 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Promoting Oral Health: Interventions for Preventing Dental Caries, Oral and Pharyngeal Cancers, and Sports-Related Craniofacial InjuriesA Report on Recommendations of the Task Force on Community Preventive ServicesCHAIR Jonathan E. Fielding, M.D., M.P.H., M.B.A. VICE-CHAIR Patricia Dolan Mullen, Dr.P.H. Ross C. Brownson, Ph.D. Mindy Thompson Fullilove, M.D. Fernando A. Guerra, M.D., M.P.H. Alan R. Hinman, M.D., M.P.H. George J. Isham, M.D. Garland H. Land, M.P.H. MEMBERS Charles S. Mahan, M.D. Patricia A. Nolan, M.D., M.P.H. Susan C. Scrimshaw, Ph.D. Steven M. Teutsch, M.D., M.P.H. Robert S. Thompson, M.D. CONSULTANTS Robert S. Lawrence, M.D. J. Michael McGinnis, M.D. Lloyd F. Novick, M.D., M.P.H. FORMER MEMBERS Patricia A. Buffler, Ph.D., M.P.H. Mary Jane England, M.D.* Caswell A. Evans, Jr., D.D.S., M.P.H.* David W. Fleming, M.D.* The following CDC staff members prepared this report: Benedict I. Truman, M.D., M.P.H. Barbara F. Gooch, D.M.D., M.P.H. Iddrisu Sulemana, M.P.H., M.A. in collaboration with Alice M. Horowitz, Ph.D. Helen C. Gift, Ph.D. Caswell A. Evans, Jr., D.D.S., M.P.H.* SummaryThe Task Force on Community Preventive Services (the Task Force) has conducted systematic reviews of the evidence of effectiveness of selected population-based interventions to prevent and control dental caries (tooth decay), oral (mouth) and pharyngeal (throat) cancers, and sportsrelated craniofacial injuries. The Task Force strongly recommends community water fluoridation and schoolbased or schoollinked pit and fissure sealant delivery programs for prevention and control of dental caries. Using the rules of evidence it has established, the Task Force found insufficient evidence of effectiveness or ineffectiveness of the remaining interventions reviewed. Therefore, the Task Force makes no recommendation for or against use of statewide or communitywide sealant promotion programs, populationbased interventions for early detection of precancers and cancers, or populationbased interventions to encourage use of helmets, facemasks, and mouthguards to reduce oral-facial trauma in contact sports. The Task Force's finding of insufficient evidence indicates the need for more research on intervention effectiveness. Until the results of such research become available, readers are encouraged to judge the usefulness of these interventions by other criteria. This report presents additional information regarding the recommendations, briefly describes how the reviews were conducted, and provides information designed to help apply the strongly recommended interventions locally. BACKGROUNDDespite substantial improvements in oral health for most persons living in the United States during the 20th century, the nation spends an estimated $60 billion annually on dental services (1), including approximately 500 million visits to dental offices (2). In 1996, estimated inpatient hospital charges for diseases of the mouth and disorders of the teeth and jaw were $451 million (3). Dental caries, oral cancers, and sports-related craniofacial injuries are potentially preventable conditions. The financial and human costs associated with these conditions, including mortality, indicate the need for interventions that promote oral health and prevent disease for all persons, regardless of age, throughout their life span. The prevalence of dental caries (i.e., the percentage of persons with >1 decayed, missing, or filled teeth) in permanent teeth increases with age, from 26% among persons aged 5--11 years to 67% among persons aged 12--17 years and 94% for dentate adults (with >1 natural teeth) aged >18 years (4,5). The prevalence of dental caries among children aged 12--17 years has declined from 90% during 1971--1974 to 67% during 1988--1991. Severity (i.e., the mean number of decayed, missing, or filled teeth) has declined from 6.2 to 2.8 during this period (4,6). Eighty percent of dental caries identified in permanent teeth of children aged 5--17 years in the United States occur in 25% of children (4,6,7). Lower-income, Mexican-American, and African-American children and adults have more untreated decayed teeth than their higher-income or non-Hispanic white counterparts (4,5,8,9). Among lowincome children, approximately one third have untreated caries in primary teeth that could be associated with pain, difficulty in eating, and underweight (9). Dental caries on smooth tooth surfaces (those without pits and fissures) also has decreased markedly. Recent data indicate that approximately 90% of caries in permanent teeth of children occur in tooth surfaces with pits and fissures, and approximately two thirds are on the chewing surfaces alone (4,7,10). Each year, oral (mouth) and pharyngeal (throat) cancers, which are mainly squamous cell carcinomas, are diagnosed in approximately 30,000 U.S. residents, and approximately 8,000 persons die of these diseases (7,11,12). Oral and pharyngeal cancers are the fourth, seventh, and fourteenth most common cancers among African-American men, white men, and all women, respectively (11). They are most often diagnosed at late stages and treated by methods (e.g., surgery, radiation, and chemotherapy) that can be disfiguring and costly (13). Overall relative 5year survival rates are approximately 54%, and mortality is nearly twice as high among certain minorities (especially African-American men) as among whites (11,12). Epidemiologic studies indicate that approximately one third of all dental injuries and approximately 19% of head and face injuries are sports-related (7,8,14--16). During 1997--1998, persons aged 5--24 years accounted for 2.6 million (70%) of the 3.7 million emergency department visits per year for sports-related injuries among persons of all ages. Approximately 22% of the average annual estimate of visits were for craniofacial injuries to the brain and skull, face, scalp, and neck (14). More widespread use of effective population-based interventions could help reduce the morbidity, mortality, and economic burden associated with dental caries, oral cancers, and sports-related craniofacial injuries. This report and other related publications provide guidance from the Task Force on Community Preventive Services (the Task Force) to decision makers in state and local health departments, managed care organizations, purchasers of health care, persons responsible for funding public health programs, and others who have interest in or responsibility for improving oral and related general health in all segments of the population. INTRODUCTIONThe Task Force is developing the Guide to Community Preventive Services (the Community Guide) with support from CDC, the U.S. Department of Health and Human Services (DHHS), other federal agencies, and other public and private partners. The recommendations presented in this report were developed by the Task Force and are not necessarily the recommendations of CDC, DHHS, or other participating organizations. This MMWR report is one in a series of reports on systematic reviews conducted for the Community Guide, a resource that will include multiple systematic reviews, each focusing on population-based opportunities to promote health and prevent disease or injury. This report provides an overview of the process used to select and review evidence and summarizes the Task Force's recommendations on community interventions to reduce dental caries, oral cancers, and sports-related craniofacial injuries. A full presentation of the recommendations, supporting evidence (i.e., discussions of applicability, additional benefits, potential harms, and barriers to implementation), economic evaluations of recommended interventions (when available), and remaining research questions will be published in the American Journal of Preventive Medicine in 2002. More information regarding this MMWR report is available from CDC's Division of Oral Health, National Center for Chronic Disease Prevention and Health Promotion at (770) 4885301. Copies of this report are available electronically at <http://www.thecommunityguide.org>. METHODSDetailed methods used to conduct systematic reviews and link evidence to recommendations for the Community Guide have been described elsewhere (17). In brief, for each Community Guide topic, a multidisciplinary development team conducts a review by
The coordination and consultation* teams generated a comprehensive list of strategies and created a priority list of interventions for review based on their perceptions of the importance of each intervention and the extent to which the interventions were practiced in the United States. These teams focused on interventions to prevent and control dental caries (including community water fluoridation, schoolbased or schoollinked pit and fissure sealant delivery programs, and communitywide sealant promotion programs), oral cancers, and sports-related craniofacial injury because these important health problems contribute substantially to annual dental care expenditures, serve as selected indicators of the need for preventive services, and address several Healthy People 2010 objectives (Table 1). To be included in the review of effectiveness of an intervention, a study had to a) involve primary investigation of an intervention selected for evaluation;† b) be published in English on or before December 31, 2000; c) be conducted in established market economies* (unless such studies were unavailable or scarce, in which case, relevant studies conducted in other countries were included); and d) compare outcomes among groups of persons exposed to the intervention with outcomes among groups of persons not exposed or less exposed to the intervention. Time and resource constraints precluded review of certain candidate interventions. Examples include a) school-based programs that deliver health education, fluoride rinse and tablets, or oral examinations and referral, either as single- or multicomponent interventions; b) programs to prevent early childhood caries; c) public, professional, and schoolbased education; and d) multicomponent interventions that target >2 health outcomes. For each intervention reviewed, the team developed an analytic framework indicating possible causal links between the intervention under study and predefined outcomes of interest. These outcomes included dental caries, oral cancers or precancers, and sports-related craniofacial injuries. These conditions were selected because they are common, sometimes life-threatening, costly in terms of resources and quality of life, or preventable by strategies already in widespread use. Moreover, promoting oral health is a fundamental concern of public health practice, not exclusively of dental health practitioners. Prevention of other important craniofacial health conditions (e.g., periodontal diseases, developmental anomalies) has been reviewed elsewhere (8). Studies that met the inclusion criteria also had to meet the quality criteria. Each study was evaluated using a standardized abstraction form and assessed for suitability of the study design and threats to validity. On the basis of the number of threats to validity, studies were characterized as having good, fair, or limited execution (17). The strength of the body of evidence of effectiveness was characterized as strong, sufficient, or insufficient on the basis of the number of available studies, the suitability of study designs for evaluating effectiveness, the quality of execution of the studies, the consistency of the results, and the effect size† (17). The Community Guide systematically links evidence to recommendations (17). The strength of evidence of effectiveness corresponds directly to the strength of recommendations (e.g., strong evidence of effectiveness corresponds to an intervention being strongly recommended, and sufficient evidence corresponds to an intervention being recommended). Other types of evidence also can affect a recommendation. For example, evidence of harms resulting from an intervention might lead to a recommendation that the intervention not be used, even if it is effective in improving certain outcomes. A finding of insufficient evidence of effectiveness does not result in recommendations for or against an intervention's use but is important for identifying areas of uncertainty and continuing research needs. In contrast, sufficient or strong evidence of ineffectiveness leads to a recommendation that the intervention not be used. Although the option exists, the Task Force has yet to use economic information to modify recommendations. RESULTSA systematic search of the Medline database* (1966 through December 2000) yielded approximately 4,000 journal article citations potentially relevant to the review. In addition, members of the development team manually searched reference lists and consulted with specialists in the field to identify other relevant citations, including reports on studies of the economics of the interventions being examined. Of all citations considered, 130 studies met the inclusion criteria and were abstracted; 94 of these were excluded because of limitations in their execution or design and were not considered further. The remaining 36 studies were considered qualifying studies. The assessment of effectiveness for the five interventions discussed in this report was based on the systematic review and evaluation of the 36 qualifying studies, all of which had good or fair quality of execution (citations and details available at <http://www.thecommunityguide.org>). Based on the evidence of effectiveness, the Task Force strongly recommended community water fluoridation and school-based or school-linked pit and fissure sealant delivery programs (i.e., those that also involve a private dental practice or public dental clinic) but did not make a recommendation for or against the other three interventions because of insufficient evidence of effectiveness or ineffectiveness (Table 2). The available evidence also did not permit the Task Force to render a judgment on the relative effectiveness of school-based versus school-linked sealant delivery programs. USING THESE RECOMMENDATIONS IN COMMUNITIES AND HEALTHCARE SYSTEMSGiven that oral health conditions cause considerable morbidity and even mortality, and that activities to promote oral health are ongoing throughout the United States, the recommendations in this report should be relevant to most communities. Communities, school systems, health-care systems, and oral health practitioners should consider starting program planning and implementation cycles by
To decide which combination of interventions is most likely to meet local objectives, decision makers should consider state and local laws and regulations, resource availability, administrative structures, and economic and social environments of implementing organizations and practitioners. They should also consider recommendations and evidence provided in this and other reports, including those of the U.S. Surgeon General (8); National Health Service Centre for Reviews and Dissemination, University of York (18); CDC (19,20); Institute of Medicine (21); and Canadian Task Force on Preventive Health Care (22,23). The Task Force has strongly recommended community water fluoridation and school-based or school-linked pit and fissure sealant delivery programs. Although the Task Force has not used economic information to modify recommendations, this information, when available, can help local policy makers in the decision-making process. If local goals and resources permit, the use of these interventions should be initiated or increased. In addition, these interventions should be considered in the context of other communitywide, provider-based, and individual strategies for preventing or controlling dental caries in communities (7,8,19). The Task Force's decision to make no recommendation for or against the use of three other reviewed interventions at the community level (i.e., statewide or communitywide sealant promotion programs; population-based interventions for early detection of precancers and cancers; and population-based interventions to encourage use of helmets, facemasks, and mouthguards in contact sports) indicates the need for high-quality (as defined previously [17]) research on their effectiveness. Until the results of such research become available, readers can judge the usefulness of these interventions based on other criteria. Although the effectiveness of communitywide sealant promotion programs remains unknown, the clinical safety and effectiveness of sealants have been established (24,25). Where organized efforts are being considered to reduce the burden of oral cancer, the findings presented here should be considered with recommendations of other groups (8,20,22,26,27). For example, more widespread use of effective strategies to reduce tobacco use, an important cause of oral and pharyngeal cancer (8,27--29), should be encouraged, and clinicians can consider periodic oral examinations of persons who engage in risk behaviors (i.e., tobacco use or excessive alcohol consumption) or manifest suspicious symptoms (8,22). Although the Task Force did not make a communitywide recommendation regarding use of protective head and face equipment in contact sports, the frequency and severity of head, face, and oral injuries have decreased in certain sports since the use of helmets, facemasks, and mouthguards became mandatory in selected organized contact sports (e.g., football, ice hockey) (30,31). ADDITIONAL INFORMATION REGARDING THE COMMUNITY GUIDECommunity Guide topics are prepared and released as each is completed. A compilation of the recommendations and supporting evidence for these topics will be published in book form. Upcoming topics in 2001--2002 include the sociocultural environment, cancer, and sexual behavior. The findings from systematic reviews on vaccinepreventable diseases, tobacco use prevention and reduction, motor vehicle occupant injury, and diabetes have been published. Additional information regarding these reports, the Task Force, and the Community Guide is available at <http://www.thecommunityguide.org>. References
* Consultants on oral health were Myron Allukian, Jr., D.D.S., M.P.H., Boston Public Health Commission, Boston, Massachusetts; Eugenio Beltran, D.M.D., Dr.P.H., Division of Oral Health, National Center for Chronic Disease Prevention and Health Promotion, CDC, Atlanta, Georgia; Aljernon Bolden, D.M.D., M.P.H., Boston University, Goldman School of Dental Medicine, Boston, Massachusetts; Maria Teresa Canto, D.D.S., M.P.H., National Institute of Dental and Craniofacial Research, National Institutes of Health, Bethesda, Maryland; Timothy R. Collins, D.D.S., M.P.H., Los Angeles County Department of Health Services, Los Angeles, California; Stephen B. Corbin, D.D.S., M.P.H., Special Olympics, Inc., Washington, D.C.; Teresa A. Dolan, D.D.S., M.P.H., University of Florida College of Dentistry, Gainesville, Florida; Thomas F. Drury, Ph.D., National Institute of Dental and Craniofacial Research, National Institutes of Health, Bethesda, Maryland; Harold Goodman, D.D.S., M.P.H., Office of Oral Health, Maryland State Health Department, Baltimore, Maryland; Larry Hill, D.D.S., M.P.H., Cincinnati Health Department, Cincinnati, Ohio; Lori Hutwagner, M.S., Division of Public Health Surveillance and Informatics, Epidemiology Program Office, CDC, Atlanta, Georgia; Amid I. Ismail, B.D.S., M.P.H., Dr.P.H., University of Michigan School of Dentistry, Ann Arbor, Michigan; Robert Isman, D.D.S., M.P.H., Office of MediCal Dental Services, California Department of Health Services, Sacramento, California; William Kohn, D.D.S., M.P.H., Division of Oral Health, National Center for Chronic Disease Prevention and Health Promotion, CDC, Atlanta, Georgia; Jayanth Kumar, D.D.S., M.P.H., New York State Health Department, Albany, New York; Raymond A. Kuthy, D.D.S., M.P.H., University of Iowa College of Dentistry, Iowa City, Iowa; Corinne E. Miller, D.D.S., Ph.D., Michigan Department of Community Health, Lansing, Michigan; R. Gary Rozier, D.D.S., M.P.H., School of Public Health, University of North Carolina, Chapel Hill, North Carolina; Randy H. Schwartz, M.S.P.H., Department of Human Services, Bureau of Health, Augusta, Maine; Robert H. Selwitz, D.D.S., M.P.H., National Institute of Dental and Craniofacial Research, National Institutes of Health, Bethesda, Maryland; Mark Siegal, D.D.S., M.P.H., Bureau of Oral Health Services, Ohio State Health Department, Columbus, Ohio; Janet Stansell, M.L.M., National Center for Chronic Disease Prevention and Health Promotion, CDC, Atlanta, Georgia; Scott L. Tomar, D.M.D., Dr.P.H., University of Florida College of Dentistry, Gainesville, Florida; Steven Uranga McKane, D.M.D., M.P.H., SUM Consulting, West Hills, California; B. Alex White, D.D.S., Dr.P.H., Kaiser Permanente Center for Health Research, Portland, Oregon. † Studies of the effectiveness of school-based programs that require use of protective sports equipment were reviewed as part of populationbased interventions to encourage use of helmets, facemasks, and mouthguards to reduce oral-facial trauma. Available studies of educational interventions were reviewed if they involved the five interventions described in Table 2. * Established market economies as defined by the World Bank are Andorra, Australia, Austria, Belgium, Bermuda, Canada, Channel Islands, Denmark, Faeroe Islands, Finland, France, Former Federal Republic of Germany, Germany, Gibraltar, Greece, Greenland, Holy See, Iceland, Ireland, Isle of Man, Italy, Japan, Liechtenstein, Luxembourg, Monaco, The Netherlands, New Zealand, Norway, Portugal, San Marino, Spain, St. Pierre and Miquelon, Sweden, Switzerland, the United Kingdom, and the United States. † Studies qualified for the final summary estimates of effectiveness if they provided sufficient detail to support quality scoring, had an acceptably small number of limitations in execution or design, and provided an appropriate measure for summarizing (e.g., median and range) the effectiveness of the intervention on a single scale. * Available at <http://www.ncbi.nlm.nih.gov/PubMed> (accessed October 17, 2001). Table 1 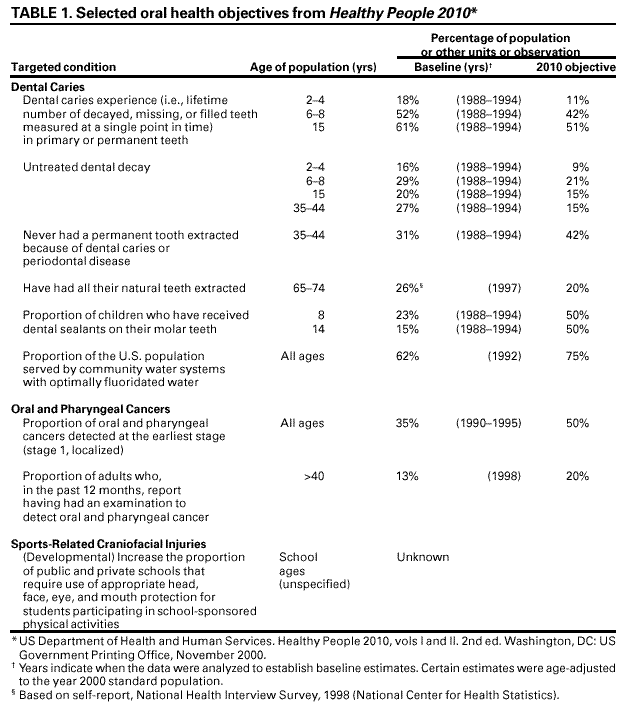 Return to top. Table 2 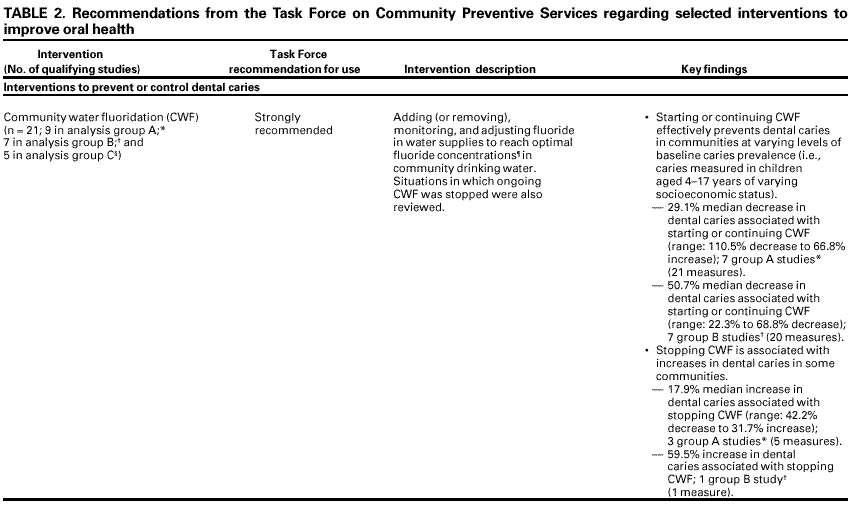  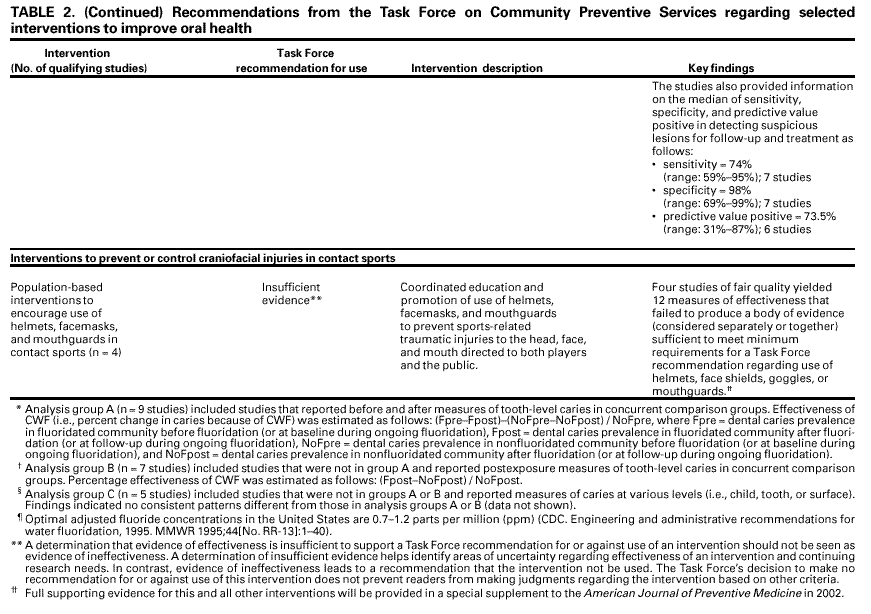 Return to top.
All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 11/30/2001 |
|||||||||
This page last reviewed 11/30/2001
|