Building a community infrastructure
to reduce cancer health disparities. Cancer 2006;107(8 Suppl):1971-9.
- Chen MS, Shinagawa SM, Bal DG, Bastani R, Chow EA, Ho RC, et al.
Asian American Network for Cancer Awareness, Research, and Training’s legacy.
The first 5 years. Cancer 2006;107(8 Suppl):2006-14.
- Ramirez AG, Talavera GA, Marti J, Penedo FJ, Medrano MA, Giachello AL, et
al.
Redes En Acción. Increasing Hispanic participation in cancer research, training, and awareness. Cancer 2006;107(8
Suppl):2023-33.
- Braun KL, Tsark JU, Santos L, Aitaoto N, Chong C.
Building Native Hawaiian capacity in cancer research and programming.
A legacy of ‘Imi Hale. Cancer 2006;107(8 Suppl):2082-90.
- Ramirez AG, Chalela P, Gallion K, Velez LF. Energy balance feasibility study for Latinas in Texas: A qualitative assessment. Prev Chronic Dis
2007;4(4). http://www.cdc.gov/pcd/issues/2007/ oct/07_0052.htm.
- Boyd JK, Braun KL. Supports and barriers to healthy living for Native
Hawaiian young adults enrolled in community colleges. Prev Chronic Dis
2007;4(4). http://www.cdc.gov/pcd/issues/2007/ oct/07_0012.htm.
- Parham GP, Scarinci-Searles I. Strategies for achieving health energy
balance among African Americans in the Mississippi Delta. Prev Chronic Dis
2007;4(4).
http://www.cdc.gov/pcd/issues/2007/oct/07_0076.htm.
- Kim LP, Harrison GG, Kagawa-Singer M. Perceptions of diet and physical
activity among California Hmong adults and youths. Prev Chronic Dis
2007;4(4). http://www.cdc.gov/pcd/issues/2007/ oct/07_0074.htm.
- Maibach EW, Van Duyn MAS, Bloodgood B. A marketing perspective on disseminating evidence-based approaches to disease prevention and health promotion. Prev Chronic Dis
2006;3(3).
http://www.cdc.gov/pcd/issues/2006/jul/05_0154.htm.
Accessed January 9, 2007.
- Kotler P, Roberto EL. Social marketing strategies for changing public behavior. New York
(NY): Free Press; 1989.
- Andreasen AR. Marketing social change: changing behavior to promote health, social development, and the environment. San Francisco
(CA): Jossey-Bass; 1995.
- Maibach EW, Rothschild ML, Novelli WD. Social marketing. In: Glanz K, Rimer BK, Lewis FM, eds. Health behavior and health education: theory, research and practice. 3rd ed. San Francisco
(CA): Jossey-Bass; 2002. p. 437-61.
- Kahn EB, Ramsey LT, Brownson RC, Heath GW, Howze EH, Powell KE, et al.
The effectiveness of interventions to increase physical activity. A systematic review. Am J Prev Med 2002;22(4 Suppl):73-107.
- Guide to community preventive services. Atlanta (GA): Centers for Disease
Control and Prevention. http://www.thecommunityguide.org.* Accessed September 1,
2006.
- Bauman A. Commentary on the VERB campaign- perspectives on social marketing to encourage physical activity among youth. Prev Chronic Dis 2004;1(3).
http://www.cdc.gov/pcd/issues/2004/jul/04_0054.htm.
Accessed January 8, 2007.
- Finlay SJ, Faulkner G.
Physical activity promotion through the mass media: inception, production, transmission and consumption. Prev Med 2005;40(2):121-30.
- Napolitano MA, Marcus BH.
Targeting and tailoring physical activity information using print and information technologies.
Exerc Sport Sci Rev 2002;30(3):122-8.
- Bird J, Otero-Sabogal R, Ha N, McPhee S. Tailoring lay health worker interventions for diverse cultures: lessons learned from Vietnamese and Latina communities. Health Educ Q 1996;23:S105-22.
- Evenson KR, Sarmiento OL, Macon ML, Tawney KW, Ammerman AS.
Environmental, policy and cultural factors related to physical activity among Latina immigrants. Women Health 2002;36(2):43-57.
- Eyler AA, Brownson RC, Donatelle RJ, King AC, Brown D, Sallis JF.
Physical activity social support and middle- and older-aged minority women: results from a US survey. Soc Sci Med 1999;49(6):781-9.
- Eyler AA, Baker E, Cromer L, King AC, Brownson RC, Donatelle RJ.
Physical activity and minority women: a qualitative study. Health Educ Behav 1998;25(5):640-52.
- Henderson KA, Ainsworth BE.
A synthesis of perceptions about physical activity among older African American and American Indian women. Am J Public Health 2003;93(2):313-7.
- Palmer TA, Jaworski CA.
Exercise prescription for underprivileged minorities. Curr Sports Med Rep 2004;3(6):344-8.
- Sanderson B, Littleton M, Pulley L.
Environmental, policy, and cultural factors related to physical activity among rural, African American women. Women Health 2002;36(2):75-90.
- Thompson JL, Allen P, Cunningham-Sabo L, Yazzie DA, Curtis M, Davis SM.
Environmental, policy, and cultural factors related to physical activity in sedentary American Indian women. Women Health 2002;36(2):59-74.
- Whitehorse L, Manzano R, Baezconde-Garbanati L, Hahn G. Culturally tailoring a physical activity program for Hispanic women: recruitment successes of La Vida Buena’s salsa aerobics. J Health Educ 1999;30(2):S18-24.
- Wilber J, Chandler P, Dancy B, Choi J, Plonczynski D.
Environmental, policy, and cultural factors related to physical activity in urban, African American women. Women Health 2002;36(2):17-28.
- Muennig P, Lubetkin E, Jia H, Franks P.
Gender and the burden of disease attributable to obesity. Am J Public Health 2006;96(9):1662-8.
- Introduction to methods in community-based participatory research for health. In: Israel BA, Eng E, Schulz AJ, Parker EA, eds. Methods in community-based participatory research for health. San Francisco
(CA): Wiley; 2005. p. 3-26.
- Stewart DW, Shamdasani PN. Focus groups: theory and practice. Newbury Park (CA): Sage; 1990.
- Coleman KJ, Gonzalez EC.
Promoting stair use in a US–Mexico border community. Am J Public Health 2001;91(12):2007-9.
- Andersen RE, Franckowiak SC, Snyder J, Bartlett SJ, Fontaine KR.
Can inexpensive signs encourage the use of stairs? Results from a community
intervention. Ann Intern Med 1998;129(5):363-9.
Back to top
|
|
