

|

|

Volume 4: No. 3, July 2007
COMMUNITY CASE STUDY
Effective Tobacco Control in Washington State: A Smart Investment for Healthy Futures
Julia A. Dilley, MES, Kristen Rohde, MA, Clyde Dent, PhD, Michael J. Boysun, MPH, Michael J. Stark, PhD, Terry Reid, MSW
Suggested citation for this article: Dilley JA, Rohde K, Dent C, Boysun MJ, Stark MJ, Reid T. Effective tobacco control in Washington State: a smart investment for healthy futures. Prev Chronic Dis [serial online] 2007 Jul [date cited]. Available from:
http://www.cdc.gov/pcd/issues/2007/
jul/06_0109.htm.
PEER REVIEWED
Abstract
Background
Tobacco use remains the leading cause of preventable death in the United States. Following the 1998 Master Settlement Agreement with the tobacco industry, Washington State dedicated substantial funding to the creation of a statewide, comprehensive tobacco control program. This report documents the history and observed effectiveness of that program.
Context
In 2000, the Washington legislature allocated $100 million out of the first Master Settlement payment of $320 million to tobacco control. The comprehensive tobacco control program was launched late that same year with an annual budget of $15 million.
Methods
We used existing data from state and national health behavior surveillance
systems to describe smoking prevalence among adults and youth. For adult
measures, we used data from the Washington State Behavioral Risk Factor
Surveillance System and the National Health Interview Survey. For youth
measures, we used data from the Washington State Healthy Youth Survey and the
national Monitoring the Future survey. We used the National Cancer Institute’s “Joinpoint” software to compare trends.
Consequences
Between 1990 and 2001, adult smoking prevalence in Washington was nearly unchanged, as it was in the United States as a whole. However, from 2001, one year after Washington instituted its comprehensive tobacco control program, to 2005, the prevalence of smoking among adults in Washington declined significantly from 22.5% to 17.6%, and by a significantly larger amount than it did nationally
during the same period (22.7% to 20.9%). In addition, the prevalence of youth smoking also declined faster in Washington
than it did nationally; for example, from 2000 to 2004, smoking prevalence among
8th graders declined from 12.5% in 2000 to 7.8% in 2004 in Washington but only from 12.2% in to 9.3% nationally.
Interpretation
Significant reductions in smoking prevalence among Washington residents following the implementation of a comprehensive tobacco control program funded at a level near that recommended by
the Centers for Disease Control and Prevention indicate that tobacco control programs are an effective investment for states committed to improving public health.
Back to top
Background
Tobacco use and exposure to secondhand smoke are widely considered to be leading causes of preventable disease and death in the United States (1). To help reduce the prevalence of tobacco use and
exposure to secondhand smoke, the Centers for Disease Control and Prevention (CDC) described a “best practices” framework, including recommended funding levels, for comprehensive state
tobacco control programs (2). This framework was modeled on successful programs to reduce smoking that were implemented in California and Massachusetts, as well as on research
findings. Individual components of the framework are designed to work synergistically with changes in government policies
aimed at reducing tobacco use, such as increasing taxes on tobacco products and
prohibiting smoking in specified public areas.
Following the 1998 Master Settlement Agreement between states’ attorneys general and the tobacco industry, Washington State dedicated substantial funding to tobacco control and used the CDC framework to design a comprehensive state program. Five years after the program was implemented in 2002, policymakers are considering what level of funding to allocate for ongoing support of the
program.
Recent research has demonstrated that there is a dose-response relationship between investment in tobacco control and the extent to which tobacco usage rates decline. For example, the results of a study that correlated state trends in cigarette consumption with state per capita expenditures on major tobacco control programs showed that increased investment in tobacco control was
associated with reductions in smoking and concluded that “larger, more established programs may have a larger dollar for dollar impact” (3). Similarly, an analysis of national youth data using a variety of statistical models also found that per capita tobacco control expenditures were inversely associated with smoking prevalence and daily cigarette consumption among youths and
estimated that the prevalence of youth smoking would be 3% to 14% lower today if all states had spent the minimum amount recommended by CDC (4).
In this report, we describe the investment in and implementation history of tobacco control programs in Washington State, assess the effectiveness of those programs over time, and identify critical populations remaining in need of support.
Back to top
Context
Table 1 summarizes the history of tobacco control programs, cigarette taxation, and major
tobacco-related legislation in Washington; Figure 1 shows the total per capita funding for statewide tobacco control programs from 1990 through 2005.
In 1990,
before implementation of any substantial tobacco
control activities in Washington, 22.5% of Washington adults smoked.
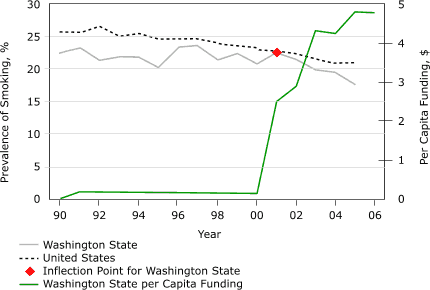
Figure 1. Smoking prevalence rates among adults in
Washington State and the United States and tobacco control funding per
capita in Washington State, 1990 through 2005. Data for Washington State are
from the Washington State Behavioral Risk Factor Surveillance System; data
for the United States are from the National Health Interview Survey. The point of inflection is the
point at which the slope of a line changes significantly. [A tabular version of this graph is also available.]
In 1991, Washington was one of 17 states to receive funding from Project ASSIST
(American Stop Smoking Intervention Study), a state-based tobacco control study implemented by the National Cancer Institute (5). The goal of ASSIST was to change the social, cultural, economic, and environmental factors that influence
smoking behavior by policy changes in three areas: increasing tobacco taxes, limiting youth access to
tobacco, and promoting smoke-free environments. ASSIST funds were used to establish a statewide coalition called Tobacco Free Washington and to implement tobacco control activities in several large counties. In 1993, Washington passed a state law that required retailers to be licensed to sell tobacco products, and a portion of the license fee was dedicated to tobacco control in the
communities where the retailers were located. From 1991 through 1999, Washington also passed laws to restrict smoking in workplaces and modestly increased taxes on tobacco products.
In 1998, the Master Settlement Agreement was negotiated between the tobacco industry and states’ attorneys general, led by then Washington Attorney General Christine Gregoire. Washington
State received its first $320 million settlement payment in 2000, and the state legislature allocated $100 million of that payment to support a comprehensive state tobacco control program. The state then
established the Washington Tobacco Prevention and Control Council to develop a comprehensive tobacco control plan for how allocated funds were to be used (6). The plan was grounded in the CDC framework and developed on the basis of advice from hundreds of stakeholders in topical working groups. Washington
State began to implement the plan in the fall of 2000.
Table 2 summarizes the CDC framework for tobacco control, including the CDC-recommended percentage of tobacco control funds to be spent on individual program components and the percentage of Washington
State’s current funding spent in each component area. Currently, the overall program is funded at $26.3 million per year, which is approximately 70% of the CDC-recommended minimum level of
$37.4 million (calculated by multiplying the 1999 minimum per capita recommendation by the 2005 Washington State population [7]).
Washington State spends approximately the CDC-recommended proportion of its tobacco control budget on school programs, statewide programs, surveillance/evaluation, and
administration (Washington State, 34%; CDC recommendation, 29%). Washington’s school programs focus on implementing CDC’s
best
practices for school-based tobacco prevention (8) in grades 5 through 9. To
reach targeted population groups statewide, leadership groups are funded to
coordinate tobacco control activities in minority communities and American
Indian tribal areas, as well as activities by businesses and the University of
Washington Public Health Training Program; funds have also been used to support
a long-established statewide multidisciplinary substance abuse/violence
prevention training/networking conference and to support surveillance and
evaluation activities, including targeted evaluation activities and the
enhancement of existing public health surveillance systems such as the
Behavioral Risk Factor Surveillance System (BRFSS) and the Healthy Youth Survey (HYS).
Washington State spends more than the CDC-recommended portion of its tobacco control budget on community-based programs (Washington
State, 22%; CDC recommendation, 14%) and counter-marketing (Washington State, 31%;
CDC recommendation, 18%). The state funds community programs in each of Washington’s 39 counties and in 27 of 29 federally recognized American Indian tribal
nations within the state; it also provides support for regional training sessions
and meetings that support other program components. The state has sponsored three paid media campaigns to discourage tobacco use (tobacco use prevention, smoking cessation/quit
line promotion, and secondhand smoke awareness); it has also engaged in tobacco-related media outreach, promoted or sponsored events to discourage tobacco use, and served as a clearinghouse
for public education and social
marketing materials.
Washington spends less than the CDC-recommended proportion of its available state tobacco control budget on disease-related programs, the enforcement of smoking prohibitions, and smoking cessation programs
(Washington State, 13%; CDC recommendation, 39%).
When the Washington Tobacco Prevention and Control Council developed the state plan for tobacco control, Washington already had an advanced cancer registry; some
tobacco control funds have been
applied to support the “planned care model” approach to changing health care systems, which includes integrating clinical best practices for tobacco use cessation to treat people with chronic disease. Funding for the enforcement of youth access laws has been shared with the state Liquor Control Board, which has authority to inspect tobacco retailers, but most of the enforcement
authority for statewide youth access and clean indoor air policies is at the local level; the higher rate of funding for community programs reflects support for this enforcement. The cessation component of the state tobacco control program includes a statewide toll-free
quit line, which provides support to all smokers who want help in quitting as well as intensive counseling and
nicotine replacement therapy to low-income and uninsured tobacco users; statewide training sessions to mobilize community programs to encourage health care systems to address tobacco use and to adopt clinical best practices for assisting patients with smoking cessation; and targeted funding to support smoking cessation within substance-abuse treatment programs.
Back to top
Methods
We used state and national surveillance data to evaluate changes in tobacco use prevalence among adults and youth from 1990 through 2005 and to determine whether the implementation of Washington
State’s comprehensive tobacco control program was associated with a significant reduction in smoking prevalence.
To describe trends in smoking prevalence among adults, we used data from the Washington State BRFSS (www.cdc.gov/brfss)
and the National Health Interview Survey (NHIS) (www.cdc.gov/nchs/nhis.htm). We then compared adult smoking prevalence trends for Washington with those for the nation from 1990 through 2005 using the National Cancer Institute’s Joinpoint
software (9), which calculates slope values (indicating the absolute change in
prevalence per year) and also identifies “points of inflection” where the slope
of a trend line changes significantly. To describe and compare prevalence trends
among youth, we used data on Washington State youth from the Washington State HYS (www3.doh.wa.gov/hys), an established youth risk behavior survey based largely
on the national Youth Risk Behavior Survey (www.cdc.gov/yrbs) (10) and the Communities that Care survey (11), and
we used data on all U.S. youth from the Monitoring the Future (MTF) survey (www.monitoringthefuture.org/
*). The HYS is administered to 6th, 8th, 10th, and 12th graders during the fall of even years. The MTF is administered to
8th, 10th, and 12th graders during the spring of every year. In both
surveys, “current smoking” is defined as having smoked any cigarettes at any time during the previous 30 days.
We compared smoking trends among Washington youth with those among U.S. youth for 2000 through 2005 only, because Washington’s youth survey methodology
was not well established before 2000.
Back to top
Consequences
Figure 1 illustrates the trends in adult smoking prevalence in Washington and
in the nation. No point of inflection was identified in the national trend. From
1990 to 2005, the national prevalence of smoking among adults declined
significantly from 25.5% to 20.9%, an average of 0.33 percentage points per year
(slope of trend line, −0.35; 95% confidence interval [CI], −0.29 to −0.41). For
Washington State, however, 2001 was a
point of inflection in the prevalence of adult smoking. From 1990 to 2001, the
prevalence of smoking in Washington State was stable (22.5% for both 1990 and
2001), but from 2001 to 2005, it declined by an average of 1.22 percentage points per year (slope
of trend line, −1.05; 95% CI, −0.45 to −1.64)
to 17.6% in 2005, which is both a significant decline and significantly greater than the decline observed nationally during the same period. Thus the smoking prevalence among Washington
State adults began to decline by significantly more than that among U.S. adults beginning just
1 year after the implementation of a well-funded comprehensive statewide program.
Figure 2 illustrates the trends in smoking prevalence among
8th graders in Washington State and nationally. The national rate declined by an average of
0.72 percentage points per year from spring 2001 to spring 2005 (slope of trend
line, −0.73; 95% CI, −0.44 to −1.02), while the prevalence in Washington
declined by an average of 1.18 percentage points per year (slope
of trend line, −1.00; 95% CI, −0.38 to −1.63). The
absolute decline of 4.7 percentage points in Washington State, from 12.5% in fall 2000 to 7.8% in fall 2004, exceeded the absolute national decline of 2.9 percentage points, from 12.2% in the spring of 2001 to 9.3% in the spring of 2005. During these periods, smoking prevalence also fell by 6.8 percentage points among
10th graders in Washington State, compared with 6.4 percentage points
among all 10th graders in the United States, and by 7.9 percentage points among 12th graders
in Washington State, compared with 6.3 percentage points among all 12th graders
in the United States. Although these differences were not statistically significant, they do suggest that the rate of decline in the prevalence of youth smoking was faster in Washington than in the nation as a whole for the period after Washington implemented its
comprehensive tobacco control program. A separate analysis of cohort growth rates in smoking prevalence among Washington students between the
6th and 12th grades from 1991 through 2005 (data not shown) also indicated that the cohort growth rate in Washington was lower than that in the nation.
Figure 2. Smoking prevalence rates among 8th-grade
youths in
Washington State and in the United States, 1990 through 2005. Data for
Washington State are from the Washington State Healthy Youth Survey; data
for the United States are from the national Monitoring the Future survey. [A tabular version of this graph is also available.]
Although Washington made some progress in instituting tobacco control policies and increasing tobacco taxes from 1990 through 2000, the prevalence of smoking did not decline significantly until after the state’s substantial investment in a comprehensive tobacco control program. The prevalence of smoking among Washington adults declined from 22.4% in 1999, just before the launch of the
program, to 17.6% in 2005. This means that there were approximately 205,000 fewer smokers in the state in 2005 than there would have been had smoking rates remained as they were before the comprehensive program was instituted. Researchers have estimated that this reduction in the number of smokers will result in future direct medical savings of $1.95 billion (12).
Despite the success of state tobacco control programs, a growing body of evidence suggests that policy makers are quick to use tobacco control money for other purposes (13) and to reduce or eliminate the funding even of successful tobacco control programs, such as those implemented in Florida and Massachusetts (14,15). Unfortunately, there is no evidence that progress in reducing tobacco use
and exposure in states with comprehensive programs is sustainable after the programs are defunded, especially since the tobacco industry continues to aggressively increase its marketing expenditures and activities (16). In fact, almost immediately following the defunding of a successful state tobacco control program in Minnesota, progress in reducing smoking among youth began to subside (17).
Similarly, the results of a recent CDC study suggest that stalled progress in reducing the national prevalence of smoking among adults may be at least partially attributable to substantial reductions in state resources dedicated to tobacco control (18).
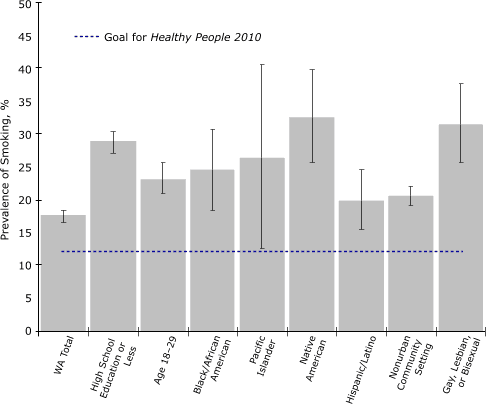
Figure 3. Smoking prevalence rates among
demographic groups in Washington State that have prevalence rates higher
than the state average. The category "Hispanic/Latino" includes
English-speaking people of any race. Error bars represent 95% confidence
intervals. Data are from the
Washington State Behavioral Risk Factor Surveillance System, 2005. [A tabular version of this graph is also available.]
Using 2005 Washington BRFSS data to identify demographic disparities in smoking prevalence among Washington adults, we found levels to be higher than average among those with a high school education or less; those aged 18 to 29; those living in nonurban zip-code areas (according to the Rural Urban Commuting Area [RUCA] classification (19); those who were gay, lesbian,
or bisexual; and those who were black, Native American, Pacific Islander, or English-speaking Hispanic (Figure 3).
Although Asians overall had a lower prevalence than the state average, studies
in Washington State found smoking prevalence among Korean and Vietnamese men to
be approximately 30% (18); thus, they represent a priority population. These populations appear less responsive to mainstream tobacco control activities and may require increasingly individualized approaches to be reached effectively (20,21). These populations are also expected to be a focus of targeted tobacco industry marketing as
the industry’s access to youth is reduced and the population at large becomes less receptive to its marketing efforts (22,23).
Substantial sustained funding will be required to reach these groups with effective counter-marketing messages. The Washington tobacco control program is implementing evaluation activities to assess the extent to which program activities
proven to be
successful in the general population can also be also be used successfully in demographic subgroups with relatively high smoking rates; for example,
the program recently examined quit line success rates and satisfaction among poor, minority, rural, and young adults (Dent CW, et al:
Unpublished study described in a poster
presented at the 2005 National Conference on Tobacco or Health, Chicago, Ill, May 2005).
Back to top
Interpretation
From 2000, when Washington established a comprehensive tobacco control program and funded it at a level approaching the minimum recommended by CDC,
through 2005, the prevalence of smoking in Washington declined significantly among both adults and youth (and significantly more than in the nation as a whole).
Our findings indicate that a comprehensive tobacco control program is an effective and cost-effective investment in public health and that a substantial sustained investment will produce better results than minimal investment.
Additionally, the remaining population of Washington smokers may be more difficult to reach through mainstream public health channels, suggesting that funding for
successful tobacco
control programs must be sustained at substantial levels rather than decreased over time.
Back to top
Acknowledgments
This work was funded by the Washington Tobacco Prevention and Control Program.
Back to top
Author Information
Corresponding Author: Julia Dilley, MES, Program Design and Evaluation Services, Multnomah County Health Department/Oregon Department of Human Services, 800 NE Oregon St, Suite 550, Portland, OR 97232. Telephone: 971-673-0589. E-mail: julia.dilley@state.or.us.
Author Affiliations: Kristen Rohde, Clyde Dent, and Michael J. Stark, Program Design and Evaluation Services, Multnomah County Health Department, Oregon Department of Human Services, Portland, Ore; Michael J. Boysun
and Terry Reid, Tobacco Prevention and Control Program, Washington State
Department of Health, Olympia, Wash.
Back to top
References
- The health consequences of smoking: a report of the Surgeon General. Atlanta
(GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2004.
- Best practices for comprehensive tobacco control programs
— August 1999. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Office on Smoking and Health; 1999.
- Farrelly MC, Pechacek TF, Chaloupka FJ.
The impact of tobacco control program expenditures on aggregate cigarette
sales: 1981-2000. [Published erratum in: J Health Econ 2004;23(2):419].
J Health Econ 2003;22(5):843-59.
- Tauras JA, Chaloupka FJ, Farrelly MC, Giovino GA, Wakefield M, Johnston LD, et al.
State tobacco control spending and youth smoking. Am J Public Health 2005;95(2):338-44.
- Stillman FA, Hartman AM, Graubard BI, Gilpin EA, Murray DM, Gibson JT.
Evaluation of the American Stop Smoking Intervention Study (ASSIST): a report of outcomes. J Natl Cancer Inst 2003;95(22):1681-91.
- Washington Tobacco Prevention and Control Council. A tobacco prevention and control plan for Washington State. Olympia (WA): Washington State Department of Health; 1999
[cited 2006 Jul 11]. Available from: http://www.doh.wa.gov/tobacco/program/reports/tobacrep.pdf
*
- Census 2000 data for the state of Washington. Washington (DC): United
States Census Bureau;[cited 2006 Jul 11]. Available from: http://www.census.gov/census2000/states/wa.html
- Centers for Disease Control and Prevention.
Guidelines for school health programs to prevent tobacco use and addiction. MMWR Recomm Rep 1994;43(RR-2):1-18.
- Kim HJ, Fay MP, Feuer EJ, Midthune DN.
Permutation tests for
Joinpoint regression with applications to cancer rates.
[Published erratum in: Stat Med 2001;20(4):655]. Stat Med 2000;19(3):335-51.
- Arthur MW, Hawkins JD, Pollard JA, Catalano RF, Baglioni AJ Jr.
Measuring risk and protective factors for substance use, delinquency, and other adolescent problem behaviors. The Communities That Care
Youth Survey. Eval Rev 2002;26(6):575-601.
- Lifetime health costs of smokers vs. former smokers vs. nonsmokers.
Washington (DC): Center for Tobacco Free Kids; 2006 [cited 2006 Nov 10]. Available
from:
http://www.tobaccofreekids.org/research/factsheets/pdf/0277.pdf *
- Sloan FA, Allsbrook JS, Madre LK, Masselink LE, Mathews CA.
States’ allocations of funds from the tobacco master settlement agreement.
Health Aff (Millwood) 2005;24(1):220-7.
- Koh HK, Judge CM, Robbins H, Celebucki CC, Walker DK, Connolly GN.
The first decade of the Massachusetts Tobacco Control Program. Public Health Rep 2005;120(5):482-95.
- Givel MS, Glantz SA.
Failure to defend a successful state tobacco control program: policy lessons from Florida. Am J Public Health 2000;90(5):762-7.
- Cigarette report for 2003. Washington (DC): U.S. Federal Trade Commission;[cited
2006 Aug 7]. Available from:
http://www.ftc.gov/reports/cigarette05/050809cigrpt.pdf
- Sly DF, Arheart K, Dietz N, Trapido EJ, Nelson D, Rodriguez R, et al.
The outcome consequences of defunding the Minnesota youth tobacco-use prevention program. Prev Med 2005;41(2):503-10.
- Centers for Disease Control and Prevention.
Tobacco use among adults — United States, 2005. MMWR Morb Mortal Wkly Rep 2006;55(42):1145-8.
- Smyser M, Krieger J, Solet D. The King County ethnicity and health survey. Seattle (WA): Public Health — Seattle and King County; 1998.
- Guidelines for using rural-urban classification systems for public health assessment.
Olympia: Washington State Department of Health;[cited 2006 Jul 11]. Available from:
http://www.doh.wa.gov/Data/Guidelines/RuralUrban.htm *
- Tobacco use among U.S. racial/ethnic minority groups — African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics: a report of the Surgeon General. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease
Prevention and Health Promotion, Office on Smoking and Health; 1998.
- Lawrence D, Graber JE, Mills SL, Meissner HI, Warnecke R.
Smoking cessation interventions in U.S. racial/ethnic minority populations: an assessment of the literature. Prev Med 2003;36(2):204-16.
- Stevens P, Carlson LM, Hinman JM.
An analysis of tobacco industry marketing to lesbian, gay, bisexual, and transgender (LGBT) populations: strategies for mainstream tobacco control and prevention. Health Promot Pract 2004;5(3
Suppl):129S-34S.
- Barbeau EM, Leavy-Sperounis A, Balbach ED.
Smoking, social class, and gender: what can public health learn from the tobacco industry about disparities in smoking? Tob Control 2004;13(2):115–20.
Back to top
|
|
