 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Use of Social Networks to Identify Persons with Undiagnosed HIV Infection --- Seven U.S. Cities, October 2003--September 2004An estimated 250,000 persons living with human immunodeficiency virus (HIV) in the United States are not aware of their infections and their risk for transmitting HIV (1). As part of CDC's Advancing HIV Prevention Initiative, identifying persons with undiagnosed HIV infection and linking them to medical care and prevention services is a national priority (2). In 2003, a 2-year demonstration project was begun with nine community-based organizations (CBOs) in seven cities to evaluate the effectiveness of using a social network strategy (3) at multiple sites to identify persons at risk for HIV infection and direct them to HIV counseling, testing, and referral (CTR). In this strategy, HIV-positive persons and HIV-negative persons at high risk (i.e., recruiters) are enlisted to recruit for CTR persons from their social, sexual, and drug-use networks (i.e., network associates [NAs]) believed to be at risk for HIV infection (4). This report summarizes preliminary results from the first year of this 2-year project, which indicated that 133 persons recruited 814 NAs, resulting in 46 newly identified HIV infections (approximately 6% of all persons tested). Health departments and CBOs should consider this strategy as an effective method for recruiting persons for CTR and identifying those with undiagnosed HIV infection. The nine CBOs participating in the social network project provided HIV-related services in seven cities*. Although details differed among sites (e.g., identification of recruiters or use of incentives), all CBOs used the same basic methods. First, CBO staff members invited clients who were HIV positive to recruit NAs, including sex and needle-sharing partners the recruiters believed did not know their HIV status and might have been at risk for HIV infection. Certain CBOs also received referrals of recruiters from collaborating agencies. Next, recruiters were interviewed to elicit information about their networks and were coached by CBO staff members on strategies for discussing HIV and CTR with NAs. Although CBO interviewers talked with recruiters about their NAs in detail, information on the specific nature of the recruiter-NA relationship (e.g., sex or needle-sharing partners) was not requested. Typically, recruiters then contacted their NAs and accompanied or referred them to a designated CTR site (on certain occasions, at a recruiter's request, NAs were contacted by CBO outreach staff). Those NAs not accompanied to a CTR site received referral cards to present to CTR staff members to indicate who recruited them for testing. NAs with positive tests were referred for medical care, HIV risk-reduction services, partner counseling and referral services (PCRS), and other services as needed (e.g., sexually transmitted disease [STD] screening, substance abuse treatment, and mental health treatment). NAs with negative HIV tests were assessed to determine HIV behavioral risks† and the need for follow-up testing, and referred for HIV risk-reduction and other appropriate services. CBOs typically provided a small incentive (e.g., gift card) to recruiters for each NA successfully recruited and tested; some provided incentives to NAs who completed HIV testing. At the discretion of CBO staff, HIV-positive NAs and HIV-negative NAs at high risk (tested during the project) were invited to become recruiters, enabling identification and testing of additional NAs in a recruiter's network. Recruiter and NA data were collected during October 2003--September 2004. Pearson chi square or Fisher's exact tests were used to test associations between selected characteristics of recruiters and NAs and prevalence of newly identified HIV-positive NAs. For outcomes significant at the p<0.05 level, pairwise comparisons were performed by using an adjustment for multiple comparisons. During October 2003--September 2004, a total of 133 recruiters (Table 1) were enlisted from the nine CBO sites (range: three to 29 recruiters). A total of 814 NAs were recruited for HIV testing, including 737 (90%) by recruiters on their own; 67 (8%) by CBO outreach workers, based on information provided by recruiters; and five (1%) by recruiters and outreach workers together. Recruitment method was not available for five (1%) NAs. Of the 133 recruiters, 80 (60%) were male, 43 (32%) were female, and 10 (8%) were transgender§ persons. Most recruiters were either HIV positive (77%) or HIV negative but at high risk (16%). A total of 113 (85%) were aged >35 years; and 125 (94%) were from racial/ethnic minorities, including 88 (66%) who were non-Hispanic black and 34 (26%) who were Hispanic. Fifty-four (41%) were heterosexuals at high risk, 39 (29%) were men who have sex with men (MSM), 15 (11%) were men who have sex with men and were injection-drug users (MSM/IDUs), and 12 (9%) were IDUs. Recruiter proficiency was assessed by calculating a network index (i.e., number of NAs recruited divided by number of recruiters) and by calculating prevalence of newly identified HIV infection among NAs; recruitment information was not available for 59 (7%) NAs (Table 1). The network index was highest for recruiters who were aged 25--34 years, Hispanic, IDUs, and MSM/IDUs, indicating that recruiters with these characteristics were most proficient at recruiting NAs for testing. However, the prevalence of newly identified HIV infection was highest among NAs recruited by transgender persons and MSM. Of the 814 NAs tested, 669 (82%) were HIV negative and at high risk, 79 (10%) were HIV negative at low or unknown risk, 46 (6%) had newly identified HIV infections, 12 (2%) had HIV diagnosed previously, and eight (1%) did not have test results available (Table 2). Information on referral to care was incomplete in these preliminary data. A total of 677 (83%) NAs were aged >25 years, 544 (67%) were male, 477 (59%) were heterosexuals at high risk, 383 (47%) were non-Hispanic blacks, and 310 (38%) were Hispanics. A total of 748 (92%) NAs were identified directly by a recruiter; 66 (8%) were identified through another NA. Prevalence of newly identified HIV infections among NAs varied significantly by sex/gender and HIV risk group; the highest prevalences were recorded among MSM/IDU (26%), transgender persons (20%), and MSM (16%) (Table 2). Prevalence of newly identified HIV infections for NAs identified directly by recruiters (6%) was similar to that for NAs identified indirectly through another NA (8%). At each site, recruiters also identified venues they frequented (e.g., substance abuse centers, bars/clubs, and homeless shelters) where they believed NAs at high risk could be reached; 110 (14%) NAs received CTR at these venues, but none were HIV positive. Reported by: C Emerson, MSW, Continuum; T Brown, Tenderloin AIDS Resource Center, San Francisco, California. S Illemsky, Whitman Walker Clinic, Washington, DC. L Jean-Jacques, Center for Multicultural Wellness and Prevention, Orlando, Florida. R Boyles, Southwest Louisiana Area Health Education Center, Lafayette, Louisiana. G Simpson, MA, Multicultural AIDS Coalition, Boston, Massachusetts. N Carrasquillo, Latino Commission on AIDS, New York, New York. D Daltry, MSW, ActionAIDS; W Maldonado, Congreso de Latinos Unidos, Philadelphia, Pennsylvania. L Kimbrough, MS, H Hancock, PhD, S Dooley, MD, K Jones, MS, S Thadiparthi, T Wang, MSPH, Div of HIV/AIDS Prevention, National Center for HIV, STD, and TB Prevention, CDC. Editorial Note:Preliminary findings described in this report suggest that programs can target testing to persons at high risk for HIV infection by enlisting persons who are HIV positive or HIV negative and at high risk to recruit NAs in their social, sexual, and drug-using networks. The approximate 6% prevalence of HIV infection among NAs tested in this project was five times the average prevalence reported by publicly funded CTR sites (5). In addition, the findings indicate that transgender and MSM recruiters were particularly effective in recruiting persons who tested positive for HIV, suggesting that transgender and MSM networks might be more likely to include persons with undiagnosed HIV infection. In this project, CBO interviewers did not ask recruiters to provide information on the specific nature of their relationship with each NA. CBO staff members reported that this contributed substantially to the willingness of recruiters to provide information about their networks and recruit NAs for CTR. Recruiters contacted most NAs themselves and, when coached and supported by CBO staff members, successfully recruited NAs for CTR. This strategy appears to make efficient use of CBO staff members, enabling them to focus on in-depth network interviews with recruiters, establishing rapport and trust, and coaching recruiters on how to effectively refer NAs for CTR. During October 2003--September 2004, CBO staff members in this project interviewed approximately three persons to identify each new case of HIV infection (133 recruiters/46 NAs). For comparison, during 2001, a survey of 22 jurisdictions indicated that health departments, on average, interviewed approximately 14 persons to identify each new case of HIV infection through PCRS (6). Cost data were collected but not analyzed for the project described in this report; further assessment of the effectiveness and cost-effectiveness of the social network strategy is needed. The findings in this report are subject to at least two limitations. First, few recruiters were enlisted who tested positive for HIV during this project and were previously unaware of their status. Whether this reflects reluctance of newly diagnosed HIV-positive clients to participate in the project or reluctance of CBO staff to suggest participation to persons who have just learned they are HIV positive is unclear. Second, data on linking newly identified HIV-positive persons to medical evaluation, care, and other services are incomplete because of difficulty in tracking and documenting referrals to other agencies. CDC guidelines recommend that HIV-positive persons be offered PCRS to identify potentially exposed partners on an ongoing basis, rather than limit such efforts to the time of initial diagnosis (7,8). In this project, most HIV-positive recruiters were not newly diagnosed; nevertheless, they were able to recruit a substantial number of NAs with a high rate of newly diagnosed HIV infection, and to do so efficiently. This finding supports the potential efficacy of working with HIV-positive persons on an ongoing basis to identify and offer CTR to others at high risk for HIV infection. However, the finding further suggests that a broader approach, which targets not only sex partners but also others in the HIV-positive person's social, sexual, or drug-using network, might be more cost-effective for identifying persons with HIV infection. Although results are preliminary, further assessment of the social network strategy is warranted. References
* San Francisco, California; Washington, DC; Orlando, Florida; Lafayette, Louisiana; Boston, Massachusetts; New York, New York; and Philadelphia, Pennsylvania. † Persons were considered at high risk for HIV if, during the preceding year, they had unprotected sex (i.e., oral, vaginal, or anal) with a person with HIV or AIDS, or a person with unknown HIV status (with or without known risk for HIV); shared drug-injection equipment; had sex in exchange for money or drugs; or had an STD. § Persons who identify with or express a gender and/or sex different from their biologic sex. Table 1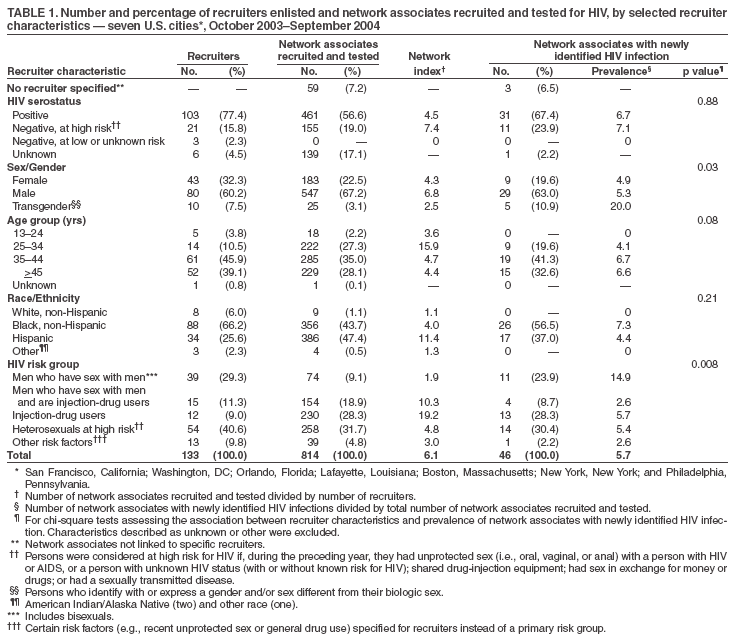 Return to top. Table 2 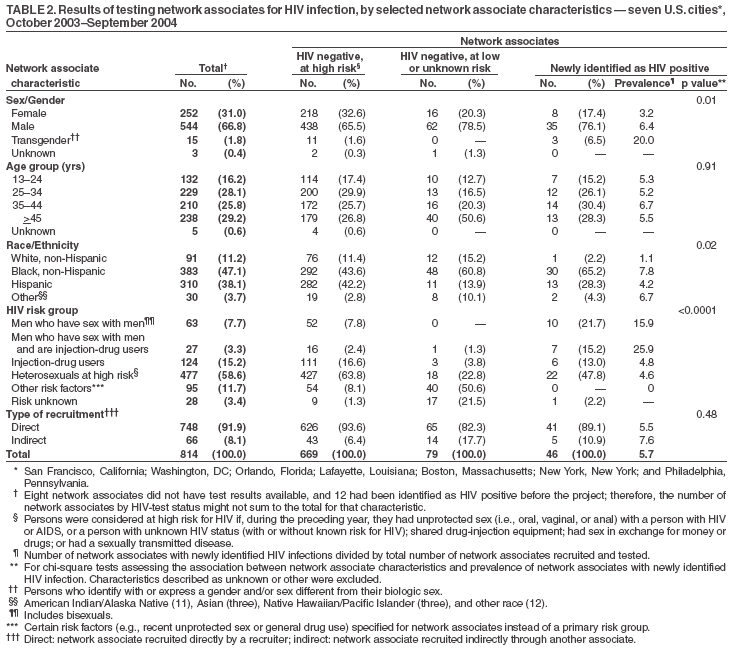 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 6/22/2005 |
|||||||||
This page last reviewed 6/22/2005
|