

|

|

Volume
2:
No. 1, January 2005
COMMUNITY CASE STUDY
Bringing Health Policy Issues Front and Center in the
Community: Expanding the Role of Community Health Coalitions
Joel S. Meister, PhD, Jill Guernsey de
Zapien
Suggested citation for this article: Meister JS,
Guernsey de Zapien J. Bringing health policy issues front and
center in the community: expanding the role of community health
coalitions. Prev Chronic Dis [serial online] 2005 Jan
[date cited]. Available from: URL:
http://www.cdc.gov/pcd/issues/2005/
jan/04_0080.htm.
PEER REVIEWED
Abstract
Background
Systemic, environmental, and socioeconomic conditions create
the context in which community members deal with their health
concerns. Comprehensive, community-based chronic disease
prevention interventions should address community-wide or
regional policy issues that influence lifestyle behaviors
associated with chronic diseases.
Context
In two communities along the
Arizona-Mexico border, community coalitions that administered a
comprehensive diabetes prevention and control intervention
expanded their membership to become policy and advocacy
coalitions with broad community representation. These coalitions,
or Special Action Groups (SAGs), identified and prioritized
policy issues that directly or indirectly affect physical
activity or nutrition.
Methods
Local schools were one focus of advocacy. The Centers for
Disease Control and Prevention’s School Health Index was
implemented as part of the overall intervention; the SAGs
supported schools in advocating for more physical education
programs, removal of vending machines, substitution of more
healthful options in vending machines, and changes in health
education curricula. In the broader community, the SAGs promoted
opportunities for walking and bicycling, long-term planning by
their cities and counties, and healthy food choices in local
grocery stores.
Advocacy tactics included attending and making presentations
at city council, school board, parks and recreation, and planning
and zoning commission meetings; participating on long-range
planning committees; organizing an annual community forum for
elected and appointed officials; and presenting healthy food and
cooking demonstrations in local markets.
Consequences
After three years, SAGs
were able to document changes in local policies and practices
attributable to their activities.
Interpretation
The SAGs contributed to
systems changes in their communities and were able to obtain new resources that
support protective behaviors. Also, the advocacy process itself
provided strong positive reinforcement to all participants in this
comprehensive diabetes intervention.
Back to top
Background
Approaches to preventing and controlling chronic diseases,
such as diabetes, must focus on broad lifestyle issues. Such an
approach to preventing and controlling diabetes may include
patients, their families, providers, and the entire community
(1-3).
More recently, and with increasing recognition of the extent
to which individual health-related behavior is shaped by social
and cultural norms and by the physical and policy environment of
a community (4), attention is being given to the systems and
environmental- and community-level factors that contribute to the
behaviors that affect health status and outcomes (4-7). The
Centers for Disease Control and Prevention’s (CDC’s)
Racial and Ethnic Approaches to Community Health (REACH) 2010 program illustrates the increasing emphasis on
changing systems factors using a logic model that includes
changes in change agents and environmental and policy shifts as
precursors of more distal changes in health-related behaviors and
health status (Figure) (8).
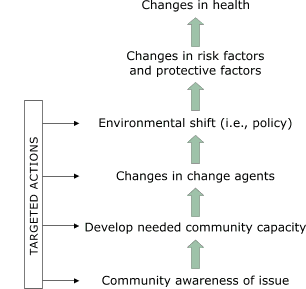
Figure.
The Racial and Ethnic Approaches to Community Health (REACH) 2010 model of change, adapted by the
Southwest Center for Community Health Promotion (8).
The Border Health Strategic Initiative (Border Health
¡SI!) was a comprehensive diabetes prevention and
control program that focused on border communities along the
Arizona-Mexico border (9). The authors adapted the REACH 2010
model so that Border Health ¡SI! included a
significant policy component. The community coalitions,
originally formed to bring together community partners and the
University of Arizona, were challenged to become Special Action
Groups (SAGs) with their own unique role — to effect policy
changes that would promote health in the community.
Back to top
Context
The U.S.-Mexico border has several singular features relevant
to diabetes prevention and control. It is a poor region with
fragmented services, and residents often cross the border —
in both directions — for health care (10). The border region
has a large Hispanic population, with diabetes prevalence
approximately twice the average for non-Hispanic whites (11,12).
Many residents are undocumented and therefore have no access to
health care except for private fee-for-service, which they can
rarely afford, or for emergency services (13).
Along the Arizona-Sonora border, the University of Arizona and
numerous community partners have been working together for the
last twenty years to create health promotion programs and the
joint capacity and infrastructure to address a wide spectrum of
health issues. Based on this ongoing, evolving, and positive
history of collaboration among community-based agencies and the
University of Arizona and our common recognition of the need for
systemic change, the partners in both communities responded
positively to the recommendation that the programmatic partners
of Border Health ¡SI! (those responsible for
specific intervention components) continue to meet as a technical
team while the coalition expand to include other community
members and agencies with a stake in policy. These coalitions
— the SAGs — would be dedicated to planning and
advocating for policy change.
One of the university partners, the Cooperative Extension
Service, was asked and agreed to be the facilitator for the SAGs.
The Mel and Enid Zuckerman Arizona College of Public
Health’s collaboration with Cooperative Extension pre-dates this
project, and the relationship was expanded and strengthened by
the decision to have Cooperative Extension serve as SAG facilitator. As
SAG facilitator, Cooperative Extension used its everyday, longstanding
connection between community and university to strengthen the SAGs.
SAG membership included organizational leaders, program
directors, community health workers (promotores de salud),
and other concerned citizens. Promotores de salud were
critical to forming SAGs (14-16). They provided the outreach and
leadership in every component of the intervention except the
provider component. They brought to the SAGs their knowledge of
what was actually happening in the community day to day. They
also provided the potential leadership for any community
mobilization that might become part of the SAGs’ action
plans.
Back to top
Methods
Fitting policy into the picture
SAG members met first to become familiar with the REACH 2010
model of change. The model’s most novel features were
emphasis on the changes in "change" agents and changes in local
policies that were posited to contribute to changes in behaviors
such as physical activity and nutrition. The "targeted
activities" that drive the model would thus have to consist not
only of the health education programs with which all partners
were familiar and comfortable but with new capacity-building
activities and advocacy interventions that at first seemed
somewhat threatening or exotic. SAG minutes and participant
observation data show that most SAG members, including
organizational leaders, had never appeared before a city council
or other elected body (17).
Distinguishing between program and policy
Our community partners were highly skilled at delivering
health promotion and education, but they had much less experience
dealing with broader policy issues that were not part of
traditional health promotion culture. These issues included, for
example, the physical environment of the community and whether it
supported walking or bicycle-riding or other forms of exercise,
the availability of low-fat, low-sugar foods in grocery stores,
the food products available in school vending machines, and the
use of candy for school fundraising.
Identifying and prioritizing policy issues
As each SAG began to identify and prioritize policy issues in
its community, sustaining the distinction between programs and
policies was the most challenging aspect of developing a policy
agenda. For instance, in initial discussions about changing food
choices, some SAG members suggested a health fair. Others, more
cognizant of the policy issues, wanted to go straight to market
owners or managers and attempt to influence their decisions on
which food products to stock and promote and how food products
were displayed.
As the policy focus became clearer, the SAGs prioritized and
selected issues to be addressed over the following one to three
years. Community A divided its policy goals into short- and
long-term goals. The short-term goal was defined as increasing
opportunities and places for physical activity, and the long-term
goals were defined as making an impact on the county’s
long-range parks and recreation planning and resource allocation.
Community B selected the following policy goals: 1) develop
more parks and recreation areas, 2) work with grocery stores to
offer and promote more healthful foods, and 3) work with
schools to emphasize health curricula and to change the use of
candy and other junk food in the fundraising and reward
structure.
Redefining health as a community-wide issue
Health came to be seen among SAG members as an array of policy
issues that extend well beyond the purview of the experts in the
county health department, the community health center, or school
nurses. SAG members realized that they needed to reach a number
of change agents that included elected officials, business
people, members of the faith community, and educational leaders.
They also needed to bring this broader vision to other health
professionals.
Bringing new members to the coalition
Identifying and then recruiting new SAG members was a critical
step in promoting a policy agenda. Convincing some of them that
health should be one of their issues was a major achievement in
recruiting and retaining them as SAG members (18). These new
recruits included the following (some in Community A, others in
Community B): a chamber of commerce executive director, county
interfaith council director, city manager, parks and recreation
department director, public works department director, planning
and zoning director, hospital administrator, school
superintendent, town librarian, newspaper editor, and police
officer.
Developing an action plan
Once issues were identified and prioritized, the SAGs formed
subgroups to develop action plans for each major issue. Community
A decided to make the SAG indispensable to the county’s
long-range development planning effort by volunteering to serve
on the planning committee, offering the SAG’s own
recommendations for open space, parks and recreation, and
walking/bicycle paths development, and offering data gathered
by its university partner.
Community A also adopted a short-term action plan that
designated a three-month period for mounting a series of health
promotion activities that would culminate in a presentation to
the city council, stressing the need for reallocating (not
increasing, at this time) parks and recreation resources to
promote physical activity among the entire community, and
attending to neighborhood safety, including lighting, sidewalks,
and animal control. The SAG in Community A contracted with a
consultant to design a compelling fact sheet that would be used
in its presentation to the city council and other policy-making
bodies.
In Community B, the SAG initiated an annual community forum
designed to educate policy makers, advocate for policy change,
and hold elected officials accountable for their support, or lack
thereof, of policies to promote health. The forum was designed so
that representatives of the SAG and other community groups could
first present their activities and policy agendas to public
officials who were invited to attend. After the community
presentations, elected and appointed officials were invited to
respond, and then the forum was opened to discussion.
The promotores in this community’s SAG mobilized
their constituents to advocate for new parks in one of the small
towns near the border and in an unincorporated area of the county
that provided few public services to its residents. These
promotores had been leading the community walking groups
and nutrition classes that were one component of Border Health
¡SI!. Now they and members of these groups went before
the county board of supervisors to advocate for parks in their
neighborhoods.
The SAG in Community B also worked with the schools component
of Border Health ¡SI! to promote changes in the
curriculum and the use of junk foods. While the schools component
of Border Health ¡SI! worked with the School Health
Index and the school health teams, the SAG also kept in close
contact with the school superintendent and individual principals
to promote change and monitor progress.
Back to top
Consequences
Results that can be traced directly to the actions of the SAGs
are described below.
Community A
- New walking paths were incorporated into the county’s
development plan.
- A new Wal-Mart Supercenter added a perimeter walking path to its
construction plan.
- Plans to terminate physical education at a local school were
halted.
- Health-related articles now appear regularly in the local
newspaper.
Community B
- Two Community Development Block Grants were obtained for parks
and walking paths. The SAG also succeeded in convincing the local
school district to donate land for one of the parks. This donation made it
possible to use the grant to fund landscaping and to purchase
exercise equipment and other amenities.
- Grocery stores in the target communities initiated healthy
food demonstrations one to two times per month. These
demonstrations were organized and conducted by
promotores.
- Stores began stocking more healthy products.
- Sales of food featured in the healthy food demonstrations
increased.
- The SAG received the 2002 Mayor’s Physical Activity
Leadership Award.
Of the many lessons learned from the SAGs, the following are
among the most salient:
- A comprehensive approach to community health promotion
requires a policy component.
- Commitment and organizational involvement of the key
community-based health organizations are necessary.
- Promotores must be involved as change agents.
- Social action focused on policy change can energize a
coalition, giving it a raison d’être beyond merely
coordinating activities, and can contribute to its
sustainability.
- The SAG created an engine for change on community health
issues.
- Short-term successes contribute to long-term effectiveness of
SAGs.
- Consciousness-raising about public health issues among those
who are not public health practitioners is important to effecting
policy change. Convincing people that health is their business
regardless of what they do professionally is critical to
recruiting opinion leaders to join a SAG and to activating local
or regional policy makers.
- Sustainability is made possible by a SAG in several ways. SAG
action motivates members to continue their advocacy efforts as
new issues arise and successes are achieved. SAG advocacy creates
links between programs and policies that may result in local or
regional agencies incorporating successful programs and new
policies into their standard mode of operation. SAGs create
strategic alliances with non-health specific groups that may lead
to new funding opportunities that help sustain multiple
components of a community health intervention. SAGs provide an
opportunity for promotores to serve as community change
agents.
The experience of the SAGs and the results of their advocacy
have been reported to the community in a variety of ways.
Foremost has been the publication of numerous articles in local
newspapers — made possible, no doubt, by SAG membership of
newspaper editors or reporters in each community. Presentations
at conferences, including the U.S.-Mexico Border Health
Association, Arizona Public Health Association, CDC Diabetes
Translation Conference, and others provided a mechanism for
dissemination of lessons learned to other border communities
throughout the region. SAG activities are also reported regularly
to the Community Action Board (CAB) of the Southwest Center for
Community Health Promotion. The CAB is, in effect, a super-SAG
for all communities involved in Border Health ¡SI!
and other border community health interventions of the Mel and
Enid Zuckerman Arizona College of Public Health.
Back to top
Interpretation
After the fact, it is difficult to imagine the Border
Health ¡SI! program without its SAG policy-change
component. This is so not only because the SAGs contributed to
systems changes in their communities and were able to obtain new
resources that support protective behaviors but also because the
advocacy process itself provided such strong positive
reinforcement to all participants in this comprehensive diabetes
intervention. The results of evaluation interviews with SAG
members and the administration of the Wilder Collaboration
Factors Inventory (19) strongly suggest that participation in the
SAG resulted in:
- Improved health behaviors within members’ own
organizations.
- Better understanding of community needs.
- Closer relationships with other agencies represented on the
SAGs.
SAG members also took credit for:
- Building awareness among policy makers.
- Influencing community-wide resource allocation.
- Gaining support for SAG initiatives by city, county, and
school-governing bodies.
- Working collaboratively with decision makers in the planning
process.
Context always plays an important role in defining the issues
to be addressed and the boundaries of possible action and change
in a given community. In this case, context included the border
geography and demography, especially the preponderance of
Hispanics in these communities, the persistent poverty and lack
of formal education among much of the population, and the
pervasiveness of diabetes. One might suppose that such a context
would militate against effective organization for policy change.
We did not find this to be true. On the contrary, the brief
history of the SAGs confirms our prior experience — that in
these have-not communities along the U.S.-Mexico border, there is
a largely untapped reservoir of intelligence and thirst for
knowledge, concern about community conditions, desire for change
and willingness to take risks, and, most important, a willingness
to act collectively for the common good.
From the perspective of university-based participatory-action
researchers, creating a collaborative policy-change initiative,
whether stand-alone or as part of a broad health intervention,
requires a strong, positive university-community partnership
(20,21). Those partnerships take time to build and require mutual
trust (22-25). To that we would add that the researcher’s
goal is to be a partner in the fullest sense, not merely to
provide technical assistance, advise, and evaluate but to be an
integral part of planning, decision making, and action —
without inadvertently assuming the leadership of what is, after
all, a community coalition. It is the action taken by all
of the partners that results in the kind of impact that lives on
in the community.
Back to top
Acknowledgments
Funding for this project comes from the Division of Diabetes Translation,
National Center for Chronic Disease Prevention and Health Promotion, Centers
for Disease Control and Prevention.
Back to top
Author Information
Corresponding author: Joel S. Meister, PhD, Associate
Professor of Public Health and Director of the Public Health
Policy and Management Concentration, Mel and Enid Zuckerman
Arizona College of Public Health, 1501 N Campbell Ave, PO Box
210228, Tucson, AZ 85724-5163. Telephone: 520-318-7270, ext 19.
E-mail: jmeister@u.arizona.edu.
Author affiliations: Jill Guernsey de Zapien, Associate Dean
for Community Programs, Mel and Enid Zuckerman Arizona College of
Public Health, Tucson, Ariz.
Back to top
References
- Teufel-Shone NI, Drummond R. La diabetes y la unión:
familiar curriculum for the Border Health Strategic
Initiative, a comprehensive community based diabetes prevention
and control program. Tucson (AZ): The University of Arizona; 2002.
- Veazie MA, Teufel-Shone NI, Silverman GS,
Connolly AM, Warne S, King BF, et al.
Building
community
capacity in public health: the role of action-oriented
partnerships. J Public Health Manag Pract 2001;7(2):21-32.
- Cohen SJ, Meister JS, de Zapien JG.
Special action groups for policy change and infrastructure support to foster
healthier communities on the Arizona-Mexico border. Public Health Rep 2004;119:40-7.
- Wilcox A, Knapp A.
Building
communities that create
health. Public Health Rep 2000;115:139-43.
- Butterfoss FD, Goodman RM, Wandersman A.
Community
coalitions for prevention and health promotion. Health Educ
Res 1993;8(3):315-30.
- Merzel C, D’Afflitti J.
Reconsidering
community-based health promotion: promise, performance, and
potential. Am J Public Health 2003;93(4):557-74.
- Roussos ST, Fawcett SB.
A
review of collaborative
partnerships as a strategy for improving community health. Ann
Review Public Health 2000;21:369-402.
- Gerberding JL.
Racial and
ethnic approaches to
community health (REACH 2010): addressing disparities in health
– at a glance. Atlanta (GA): Centers for Disease Control and
Prevention; 2004.
- Cohen S, Ingram M. Border Health
Strategic Initiative: overview and introduction to a community-based model for
diabetes prevention and control. Prev Chronic Dis [serial online]
2005 Jan.
- U.S. Department of Health and Human Services.
Assuring a healthy future along the U.S.-Mexico
border.
Washington (DC): U.S. Department of Health and Human Services; 1999.
- Flood T, Lebowitz MD, De Zapien J, Staten L, Rosales C.
Douglas community health survey: diabetes and health care in
Arizona on the Mexican border. Phoenix (AZ): ADHS; 1999
- Centers for Disease Control and Prevention.
Diabetes: disabling,
deadly, and on the rise. Atlanta (GA): U.S. Department of Health and Human
Services; 2004.
- De Zapien JG. Making a difference for prevention: policy change in
communities at the US-Mexico Border. Washington (DC): 18th National
Conference on Chronic Disease Prevention and Control; 2004 Feb 18-20.
- Meister JS, et al. The community health worker
evaluation tool kit. Tucson (AZ): Mel and Enid Zuckerman Arizona College of Public Health,
University of Arizona; 2000. Available from: URL:
http://www.publichealth.arizona.edu/chwtoolkit/*.
- Meister JS. Community outreach and community
mobilization: options for health care at the U.S.-Mexico border. Washington
(DC): U.S. Department of Health and Human Services; 1997.
- Rosenthal EL, et al. The national community health
advisor study. Tucson (AZ): Mel and Enid Zuckerman Arizona
College of Public Health, University of Arizona and The Annie E. Casey
Foundation; 1998. Available from: URL: http://www.aecf.org*.
- Reinschmidt K, Dunne A. Personal communication and meeting minutes; 2003.
- Castro FG, Elder J, Coe K, Tafoya-Barraza
HM, Moratto S, Campbell N, et al.
Mobilizing
churches for health promotion in Latino
communities. J Natl Cancer Inst Monogr 1995(18):127-35.
- Mattessich P, Murray-Close M, Monsey B. The Wilder
Collaboration Factors Inventory: assessing your collaboration's
strengths and weaknesses. Saint Paul (MN): Amherst H. Wilder Foundation; 2001.
- Israel BA, Schulz AJ, Parker EA, Becker AB, Allen A, Guzman JR. Critical issues in developing and following
community-based participatory research principles. In: Minkler M, Wallerstein N, editors. Community-based
participatory research
for health. San Francisco (CA): Jossey-Bass; 2003. p. 56-73.
- National Association of County and City Health Officials. Mobilization for action through
partnerships and planning (MAPP).
Washington (DC): National Association of County and City Health Officials. Available
from: URL: http://www.naccho.org/project77.cfm*.
- Israel BA, Schulz AJ, Parker EA, Becker AB.
Review of
community-based research:
assessing partnership approaches to improve public health. Annu
Rev Public Health 1998;19:173-202.
- Weiss ES, Anderson RM, Lasker RD.
Making the
most of
collaboration: exploring the relationship between partnership
synergy and partnership functioning. Health Educ
Behav 2002;29(6):683-98.
- Alexander JA, et al. Leadership in collaborative
community health partnerships. Nonprofit management and
leadership 2001;12(2):159-75.
- Harris E, Wills J.
Developing
healthy local communities
at local government level: lessons from the past decade. Aust N Z J Public
Health 1997;21(4 Spec No):403-12.
Back to top
*URLs for nonfederal organizations are provided solely as a
service to our users. URLs do not constitute an endorsement of any organization
by CDC or the federal government, and none should be inferred. CDC is
not responsible for the content of Web pages found at these URLs.
|
|
