 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Measles --- United States, 2000In 2000, a provisional total of 86 confirmed measles cases were reported to CDC by state and local health departments, representing a record low and a 14% decrease from the 100 cases reported in each of the previous 2 years (1,2). This report describes the epidemiology of measles in the United States during 2000 and documents the continued absence of endemic measles and the continued risk for internationally imported measles cases that might result in indigenous transmission. Following state laws and regulations, health-care providers, laboratories, and other health-care personnel report confirmed measles cases to state public health departments; this information is forwarded to CDC (3). Data on vaccination status, age, complications, setting of transmission, and serologic confirmation of cases also are collected. Of the 86 reported measles cases, 26 (30%) were inter-nationally imported*. Of the 60 indigenous cases, 18 were import-linked, nine were imported virus, and 33 were of unknown source. Importation-associated cases (i.e., imported, import-linked, and imported virus cases) accounted for 62% of all reported cases. The proportion of cases classified as "internationally imported" cases has been relatively stable since 1998 (Figure 1). Of the 26 imported cases, 14 occurred in United States residents who had traveled abroad and 12 in international visitors. Measles was imported from 10 countries. The largest numbers of imported cases reported were from Japan (seven cases) and Korea and Ethiopia (four each). The states reporting the most imported measles cases were New York (eight cases), California (six), and Hawaii and Vermont (three each). Four counties had more than one imported case in 2000. On average, imported cases resulted in <1 import-linked case (range: 0--5). Measles virus was isolated from eight chains of transmission linked to an imported measles case (including three chains of one case). In each chain, the viral genotype sequenced was consistent with the genotype of virus known to be circulating in the source country of the imported case. Virologic evidence of importation was found in five chains of transmission (nine cases) that were not linked epidemiologically to imported cases. Genotype D5 was cultured from two isolated cases and genotypes G2, H1, and H2 were each isolated from one chain of transmission. These genotypes are known to circulate in Japan, China, and Vietnam, respectively. The lack of any consistently repeating genotype indicates that there is no endemic genotype. Therefore, all indigenous cases with genotype information and no epidemiologic link to an imported case were classified as imported virus cases. During 2000, a total of 20 states reported confirmed measles cases. Three states accounted for 57% of cases: New York (23 [13 from New York City]), California (19), and Nevada (seven). The remaining 17 states each reported from one to three measles cases. Of the 3,140 counties in the United States, 41 (1%) reported a confirmed measles case; seven counties (<1%) reported more than three cases. In 2000, 68 (79%) of the 86 reported cases occurred during weeks 1--26, and 18 (21%) occurred during weeks 27--52. The median number of cases per week was one (range: 0--9). During 18 weeks, no cases were reported. During 17 additional weeks, all reported cases were import-associated. During five periods of 4 weeks, all reported cases were import-associated (Figure 2). Ten cases (12% of total cases) were in infants aged <12 months, 27 (31%) in children aged 1--4 years, 17 (20%) in persons aged 5--19 years, 20 (23%) in persons aged 20--34 years, and 12 (14%) in persons aged >35 years. Of the 86 patients, 23 (27%) had a documented history of measles vaccination; 40 (46%) had not been vaccinated, nine of these were aged <12 months; and 23 (27%) patients had unknown vaccination status. Among 48 cases in persons for whom vaccine was recommended and vaccination status was known, 24 (50%) were unvaccinated. Of 71 cases in U.S. residents (57 indigenous and 14 imported), 54 (77%) occurred in vaccine-eligible persons. Of these residents, 20 (37%) were known to be vaccinated, 20 (37%) were not vaccinated, and 14 (26%) had unknown vaccination status. In 2000, 10 measles outbreaks (i.e., three or more confirmed cases) occurred in nine states accounting for 48 (56%) of the 86 cases. An epidemiologic link to an imported case was documented in five of the 10 outbreaks. The largest outbreaks occurred in New York: one in Oswego/Onondaga counties involving nine persons and a second in Kings County involving eight persons. The Oswego/Onondaga outbreak occurred in a high school; the source of infection was unknown. Of the six high school students eligible for vaccination, five had been vaccinated. Each of these students had received a single dose of measles vaccine, which was in compliance with state requirements at that time. The outbreak in Kings County occurred in a religious community in Brooklyn following an imported case from the United Kingdom. Two cases were in infants aged <12 months. Among the six patients who were vaccine eligible, three were unvaccinated. One outbreak in 2000 illustrates the difficulty in linking indigenous cases to their imported source. A U.S. resident and Olympic athlete aged 24 years developed prodromal measles symptoms while competing in an athletic event in Utah. The athlete had no known exposure to measles; however, 2 weeks before arriving in Utah, she had participated in an athletic competition in Japan. Following the competition in Utah, the athlete flew to Italy and subsequently developed a rash consistent with measles. The team physician notified CDC of the case from Italy. On return to the United States, the athlete tested IgM positive for measles. Three confirmed measles cases were linked epidemiologically to the athletic event in Utah. No viral strain was obtained from any of the cases. Reported by: M Papania, MD, S Redd, W Bellini, PhD, Div of Viral and Rickettsial Diseases, National Center for Infectious Diseases; Epidemiology and Surveillance Div, National Immunization Program; and B Lee, MD, EIS Officer, CDC. Editorial Note:Measles is still endemic in many countries and results in approximately 800,000 deaths per year (4). However, the reported incidence of measles in the United States has been <1 case per million for the past 4 years (1). The high percentage of cases resulting from importations and very limited indigenous spread from these imported cases also has continued over the same period. The consistently small number of unknown source cases suggests that measles is no longer endemic in the United States. However, unknown source cases continue to occur sporadically. Many of these cases, especially isolated cases, might be misclassifications resulting from false-positive laboratory tests. However, even among true measles cases, it is impossible to identify the imported case in every chain of transmission. The outbreak in Utah demonstrates the difficulty in linking every case to an imported source. CDC was informed of the case only because it occurred in an Olympic athlete. The case was not reported as a U.S. case because rash onset and diagnosis had occurred in Italy. If the team physician had not called from Italy to report this case, the three associated cases in Utah would have been classified as unknown source cases. Because most visits to the United States are of a relatively short duration, many persons shedding measles virus might leave the country before the rash begins and before measles is diagnosed. Many other international visitors who develop measles in the United States might choose to return home before they seek care because they are unfamiliar with the U.S. health-care system or lack valid health insurance in the United States. In both situations, the imported case would not be detected except under special circumstances. Difficulty in epidemiologically linking every case to an imported source highlights the crucial role of virologic surveillance in monitoring the absence of endemic measles. Collection of viral specimens is an important part of any measles case investigation. Worldwide, during large outbreaks (5,6) or in areas where disease is endemic (7,8), one measles genotype is usually found. Since 1992 in the United States, no genotypes have been found consistently, and when genotypic data are available, all isolates from imported cases have the genotype found in the country of origin (5,9). Imported measles cases consistently test the level of population immunity to measles in the United States. The average of less than one import-linked case following an international importation suggests that the level of population immunity is high, probably as a result of successful vaccination efforts in the United States. First-dose vaccination coverage among preschool children has been >90% for the past 4 years (10). Two doses of measles vaccine are required for school-aged children in 49 states (CDC, unpublished data, 2002). Sustaining high levels of vaccination is important in limiting indigenous spread of measles from imported cases and preventing measles from becoming re-established as an endemic disease in the United States. Acknowledgement This report is based on data contributed by state and local health departments. References
* Imported=cases among persons who were infected outside the United States; Indigenous=cases in persons infected in the United States. Indigenous cases are subclassified into three groups: import-linked=cases epidemiologically linked to an imported case (virologic evidence of importation is not required for this classification); imported virus=cases that cannot be linked epidemiologically to an imported case but for which imported virus has been isolated from the case or from an epidemiologically linked case; and unknown source=all other cases acquired in the United States for which no epidemiologic link or virologic evidence has been found to indicate importation. Figure 1  Return to top. Figure 2 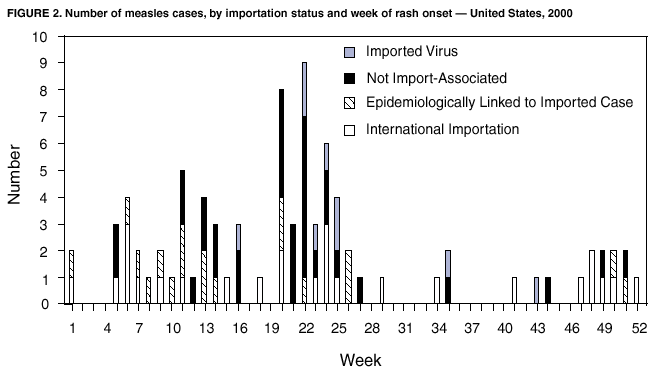 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 2/14/2002 |
|||||||||
This page last reviewed 2/14/2002
|