 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Prenatal Discussion of HIV Testing and Maternal HIV Testing -- 14 States, 1996-1997In July 1995, the Public Health Service recommended that health-care providers counsel all pregnant women about human immunodeficiency virus (HIV) prevention and encourage testing for HIV infection (1) and, if indicated, initiate zidovudine therapy (2). To evaluate compliance with these recommendations, CDC analyzed population-based data on HIV counseling and testing during 1996-1997 from 14 states participating in the Pregnancy Risk Assessment Monitoring System (PRAMS). This report presents an analysis of survey data collected from 1996 through 1997; results indicate that HIV counseling and testing of pregnant women were common but varied by state, type of prenatal health-care provider, Medicaid status, and maternal demographic characteristics. PRAMS is an ongoing, state-based surveillance system that collects information about maternal behaviors, attitudes, and experiences. Each month, PRAMS surveys a random sample of mothers who have given birth to live infants during the previous 2-6 months using stratified, systematic sampling of resident birth certificates. A questionnaire is mailed to each mother, and a follow-up questionnaire is mailed to nonrespondents. Nonrespondents then are contacted by telephone. Statistical weights are applied to account for sampling probability, nonresponse, and sampling frame coverage in each state. The annual state-specific response rate to the entire questionnaire for 11 states in 1996 and 13 states in 1997 was approximately 70% (range: 69.4%-80.0%). Details of the survey design, questionnaire, and other operational aspects of the survey have been published (3). Beginning in 1996, mothers who received prenatal care were asked whether a doctor, nurse, or other health-care provider counseled them about testing for HIV. Mothers in eight states, regardless of whether they received prenatal care, were asked if they had been tested for HIV infection during pregnancy or at delivery. Mothers who received any prenatal care and responded to the provider test discussion question were included in the analysis (n=17,354 [97.4%] in 1996; n=19,693 [98.1%] in 1997). To analyze maternal HIV testing, data were included on all mothers who responded to the HIV testing question regardless of having received prenatal care (n=8420 [89.8%] in 1996; n=11,152 [91.0%] in 1997). To account for the complex survey design, SUDAAN was used to calculate point estimates, risk ratios, and 95% confidence intervals (CIs) surrounding the risk ratios. State-specific risk ratios were considered significant if the 95% CI did not include 1. State-specific risk ratios are not presented for sparse data (response categories with less than 20 women). During 1997, the state-specific proportion of mothers who recalled discussing HIV testing with their prenatal health-care provider ranged from 63.4% (Maine) to 86.7% (North Carolina), and the proportion of mothers who recalled being tested ranged from 58.0% (Oklahoma) to 80.7% (Florida) (Figure 1). Among 10 states with data from 1996 to 1997, increases in testing discussions occurred in New York (22.8%), Oklahoma (17.8%), and West Virginia (15.3%). Seven states demonstrated no increases (range: -2 to 0.9%) in prenatal testing discussions. The largest increase in reporting of maternal testing from 1996 to 1997 occurred in New York (18.1%). Smaller increases occurred in West Virginia (15.2%), Florida (14.3%), Oklahoma (11.5%), and Georgia (6.5%). During 1997 in all states, black mothers were significantly more likely than white mothers to report that their provider discussed testing (risk ratio [RR]=1.05-1.29). Hispanic mothers were not significantly more likely to report having had a testing discussion in most states. In seven states, mothers with less than a high school education were significantly more likely (RR=0.96-1.22) to recall a discussion about testing. Similarly, in 11 states, mothers aged less than 25 years were significantly more likely to recall a discussion about testing (RR=1.04-1.25). Public health-care providers were more likely than private providers to discuss testing (RR=0.96-1.29) in 10 states. In 11 states, mothers who received Medicaid benefits during pregnancy were significantly more likely to report discussions with a health-care provider (RR=0.99-1.32). In most states, black race, type of prenatal health-care provider, education level, age, and receipt of Medicaid benefits were associated significantly with maternal HIV testing. However, associations between maternal characteristics and testing discussions were stronger than associations between maternal characteristics and actual testing. Reported by: Pregnancy Risk Assessment Monitoring System Working Group, Div of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion; Div of HIV/AIDS-Surveillance and Epidemiology, National Center for HIV, STD, and TB Prevention, CDC. Editorial Note:Editorial Note: This report documents a substantial level of counseling about HIV testing and receipt of testing for women who have given birth since publication of the 1995 guidelines. In 1997, greater than 70% of women in nine states recalled discussing HIV testing with their health-care provider during prenatal care, and at least 50% of women in all states reported being tested for HIV during pregnancy or at delivery. Data from PRAMS suggest that physician practices regarding prenatal HIV testing discussions and prenatal maternal HIV testing may be influenced by state-specific variations in HIV seroprevalence rates among childbearing women and physician perceptions of maternal HIV risk factors. Health-care providers serving women in states with high HIV seroprevalence rates may be more aware of HIV prevention and may place higher priority on prenatal HIV prevention. For example, on average, fewer mothers (69.2%) in low HIV seroprevalence states (HIV seroprevalence rate among pregnant women less than 0.05%) recalled a discussion about testing compared with mothers (81.4%) in high seroprevalence states (seroprevalence rate greater than 0.4%) (4). Maternal HIV testing demonstrated a similar association; fewer mothers (58.0%) in low seroprevalence states were tested compared with mothers (70.9%) in high seroprevalence states. Variations in testing discussions by maternal race, age, and Medicaid status may reflect targeted testing efforts by providers on the basis of known epidemiology of HIV among women in their area. In addition, perception of the mother's risk may influence whether a provider discusses HIV testing. Differences in state legislation also may contribute to variations in HIV discussions and testing. During 1996, Florida and New York enacted legislation requiring that all health-care providers include HIV counseling during prenatal care. High levels of provider discussions on HIV testing reported in Washington and North Carolina can be attributed to legislation mandating this activity before 1996. In July 1997, Arkansas law required that providers test all pregnant women for HIV; however, that legislation probably did not affect results presented in this report. An association among legislation, discussions, and actual HIV testing cannot be established using PRAMS data (5). Another survey has shown increased test counseling for women who were young and other than white, sought care from a public provider, and had low incomes (6). PRAMS data also are consistent with a provider survey that found variations in prenatal test counseling according to provider type (i.e., public versus private) and type of patient insurance (i.e., Medicaid versus other) (7). The findings in this report are subject to at least four limitations. First, information about previous HIV testing among mothers and the testing date, if any, were not available. Second, the wording of the survey questions did not allow consideration of a cause-effect relationship between provider test counseling and maternal test acceptance. Third, information was not collected on maternal risk for HIV infection, context of test counseling (i.e., strength of provider encouragement), or reasons a mother refused testing. Finally, data were not available to estimate self-reported information accuracy; however, most respondents completed the questionnaire within 4 months of the infants' delivery, minimizing recall bias. Data from this survey permit health-care professionals and policymakers to monitor ongoing health-care provider counseling and maternal testing. The results described in this report emphasize the need for increasing health-care providers'-- especially private sector providers'--awareness of HIV testing during prenatal care to ensure that health-care providers counsel all pregnant women. References
Figure 1 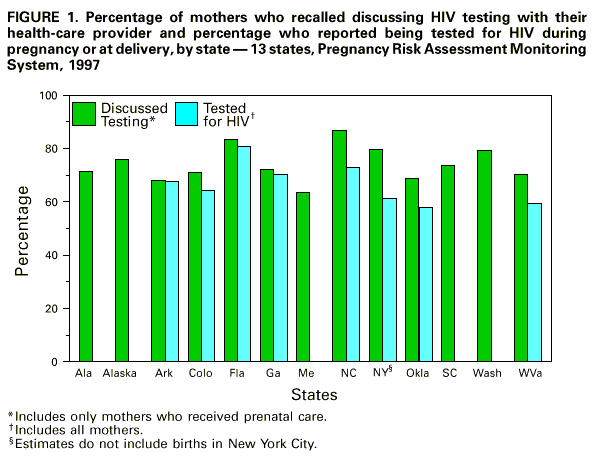 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 5/20/99 |
|||||||||
This page last reviewed 5/2/01
|